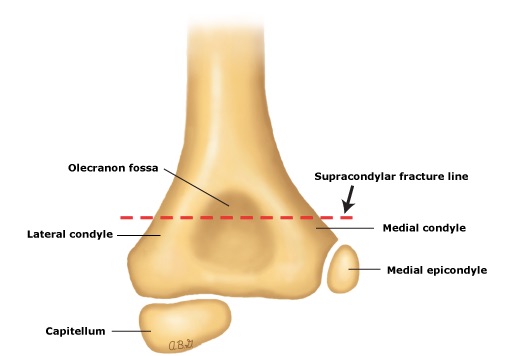
Pediatric Elbow Anatomy
Definition: Fracture of the distal humerus above the level of the epicondyles
Mechanism
- Indirect: Fall onto outstretched and hyperextended upper extremity
- Direct (less common)
- Direct trauma to the elbow
- Fall onto a flexed elbow or from object striking the elbow
- Direct trauma to the elbow
Epidemiology
- Comprise of 55-75% of all elbow fractures (Egol 2010)
- Male predominance
- Peak incidence between 5-8 years of age after which dislocation is more frequent

S-Shaped Deformity (Brubacher 2008)
Physical Exam
- Patients will present with a swollen, tender elbow with painful range of motion
- S-shaped Deformity: Occurs when the fracture is completely displaced at the distal humerus
- Pucker Sign
- Puckering, dimpling, or ecchymosis of the skin anterior to the distal humerus
- Indicates that the proximal fragment has penetrated the brachialis muscle (Brubacher 2008)
- A thorough neurovascular exam must be performed
- Neuropraxis is common (Egol 2010)
- Anterior Interosseous Branch of the Median Nerve Neurapraxia
- Most Common associated nerve injury
- Unable to flex the interphalangeal joint of the thumb and the distal interphalangeal joint of the index finger (can’t make an A-OK sign)
- Radial Nerve Neurapraxia: inability to extend wrist or digits
- Ulnar Nerve Neurapraxia: inability to abduct or adduct fingers
- Anterior Interosseous Branch of the Median Nerve Neurapraxia
- Neuropraxis is common (Egol 2010)
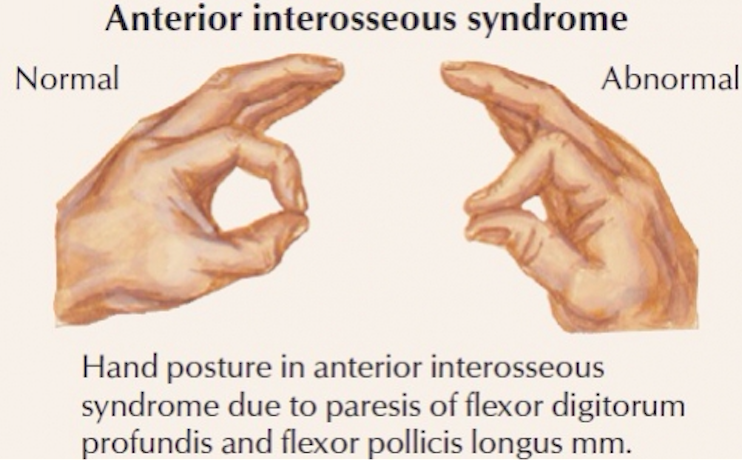
Anterior Interosseous Syndrome (jcphysiotherapy.com)
- Vascular Injury
- Results from direct injury to the brachial artery or secondary to antecubital swelling
- Can lead to Volkmann’s Contracture: permanent flexion contracture of the hand at the wrist secondary to obstruction of the brachial artery.
