This post is cross-posted on REBEL EM here.
Definition: Bacterial infection of the hip joint space and synovial fluid
Background
- Causes
- Hematogenous spread in bacteremia
- Local spread (i.e. from osteomyelitis)
- Direct inoculation (traumatic or surgical)
- High-Risk Subgroups
- Age < 2 years (peak incidence 6 – 24 months)
- Immunocompromised state (i.e. AIDS, active CA etc)
- Functional asplenia (i.e. sickle cell disease)
- Complications
- Sepsis
- Osteomyelitis
- Chronic arthritis
- Osteonecrosis
- Capsule damage
Differential Diagnosis (for atraumatic hip pain)
- Transient Synovitis
- Septic Arthritis
- Osteomyelitis
- Legg-Calve-Perthes (LCP) Disease
- Slipped Capital Femoral Epiphysis (SCFE)
Presentation
- Varies greatly based on age group
- Infants: fever, failure to feed, lethargy, pain with handling
- Older children
- Fever (absent in up to 20% of patients)
- Non-specific symptoms: malaise, poor appetite, irritability
- Joint pain and/or swelling
- Pain is typically acute in onset (unlike in osteomyelitis)
- Look for pain with passive range of motion
- Often limb held in abduction, flexion and external rotation which increases joint space
- Gait abnormality
- New limp
- Refusal or difficulty with bearing weight
Causative Pathogen
- S. aureus is the most common causative organism across age groups
- Birth – 2 months
- Group B Streptococci
- N. gonorrhoeae
- E. coli
- > 2 months
- S. pneumoniae
- S. pyogenes
- K. kingae (more common in immunocompromised state)
- H. influenzae (less prevalent in areas of high vaccination rate)
- Other agents to consider in specific populations
- Salmonella in sickle cell disease (S. aureus still the most common in this group)
- N. gonorrhoeae in sexually active patients and if polyarticular involvement
Septic Arthritis vs. Toxic Synovitis
- Toxic synovitis
- Definition: A benign, self-limited inflammation of the hip joint
- Symptoms mimic septic arthritis (atraumatic, fever, inability to bear weight/new limp and acute onset of pain)
- Treatment: anti-inflammatories and follow-up
- Kocher Criteria (Kocher 1999, Kocher 2004)
- Approach to differentiating septic arthritis from toxic synovitis
- Consider application to pediatric patients with an acute irritable hip where both of these diagnoses are considered
- Criteria (each is worth 1 point)
- Non weight-bearing
- Temp > 101.3oF (38.5oC)
- ESR > 40 mm/hr
- WBC > 12,000 cells/mm3
- Caveat: Though Kocher criteria is the most studied decision tool, it is far from perfect. A Kocher score of 0 does not rule out the disease (Caird 2006) but a positive screen should heighten suspicion
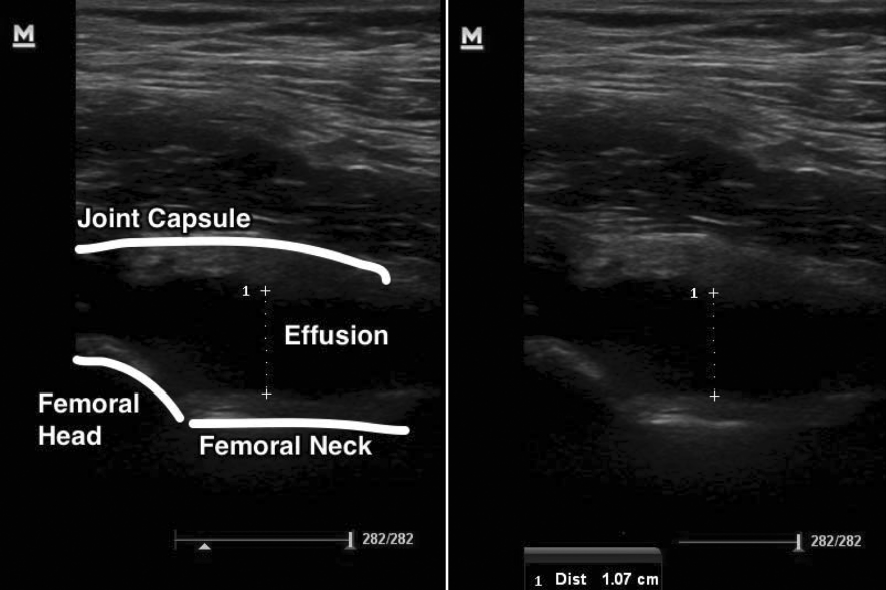
Ultrasound Hip Effusion (Plumb 2015)
ED Management
- Unstable/Toxic patient
- In toxic patient with hip pain and fever, treat as sepsis of any other cause
- Resuscitate with crystalloids
- Start empiric antibiotics
- Obtain expert consultation for source control
- Imaging
