
Knee Anatomy (anatomynote.com)
Definition: Rupture of the patellar tendon (tendon attaching patella to tibial tubercle) with or without associated fracture.
Mechanism
- Overload of the extensor mechanism complex (quadriceps, quadriceps tendon, patella, patellar tendon, tibial tubercle)
- More likely to occur with knee flexed to 60 degrees, given most force on tendon at this angle (Matava 1996)
Epidemiology
- Uncommon injury: < 1% US population per year (Volpi 2016)
- Gender: Males > Females
- Age: 20s and 30s most commonly
- More often unilateral, but bilateral patellar tendon rupture has been documented (Matava 1996)
- Predisposing Factors (Volpi 2016)
- Previous surgery
- Patellar tendinopathy
- SLE
- Rheumatoid arthritis
- Chronic renal failure
- DM
Physical Exam
- Loss of extensor mechanism (ability to extend at knee joint)
- Hemarthrosis, swelling, tenderness
- Palpable defect inferior to patella
- Patella alta (elevation of patellar height)
- Inability of unassisted weight bearing (Volk 2014)
Injury Classification
- Partial tendon rupture – Extensor mechanism intact
- Complete tendon rupture – Loss of extensor mechanism
- Tendon avulsion from inferior pole of patella
- May include bony fragment when associated patellar fracture (McMahon 2014)
- Mid-tendon rupture
- Tendon avulsion from tibial tubercle
- May include bony fragment when associated tibial tubercle fracture
- Tendon avulsion from inferior pole of patella
- Xrays
- Trauma knee series: AP, lateral, obliques and can consider sunrise/tunnel views if indicated
- Xray cannot visualize tendon, but may provide other evidence of tendon rupture as shown below

Patella Alta (Case courtesy of Radiopaedia.org. From the case rID: 11743)

Patellar Tendon Rupture with Avulsion of Tibial Tubercle (medscape.com)
- Ultrasound
- Can aid in diagnosis at bedside using longitudinal view from inferior patella to tibial tuberosity
- Normal tendon structure can be identified as multiple parallel echogenic lines
- Rupture can be identified as a hypoechoic break with surrounding edema
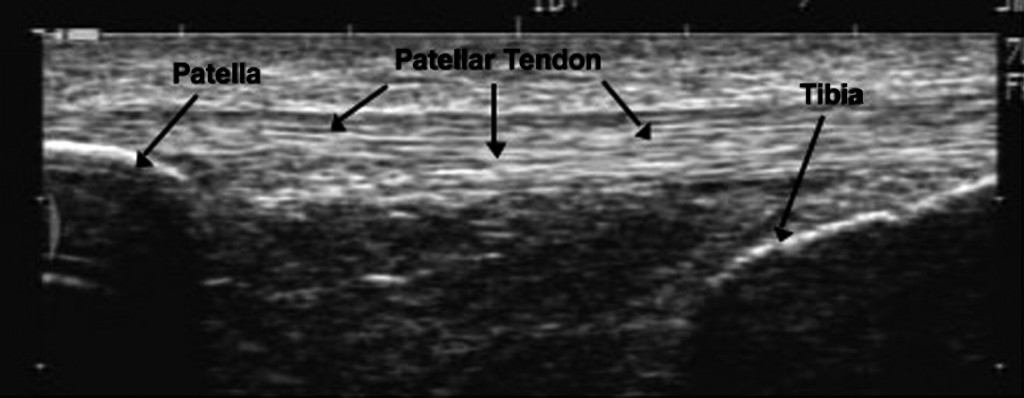
Patellar Tendon US Normal (drandyfranklynmiller.com)
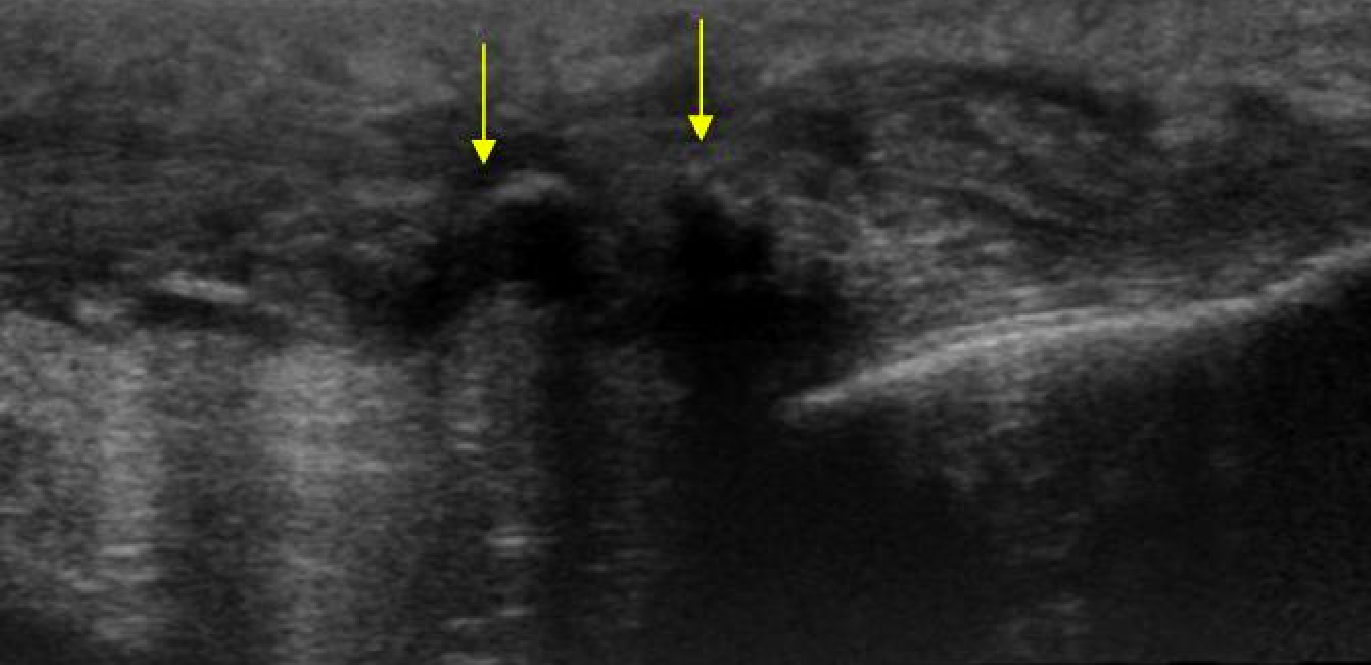
Ruptured Patellar Tendon (www.ultrasoundcases.info)
- MRI
- Gold standard for diagnosis