Fractures Types
- Extension type injuries represent 98% of supracondylar humerus fractures
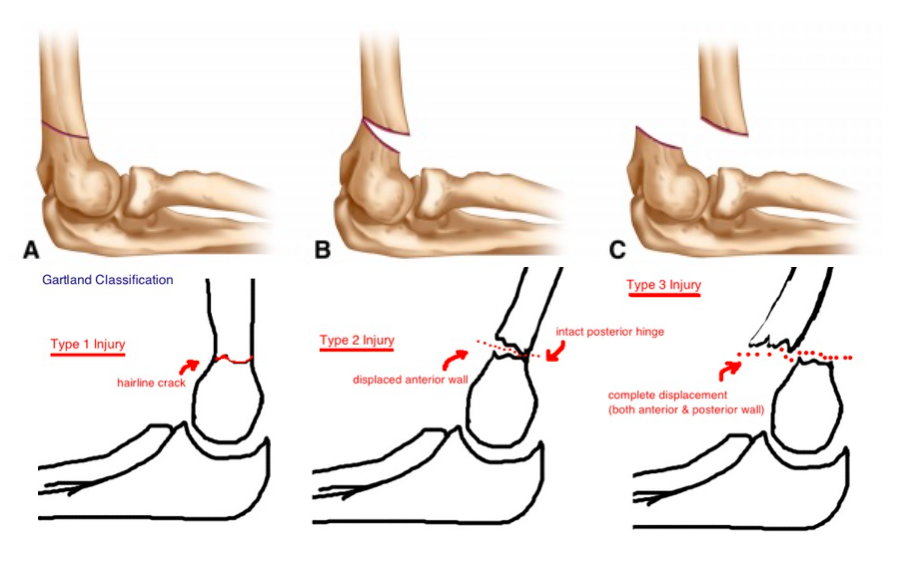
- Gartland Classification of Supracondylar Fractures
- Based on the degree and direction of displacement, and the presence of an intact cortex (Alton 2015)
- Type1: Minimal displacement – fat pad elevation on radiographs
- Type2: Posterior hinge – anterior humeral line anterior to capitellum
- Type3: Displaced – no cortices intact
- Type4: Periosteal disruption with instability in both flexion and extension
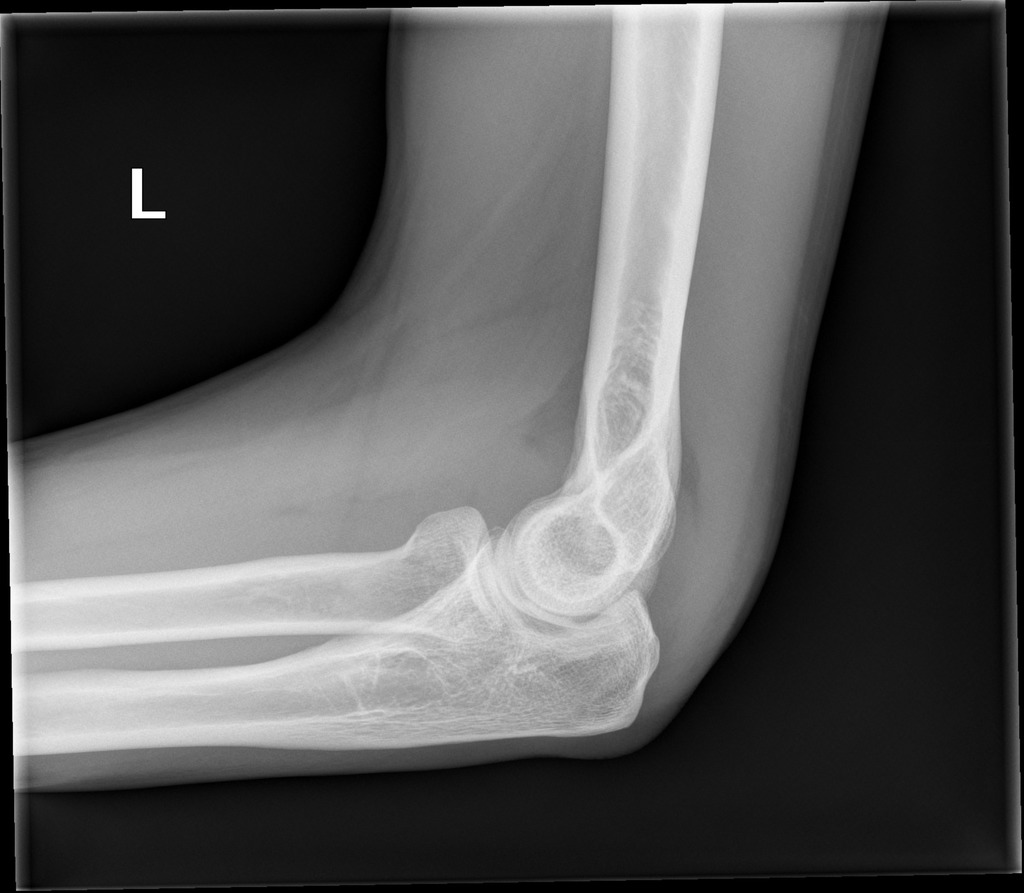
Presence of Posterior and Anterior Fat Pad Signs (Case courtesy of Dr Bruno Di Muzio, Radiopaedia.org. From the case rID: 45115)
Diagnostic Imaging
- Always obtain AP and lateral radiographs
- Occult Fractures
- Clear fractures often absent on plain radiographs
- Look for indirect evidence of fracture
- Anterior Fat Pad Sign (“Sail Sign”)
- The presence of a small anterior fat pad can be a normal finding
- Elevation of the anterior fat pad (abnormal) is secondary to a joint effusion
- Posterior Fat Pad Sign
- Presence of a lucent crescent located in the olecranon fossa
- Presence of posterior fat pad is always pathologic.