- Ultrasound to confirm presence of effusion as absence greatly decreases (but does not eliminate) risk of septic arthritis
- If US negative but continued suspicion, can obtain MRI
- Imaging should not delay orthopedic consultation
- Stable/Non-toxic Patient
- Provide analgesia and antipyretics immediately
- This is both therapeutic and diagnostic
- Well appearing child who is ambulating after an NSAID is less concerning for septic arthritis
- Often, when the decision is difficult, orthopedics will want to know the patient’s response to analgesia
- Obtain X-rays of hip to assess for alternate pathology (fracture, oseomyelitis, LCP, SCFE) and for presence of effusion
- Laboratory tests
- CBC for white blood cell count
- Erythrocyte sedimentation rate (ESR)
- Blood cultures (positive in 20-50% of cases)
- Apply Kocher criteria
- 0 predictors
- Very low risk for septic arthritis
- Consider management with observation alone
- 1 predictors
- Low risk (3%) of septic arthritis
- Consider imaging or orthopedics consultation
- 2 predictors
- Moderate risk for septic arthritis (40%)
- Hip aspiration via ultrasound or fluoroscopy
- > 3 predictors
- Very high risk for septic arthritis (>93%)
- Consider aspiration in the OR
- 0 predictors
-

Ultrasound Guided Hip Aspiration (Plumb 2015)
Arthrocentesis
- Ideally performed with either fluoroscopy or ultrasound for guidance (Plumb 2015)
- Fluid Findings
- Findings overlap with other possible etiologies making interpretation difficult
- Likely turbid
- WBC Count: 10,000 – 250,000
- PMNs > 75%
- Elevated lactate
- Antimicrobial Management
- Provide analgesia and antipyretics immediately
|
Age |
Agent 1 |
Agent 2 |
Additional Considerations |
| Birth – 2 months | Nafcillin 50 mg/kg | Cefotaxime 50-75 mg/kg | |
| > 2 months of age | Nafcillin 50 mg/kg | Ceftriaxone 50 mg/kg | Consider adding vancomycin 10 mg/kg if concern for MRSA |
Editor’s Note: While some resources suggest nafcillin as first line, many clinicians opt for vancomycin in all patients since the prevalence of MRSA has increased dramatically in recent years.
Take Home Points
- Septic arthritis of the hip can be a difficult diagnosis to make. Consider it in all patients with hip pain or limp and fever.
- In toxic appearing patients with hip pain/new inability to bear weight and fever, do not delay orthopedic consultation for imaging or labs. Source control in the OR is paramount.
- No single test can rule in or out septic arthritis of the hip. Apply the Kocher criteria to help risk stratify patients but be aware of the limitations of this decision tool.
- Always administer analgesics and antipyretics as appropriate response can help decrease the likelihood of septic arthritis.
Read More
ALiEM: Transient Synovitis vs. Septic Arthritis of the Hip
Peds EM Morsels: Septic Arthritis
MD Calc: Kocher Criteria for Septic Arthritis
McQullen KK: Musculoskeletal Disorders, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 176: p 2250-2270.
