Background: Insulin was first licensed for human use in 1922. Since then, numerous formulations with various similar names have been produced and marketed. Because the names of the different drugs are often very similar (novolin vs novalog) it can difficult for emergency providers to keep all of the agents straight. In this post, we discuss the categories of insulins, the nomenclature and the pharmacokinetics of the most commonly used agents.
Thank you to the St. John’s pharmacy students for their incredible work in compiling the information shared below.
Insulin Categories
- Rapid Acting – AnaLOGs
- Aspart, lispro, glulisine
- Short Acting
- Regular (NovoLIN or HumuLIN)
- Intermediate Acting
- NPH, protamine combined
- Long Acting (Basal)
- Glargine (Lantus), detemir (Levemir)
Insulin Nomenclature
- Novo Products – Novo Nordisk company
- Hum Products – Eli Lilly company
- Suffixes
- Log – Rapid acting (i.e. NovoLog, HumaLog)
- Lin R – Short acting (NovoLin R, HumuLin R)
- Lin N – Intermediate acting (NovoLin N, HumuLin N)
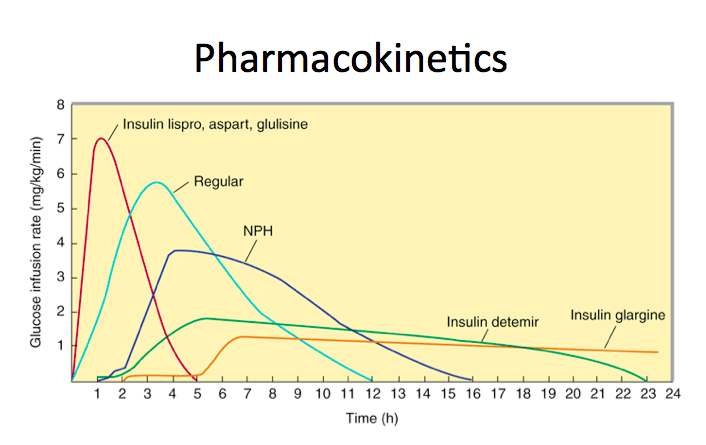
| Insulin Name | Onset | Peak | Duration |
| Rapid Acting | |||
| Lispro (Humalog) | < 15 minutes | 0.5 – 3 hours | 3-5 hours |
| Aspart (Novolog) | < 15 minutes | 0.5 – 3 hours | 3-5 hours |
| Glulsine (Apidra) | < 15 minutes | 0.5 – 3 hours | 3-5 hours |
| Short Acting | |||
| Regular (Novolin R or Humulin R) | 0.5 – 1 hour | 2-4 hours | 4-8 hours |
| Intermediate Acting | |||
| NPH (Novolin N or Humulin N) | 2-4 hours | 4-10 hours | 10-18 hours |
| Long Acting | |||
| Glargine (Lantus) | 4-6 hours | Same action throughout the day | 24 hours |
| Detemir (Levemir) | 2-3 hours | 6-8 hours | Dose dependent (5.7 – 23.3 hours) |
| Combinations | |||
| Hululin or Novolin 70/30 | 0.5 – 1 hour | 2-10 hours | 10-18 hours |
| Novolog Mix 70/30, Humalog Mix 75/25 or 50/50 | < 15 minutes | 1-2 hours | 10-19 hours |
Reasons for Hypoglycemia in Patients on Insulins
- Caloric intake inadequate for insulin dose
- Reduced intake, increased exercise, catabolic stress (infection, myocardial infarction etc.)
- Decreased gluconeogenesis
- Reduced insulin elimination
- Insulins primarily renal excreted
- Patients with CKD, ESRD or AKI at risk for reduced elimination
- Increased insulin dose
- Unintentional (medication error)
- Intentional (self harm, homicide)
Disposition
- Regular Insulin – short acting enough for ED observation + discharge home
- Kinetics of large insulin overdose unpredictable – admit to high monitored setting

excellent. short, concise and directed.
It’s also given IV associated with TPN
should regular insulin be given IV or SC?
Depends on indication. In DKA, regular insulin IV. Same for hyperkalemia treatment. Otherwise, SQ/SC is just fine