- Anterior Humeral Line
- In an elbow with normal anatomic alignment, a line drawn down the anterior surface of the humerus should cross the middle third of the capitellum
- If this line is disrupted, it suggests an occult supracondylar fracture
- Anterior Fat Pad Sign (“Sail Sign”)
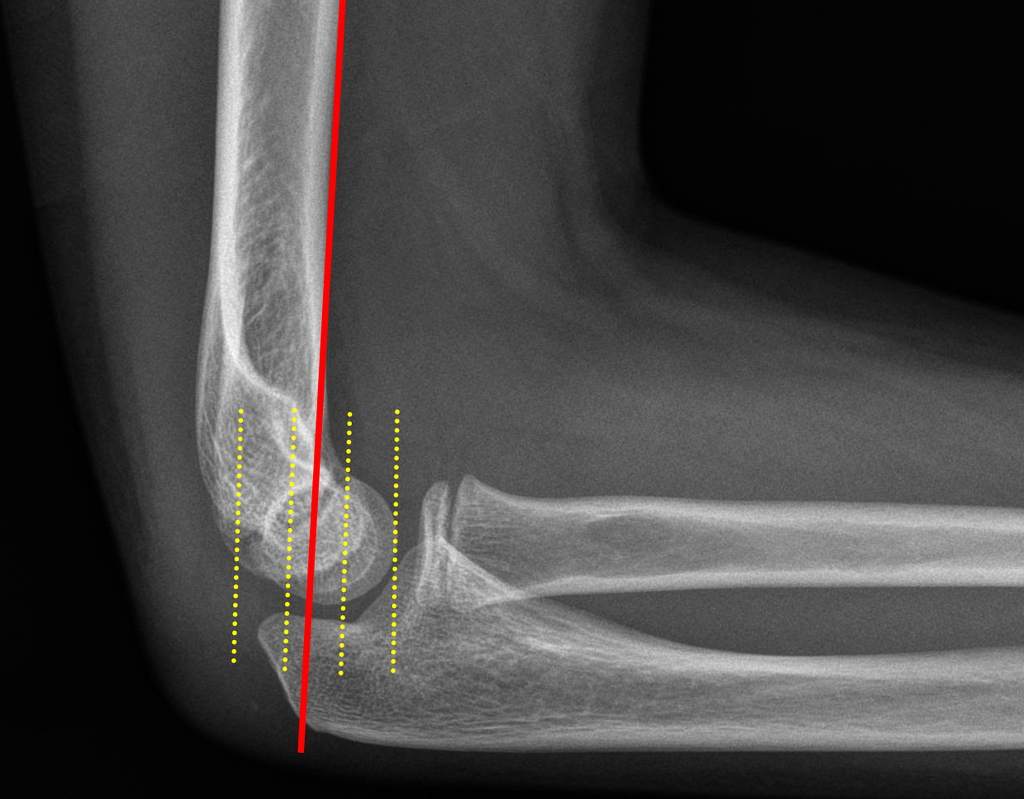
Normal Anterior Humeral Line (Case courtesy of Dr Benoudina Samir, Radiopaedia.org. From the case rID: 41167)
ED Management
- Assess for secondary injuries as with any other trauma patient
- Gartland Type1 Fractures
- Long arm posterior splint
- Elbow in 90 degrees of flexion
- Forearm in neutral position
- Orthopedic follow-up in one week for likely operative management
- Long arm posterior splint
- Gartland Type2/3 Fractures
- Immediate orthopedic consultation in order to determine appropriate intervention (closed versus open reduction with percutaneous pin placement)
- Gartland 2/3 fractures have higher likelihoods of occult neurovascular injury and thus residual deformity
- Closed reduction and percutaneous pinning is the preferred treatment for displaced fractures (Brubacher 2008)
- Other indications for immediate consultation
- Open fractures
- Presence of neuromuscular compromise
- Evidence of compartment syndrome
Prognosis
- Long-term outcomes of supracondylar humeral fractures are good; however, there is potential for long-term pain, ulnar nerve sensitivity, and decrease in grip in Type2/3 fractures (Sinikumpu 2016)
- Most complications from supracondylar humeral fractures are neurapraxias which require no treatment (Egol 2010)
Take Home Points
- Supracondylar humeral fractures may often present without evidence of fracture lines on diagnostic imaging. Always assess for indirect signs of fractures.
- Do not forget to conduct a thorough neurovascular exam as supracondylar fractures can be associated with neurapraxias, vascular injuries, and compartment syndrome.
- Type1 fractures can be splinted and discharged with close orthopedic follow-up; Type2/3 fractures generally require immediate orthopedic consultation.
Read More
Orthobullets: Supracondylar Fracture – Pediatric
References
Egol KA et al. Handbook of Fractures. Lippincott Williams & Wilkins; 2010. Link
Brubacher JW, Dodds SD. Pediatric supracondylar fractures of the distal humerus. Curr Rev Musculoskelet Med. 2008;1(3-4):190-6. PMID: 19468905
Alton TB, Werner SE, Gee AO. Classifications in brief: the Gartland classification of supracondylar humerus fractures. Clin Orthop Relat Res. 2015;473(2):738-41. PMID: 25361847
Sinikumpu JJ et al. The long-term outcome of childhood supracondylar humeral fractures: A population-based follow up study with a minimum follow up of ten years and normal matched comparisons. Bone Joint J. 2016; 98-B(10):1410-1417. PMID: 27694598
very informative
Agree with Yusuf. Very informative.
Informative