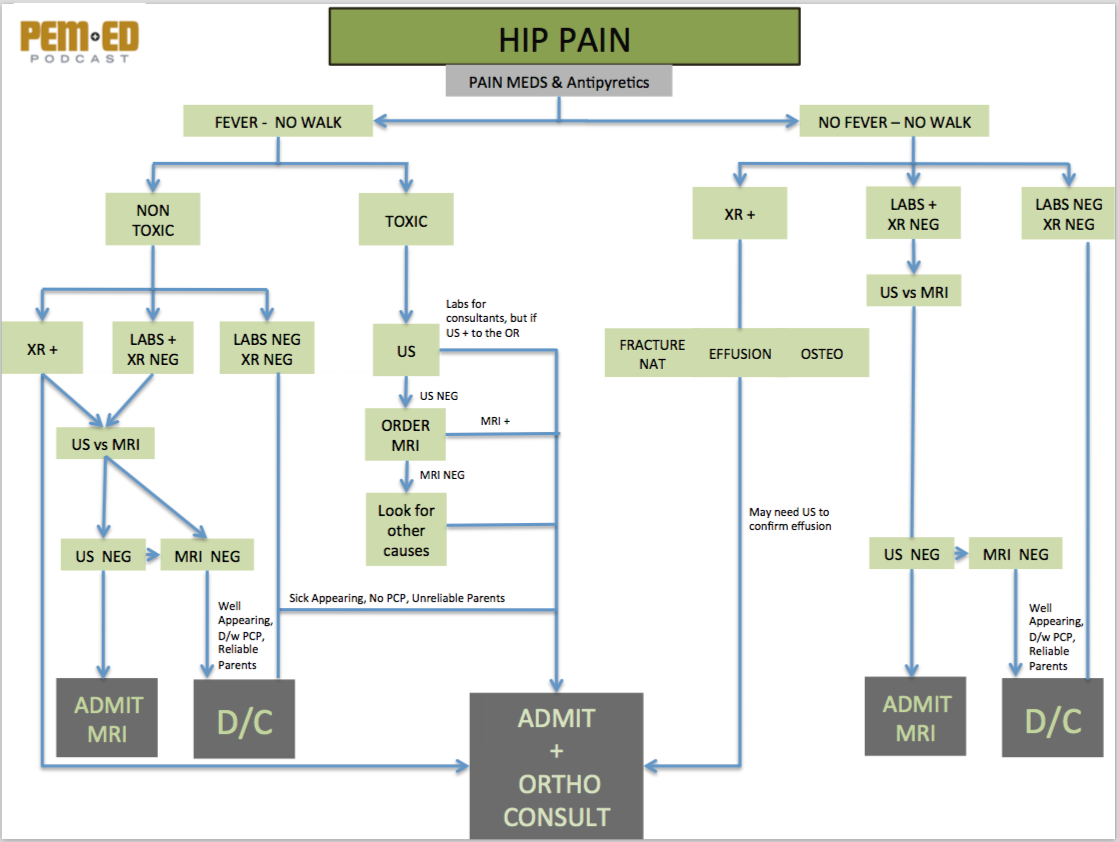
Hip Pain Diagnostic Algorithm (PEM ED)
References
Kocher MS et al. Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction algorithm. J Bone Joint Surg Am 1999; 81(12): 1662-70. PMID: 10608376
Kocher MS et al. Validation of a clinical prediction rule for the differentiation between septic arthritis and transient synovitis of the hip in children. J Bone Joint Surg Am 2004; 86-A(8): 1629-35. PMID: 15292409
Caird M et al. Factors distinguishing septic arthritis from transient synovitis of the hip in children. A prospective study. J Bone Joint Surg Am. 2006; 88(6):1251-1257. PMID: 16757758
Plumb J et al. The role of ultrasound in the emergency department evaluation of the acutely painful pediatric hip. Pediatric Emerg Care 2015; 31: 54-61. PMID: 25560622
