BACKGROUND
- More than 500,000 annual emergency department visits and 60,000 hospitalizations for pediatric patients with TBI in the United States (Chen, Int J Environ Res Public Health. 2018., PubMed ID: 29874782)
- Most head trauma is minor, but it is crucial to identify patients with clinically important traumatic brain injury who require further evaluation and management
- CT scans are associated with significant ionizing radiation, which may be harmful to the developing brain (Brenner, NEJM 2007, PubMed ID: 18046031)
- Always consider non-accidental trauma
CLINICAL EVALUATION
- History should include (S)AMPLE history as well as details about the trauma (mechanism) and high-risk symptoms (loss of consciousness, vomiting, headache, behavioral changes, worsening of symptoms).
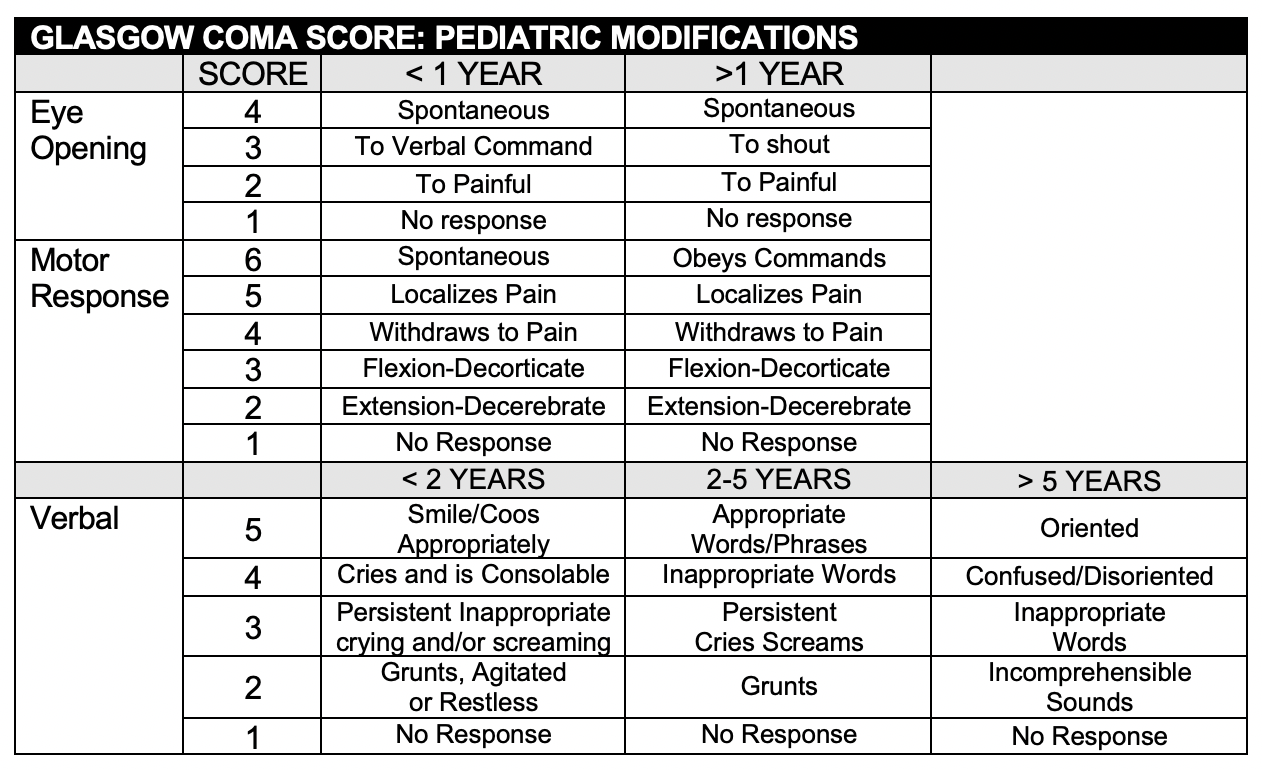
- Physical exam should include a full trauma evaluation where indicated, with specific focus on GCS, mental status, and signs of skull fracture and increased ICP
- Pediatric GCS can be difficult to assess in preverbal patients (see below)
RADIOLOGIC EVALUATION
- Multiple clinical decision rules have been derived and validated to identify pediatric clinically important traumatic brain injury
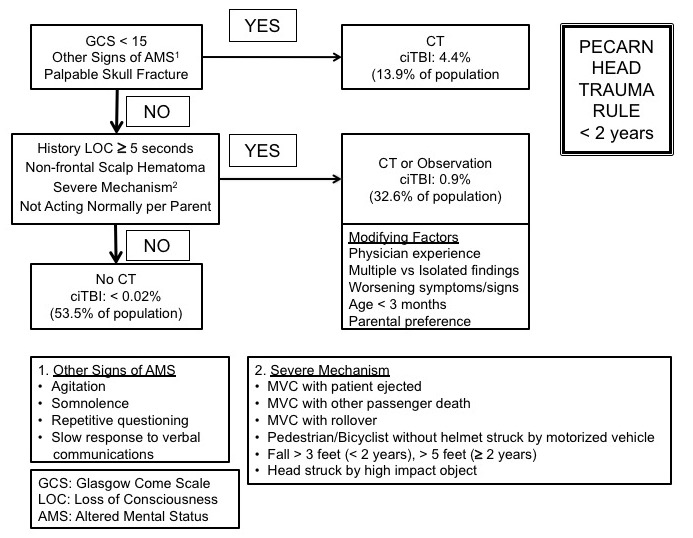
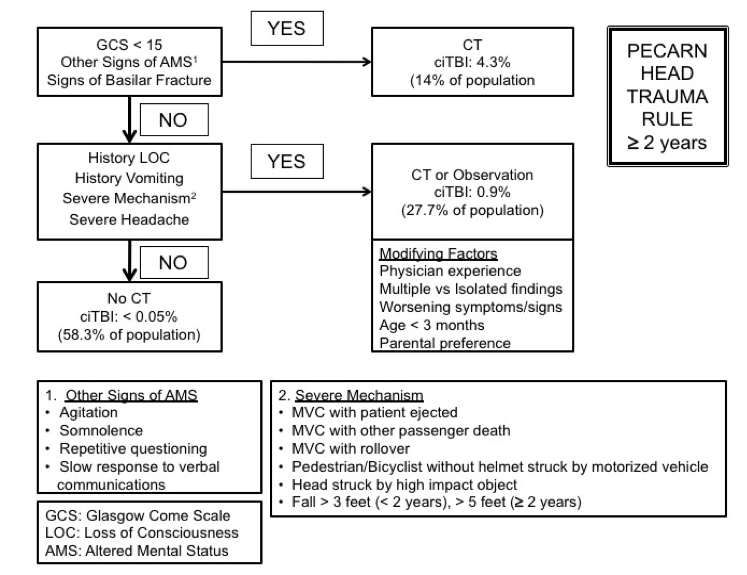
- The PECARN head trauma rule is most frequently utilized in the U.S. (Kupperman, Lancet 2009, PubMed ID: 19758692 , MD CALC)(See below)
- Patients with trivial head trauma and a GCS 14 were excluded
- In an analysis including combined age groups and both the derivation and validation sets 1 in 5,000 with clinically important traumatic brain injury could be missed (high predictive value of a negative test)
- Potential to decrease CT usage
- Rules for < 2 years and > 2 years with specific event, history and physical exam factors associated with clinically important traumatic brain injury.
- Other pediatric head trauma clinical decision tools include the Canadian CATCH rule (MD CALC) and U.K. CHALICE (MD CALC) rule.
- Recent studies suggest the rapid MRI may be an attractive alternative to CT (Ramgopol, BMC Pediatrics 2020, PubMed ID: 31931764, Sheridan, J Neurosurg Pediatr. 2016, PubMed ID: 27885947).
MANAGEMENT
- ABCs take priority, as in all trauma patients
- Management includes maintaining adequate cerebral perfusion pressure, as well as addressing increased intracranial pressure (elevating head of bed, analgesics and sedation, osmotic agents)