- Usually unnecessary in ER and can be obtained as out-patient if needed
Emergency Department Management
- Partial tendon rupture
- Usually treated non-operatively
- Knee immobilizer and crutches (non-weight bearing in immediate period)
- Orthopedic follow up – graded weight bearing as tolerated for 3-6 weeks (Khan 2005)
- Complete tendon rupture
- Usually treated with operative repair
- Prompt follow up necessary (within 1 week)
- Non-weight bearing with knee immobilizer and crutches
- Shorter time to surgical repair was associated with better outcomes of recovery – lower incidence of quadriceps weakness and incomplete knee flexion (Matava 1996)
- Indications for immediate Orthopedic consultation
- Any associated fracture (e.g. tibial plateau, patellar)
- Pediatric population
- Sleeve fractures are often missed due to cartilaginous tendon attachment in children
- Expected non-compliance with knee immobilization or non-weight beating status
Prognosis
- For partial tendon rupture, rehabilitation length depends on severity of tear with complete recovery by 6 months
- For complete tendon rupture, non-restricted activity usually resumes at 4-6 months with complete recovery between 6-12 months (Vopli 2016)
Take Home Points
- Loss of extensor mechanism is a key part of the knee exam and indicates complete disruption of the patellar tendon (or quadriceps tendon)
- All patients with patellar tendon rupture should have their knee immobilized, be initially non-weight bearing and follow up promptly with Orthopedics
- Missed diagnoses and delay of surgical repair can lead to worse outcomes
References
Khan KM et al. Patellar Tendinopathy and Patellar Tendon Rupture. In: Maffulli N., Renström P., Leadbetter W.B. (eds) Tendon Injuries. 2005. Springer, London (Link)
Matava M. Patellar Tendon Ruptures. J Am Acad Ortho Sure 1996; 4(6): 287–296. PMID: 10797196
McMahon, Patrick J., et al (2014). “Chapter 3. Sports Medicine.” Current Diagnosis & Treatment in Orthopedics, 5e Eds. Harry B. Skinner, and Patrick J. McMahon. New York, NY: McGraw-Hill.
Volk WR et al. Complications in Brief: Quadriceps and patellar tendon tears. Clin Orthop Relat Res 2014; 472(3): 1050-7. PMID: 24338040
Arthroscopy and Sport Injuries : Applications in High-Level Athletes, edited by Piero Volpi, Springer, 2015. ProQuest Ebook Central. Link