Definition: A cesarean section preformed either during maternal cardiac arrest or during impending maternal cardiac arrest the primary goal of which is to increase the chance of successfully resuscitating the mother and, potentially, improving fetal survival.
Physiological Changes in Late Pregnancy
- Blood volume and cardiac output increase by 30-40% above the nonpregnant state by 28 weeks
- This hypervolemic state is protective for the mother, as fewer red cells are lost during hemorrhage
- Clinical signs of maternal shock manifest only after 40% of maternal blood volume is lost
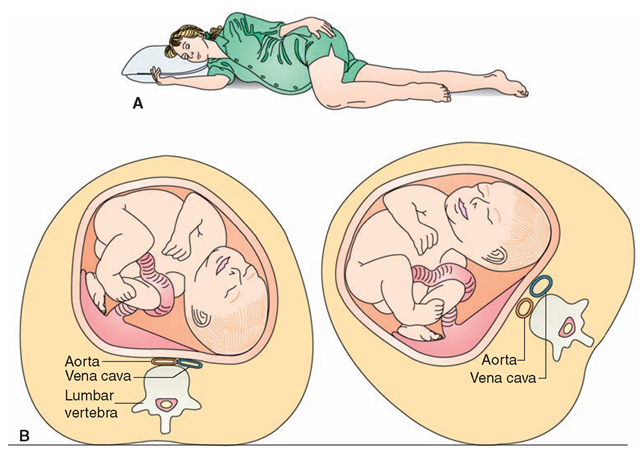
- Late pregnancy is very susceptible to hypotension from compression of the inferior vena cava (IVC) in the supine position by the enlarged uterus
- The enlarged uterus causes elevation of the diaphragm by about 4 cm, and results in a decrease in the functional residual capacity by about 20%
General approach to the pregnant trauma patient
- Overall same general approach as in non-pregnant patients. Focus must always be on resuscitating the mother, not the fetus.
- Special considerations in primary survey
- Airway: There is physiologic narrowing of the upper airways in the third trimester
- Use an endotracheal tube 1 size smaller.
- Intubation medications are the same.
- RSI is the preferred method of intubation for any indication in the third trimester due to the increased risk of aspiration.
- Breathing: Pregnant patients are predisposed to rapid falls in Pa02 during apnea
- Supplemental O2 should be provided for any pregnant patient being resuscitated regardless of saturation.
- Circulation: Hypovolemia should be suspected before clinical signs of hypotension in trauma patients, as the state of hypervolemia and resulting hemodilution may mask underlying significant blood loss.
- Aggressive volume resuscitation is encouraged regardless of blood pressure.
- Resuscitation of the pregnant patient should include uterine displacement to relieve compression of the IVC and thus improve cardiac output and restore circulation.
- Perform in any patient in whom the uterus could potentially cause compression regardless of gestational age or lack of knowledge of gestational age.
- Traditional teaching: This can be done by tilting the backboard up a 30 degree angle to the left, but may be difficult to perform effective chest compressions while patient tilted
- New model: It is more effective to manually move the uterus to the patient’s left with one or two hands during ongoing chest compressions, while patient remains flat on their back.
- Airway: There is physiologic narrowing of the upper airways in the third trimester
Purpose of Peri-Mortem C-Section (PCS):
- Primary goal is improvement of maternal, not fetal, resuscitation
- PCS decreases uterine compression on the IVC thus increasing venous return, resulting in improved maternal cardiac filling pressure.
- PCS also allows for improved respiratory mechanics, as the diaphragm is lowered after the procedure
When to perform a PCS:
- Traditional teaching: perform a PCS at 24 weeks in a peri-arrest or arresting mother, as a fetus is generally
considered viable at 24 weeks gestational age.
- At 24 weeks gestation, there is a 20-30% chance of extrauterine fetal survival if neonatal facilities are available.
- New model: PCS is resuscitative hysterotomy for the mother
- 24 week guideline is flawed
- You will likely not have this information in this clinical setting.