- Anticonvulsants should be considered in patients with intracranial abnormalities (e.g. Keppra; recommended dose varies)
- Neurosurgical consult should be called for any patients with abnormal CT findings
DISPOSITION
- Most patients can be discharged after either a period of observation or after initial evaluation
- Patients with intracranial abnormalities should be managed in conjunction with neurosurgical consultants
- The CHILDA Score can be used to determine the need for ICU admission (Greenberg, JAMA Pediatrics, PubMed ID: 28192567)
REFERENCES
Kuppermann N, Holmes JF, Dayan PS, Hoyle JD, Atabaki SM, Holubkov R, Nadel FM, Monroe D, Stanley RM, Borgialli DA, Badawy MK, Schunk JE, Quayle KS, Mahajan P, Lichenstein R, Lillis KA, Tunik MG, Jacobs ES, Callahan JM, Gorelick MH, Glass TF, Lee LK, Bachman MC, Cooper A, Powell EC, Gerardi MJ, Melville KA, Muizelaar JP, Wisner DH, Zuspan SJ, Dean JM, Wootton-Gorges SL., Pediatric Emergency Care Applied Research Network (PECARN). Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet. 2009 Oct 03;374(9696):1160-70. PMID: 19758692
Martin H Osmond, Terry P Klassen, George A Wells, Rhonda Correll, Anna Jarvis, Gary Joubert, Benoit Bailey, Laurel Chauvin-Kimoff, Martin Pusic, Don McConnell, Cheri Nijssen-Jordan, Norm Silver, Brett Taylor, Ian G Stiell, Pediatric Emergency Research Canada (PERC) Head Injury Study Group. CATCH: a clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ , 182 (4), 341-8, 2010 Mar 9. PMID: 2831681
J Dunning, J Patrick Daly, J-P Lomas, F Lecky, J Batchelor, K Mackway-Jones, Children’s head injury algorithm for the prediction of important clinical events study group. Derivation of the Children’s Head Injury Algorithm for the Prediction of Important Clinical Events Decision Rule for Head Injury in Children. Arch Dis Child, 91 (11), 885-91, Nov 2006. PMID:17056862
Greenberg JK, Yan Y, Carpenter CR, Lumba-Brown A, Keller MS, Pineda JA. Development and Internal Validation of a Clinical Risk Score for Treating Children with Mild Head Trauma and Intracranial Injury. JAMA Pediatr. 2017 Apr 1;171(4):342-349. PMID: 28192567
Borgialli, Dominic A.; Mahajan, Prashant; Hoyle, John D.; Powell, Elizabeth C.; Nadel, Frances M.; Tunik, Michael G.; Foerster, Adele; Dong, Lydia; Miskin, Michelle; Dayan, Peter S.; Holmes, James F.; Kuppermann, Nathan; Walthall, Jennifer (2016). Performance of the Pediatric Glasgow Coma Scale Score in the Evaluation of Children With Blunt Head Trauma. Academic Emergency Medicine (8): 878-884. PMID: 27197686
