Definition: Inflammation of the partial and/or visceral layers of the pericardium surrounding the heart. The inflammation is characterized by lymphocytes and granulocytes infiltrating the pericardium.
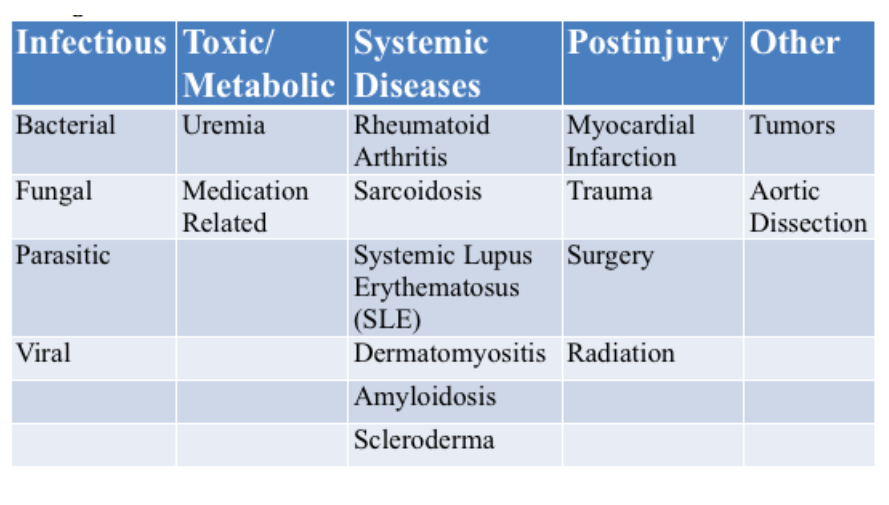
Etiologies
Presentation
- Symptoms
- Chest Pain
- Typically sharp and pleuritic
- Improved with sitting or leaning forward
- Increased with lying down
- May radiate to the trapezius muscles
- Fever
- Myalgias
- Chest Pain
- Exam Findings
- Pericardial Friction Rub
- Occurs from friction between the sliding of the inflamed visceral pericardium against the parietal pericardium or of the parietal pericardium against the pleura
- Friction rubs are intermittent and often inaudible when present in the ED due to ambient noise
- Pericardial Effusions
- Variably present and are often small
- Significant effusions more commonly seen in uremic pericarditis
- Pericardial Friction Rub
Diagnosis
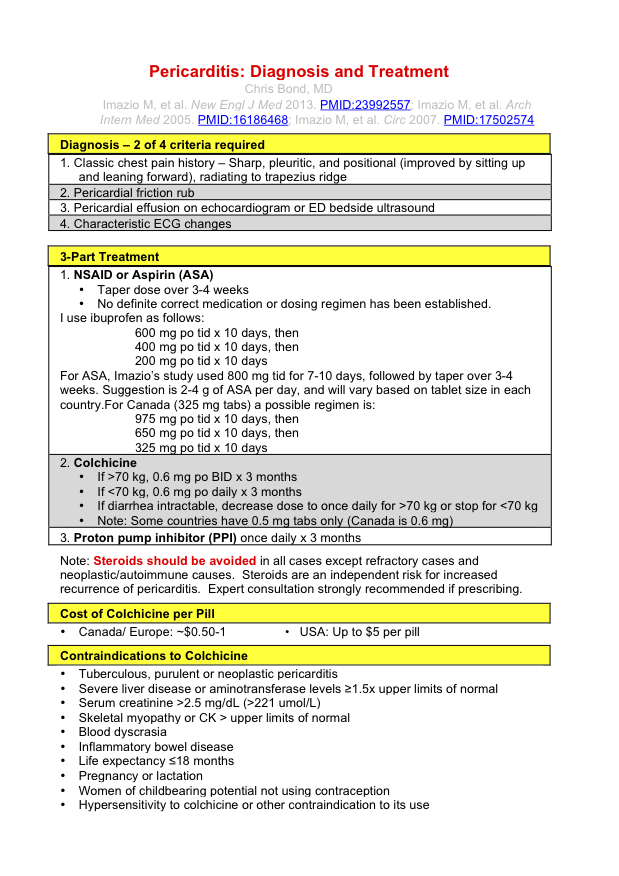
- Diagnostic Criteria (2 out of 4 required)
- Classic chest pain history: sharp, pleuritic and positional with radiation to the trapezius ridge
- Pericardial friction rub
- Pericardial effusion on echocardiogram
- Characteristic EKG findings
- EKG Findings
- EKG is a reliable diagnostic tool. However, EKG changes occur in stages over time and classic findings may not be present depending on the duration of symptoms
- Caution: Acute ST segment elevation myocardial infarction (STEMI) is often be mis-diagnosed as pericarditis
- The first step in diagnosis of pericarditis should be to think about and eliminate STEMI as the diagnosis
- Excellent review of the differences from the ECG Case of the Week
- STEMI ST elevations are convex
- Patients may have concomitant T wave inversions with the ST elevations
- Reciprocal changes (ST depressions) are commonly seen
- Repeat EKGs may show dynamic changes and development of Q waves
- Inferior and inferolateral STEMI easily confused for pericarditis
- Non-concave up morphology specific for STEMI (Brady 2001)
- Any ST depression in aVL sensitive and specific for STEMI (Bischof 2015)
- Stage 1
- Occurs over hours to days
- Characterized by diffuse ST elevations
- Morphology: Concave upwards
- May see ST depression in aVR and V1
- Should NOT see reciprocal ST depressions (indication that patient has a STEMI)
- PR segment depression
- Spodik’s Sign: Downsloping of the TP segment (Spodick 1976)
- Stage 2
- ST and PR segments normalize
- T waves flatten and then transition to deep, symmetrical T wave inversions
- Stage 3 – resolution
- ST and PR segment changes resolve
- T wave inversions may persist indefinitely
- Laboratory Studies
- No lab test has a high enough sensitivity or specificity to either rule-in or rule-out pericarditis or differentiate it from MI
- White blood counts: Can be elevated due to stress from MI
- Troponin: Can be elevated in MI as well as in myopericarditis or myocarditis
- Cardiac Ultrasound
- Small pericardial effusions are often seen in patients with pericarditis
- Patients with pericarditis should not have focal wall motion abnormalities (commonly seen in STEMI)
Pericarditis EKGs
Medical Management (See Clinical Card)