- Even the best ultrasound dating criteria is subject to 1-2 weeks of uncertainty.
- PCS is primarily resuscitative for mother – best chance of saving the fetus is to save the mother.
- Counter argument to new model: before 24 weeks gestation, the fetus is small and PCS will not have significant effect on maternal hemodynamics.
- Alternate guide to perform PCS
- There is a reported gestational age anywhere near viability
- The abdomen is large, specifically if fundal height is above umbilicus
- If baby looks big on ultrasound (may not have time to measure biparietal diameter, but can get a general sense of the size of the fetus)
- 24 week guideline is flawed
How long after arrest do you have to perform a PCS?
- Perform a PCS as soon as possible after maternal cardiac arrest.
- After 4 minutes of maternal arrest there is a precipitous decline in fetal neurologic outcome and survival.
- Despite decreased utility after 4 minutes for fetal survival, resuscitative hysterotomy will continue to hold benefits to the mother.
How to perform a PCS:
- Make a vertical incision from xiphoid to the pubis using a scalpel (ideally #10 Blade)
- Cut through subcutaneous tissue to get to peritoneal wall
- Use fingers to bluntly dissect to the peritoneum
- Cut through peritoneum vertically (ideally with scissors or use a scalpel to initiate an opening inferiorly)
- Deliver the uterus, then cut into the lower half of the uterus vertically to avoid the placenta and then use scissors to extend the incision upwards until you reach the baby
- Deliver the baby (neonate will likely need resuscitation)
- Clamp and cut the umbilical cord
- Place packing/towels in the opened uterus and abdomen
Below is a short blast talk on the Peri-Mortem C-Section from Core EM Faculty Salil Bhandari
Take home points:
- Think of PCS as a resuscitative hysterotomy primarily aimed at saving the life of the mother
- If you think PCS will improve maternal resuscitation, act quickly to start and complete the procedure
- The optimal surgical approach for a PCS is via a large vertical incision.
References
Ramanathan S, Porges RM. Anesthetic Care of the Injured Pregnant Patient. In Capan LM, Miller SM, Turndorf H Editors, Trauma Anesthesia and Intensive Care; J.B. Lippincott Company; 1991; 599-628.
Pimentel L. Mother and Child: Trauma in Pregnancy. Emerg Med Clin North Am. 1991 Aug;9(3):549-63. PMID: 2070767
Drost TF, Rosemurgy AS, Sherman HF, Scott LM, Williams JK. Major Trauma in Pregnant Women: Maternal/fetal Outcome. J Trauma. 1990 May;30(5):574-8. PMID: 2342141
Vanden Hoek TL, Morrison LJ, Shuster M, et al. Part 12: cardiac arrest in special situations: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S829. PMID20956228
O’Connor RL, Sevarino FB. Cardiopulmonary arrest in the pregnant patient: a report of a successful resuscitation. J Clin Anesth. 1994;6(1):66. PMID 8142104
Cordero DR, Toffle RC, McCauley CS. Cardiopulmonary arrest in pregnancy: the role of caesarean section in the resuscitative protocol. W V Med J. 1992;88(9):402. PMID: 1462532
Additional resources:
EMCrit: Peri-Mortem C-section
St. Emlyn’s: Peri-mortem C-section
JAMIT: Perimortem Caesarian Section
Should you continue CPR after the C-Section?
Yes. The C-section will hopefully improve venous return and increase the efficacy of your CPR.
Is it requires any type of anaesthesia?
Patients requiring peri-mortem c-section are typically in extremis and likely do not need much if anything in the way of anesthesia. Obviously, I’d be very cautious about any systemic medications that may drop BP.
if we have to give anaesthesia, which drugs should we prefer?
This article is missing the key step of delivering the placenta. Don’t just clamp/cut and stuff, manually scoop the placenta off the uterine wall. With regards to maternal survival, the placenta is sucking up a huge amount of O2 and it’s not until the placenta is detached from the uterus that this stops and her SpO2 will pop up to improve outcomes.