- Non-Steroidal Antiinflammatory Drugs (NSAIDs) or Aspirin
- Both NSAID and aspirin should be tapered over 3-4 weeks
- Optimal regimen unknown
- Ibuprofen
- 600 mg PO Q8 X 10 days, then
- 400 mg PO Q8 X 10 days, then
- 200 mg PO Q8 X 10 days
- Aspirin
- 800 mg Q8 X 7-10 days followed by taper (Imazio 2013)
- Sample Schedule (In US, 325 mg ASA available)
- 975 mg PO Q8 X 10 days, then
- 650 mg PO Q8 X 10 days, then
- 325 mg PO Q8 X 10 days
- Colchicine
- If > 70 kg: 0.6 mg PO Q12 X 3 months
- If < 70 kg: 0.6 mg PO Q24 X 3 months
- Contraindications: Liver disease, Renal insufficiency/failure (Cr > 2.5 mg/dl), Myopathies, Blood dyscrasia, Inflammatory bowel disease, Pregnancy or lactation, women of childbearing age not using contraception.
- Proton Pump Inhibitor: PO Q24 hours X 3 months
- Corticosteroids
- Should not be prescribed from the ED as 1st line therapy as they increase the risk of recurrence
- Frequently used in treatment of patients with autoimmune pericarditis
Disposition
- Most patients with pericarditis can be treated as outpatients with close follow up
- Patients with concern for myocarditis or myopericarditis should be considered for admission. Tachycardia out of proportion to pain/fever and significant troponin elevations may be seen in these disorders (Imazio 2007)
- Patients with large pericardial effusions should be considered for admission to follow change in size and for consideration of pericardiocentesis (diagnostic or therapeutic) (Imazio 2007)
Take Home Points
- Always consider STEMI as the diagnosis prior to diagnosing pericarditis. If the the EKG shows convex ST elevations, reciprocal ST depressions or dynamic changes, the patient is much more likely to have a STEMI.
- Patients with pericarditis should be treated with a combination of NSAID/Aspirin and Colchicine
- Patients with large pericardial effusions, tachycardia out of proportion to fever/pain and troponin elevations are more likely to have complicated courses and should all be considered for admission
ECG Case of the Week (Amal Mattu): Acute STEMI vs. Pericarditis Part 1 + Part 2
REBEL EM: Colchicine for Treatment of Pericarditis
SOCMOB: Pericarditis: Treatment and Diagnosis Pocket Card
FOAMcast: Episode 54 – The Pericardium
Pericarditis PV Card (Chris Bond (socmob.org)
Brady W et al. Electrocardiographic ST-segment elevation: the diagnosis of acute myocardial infarction by morphologic analysis of the ST segment. Acad Emerg Med 2001;8:961–7. PMID: 11581081
Bischof JE et al. ST depression in lead aVL differentiates inferior ST-elevation myocardial infarction from pericarditis. Am J Emerg Med 2015 PMID: 26542793
Spodick D. Differential characteristics of the electrocardiogram in early repolarizations and acute pericarditis. NEJM 1976;295(10):523–6. PMID: 950958
Imazio M et al. A randomized trial of colchicine for acute pericarditis. NEJM 2013; 369(15): 1522-8 PMID: 23992557
Imazio M et al. Indicators of poor prognosis of acute pericarditis. Circulation 2007; 115(21): 2739-44. PMID: 17502574




Very systematically written and easy to grasp. Would be helpful for exams. It would be of great help if all this could be in PDF format so that I could save it. Thank you