Pacemaker Terminology
- Five letter code system that describes the different pacemaker settings
- First three letters are most useful in ED management
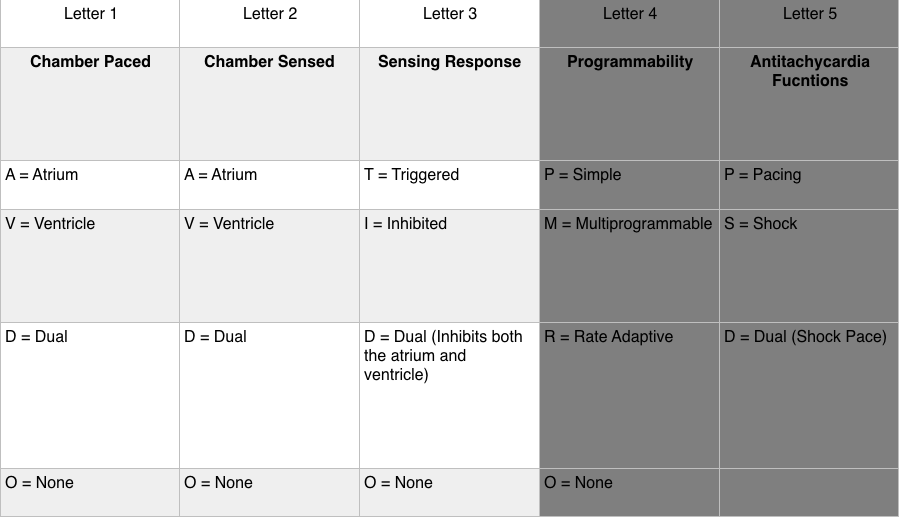
- Sensing Response
- Triggered (T): Sensed intrinsic depolarization will result in the pacemaker discharging (this setting not used in current generation pacemakers)
- Inhibited (I): Sensed intrinsic depolarization will result in inhibition of the pacemaker
- Dual (D): Dual inhibition of both atrial and ventricular pacing in response to intrinsic ventricular depolarization
- None (O): Does not trigger or inhibit regardless of the native activity
- Example #1: DDD
- Chamber paced: Atrium and ventricle can be paced
- Chamber sensed: Intrinsic depolarization of the atrium and ventricle is sensed
- Sensory response: Can inhibit pacemaker in response to an intrinsic ventricular depolarization OR trigger pacemaker in response to an atrial intrinsic depolarization with no associated ventricular response
- Example #2: VVI
- Device has a single lead in the ventricle that senses ventricular activity and can pace the ventricle
- An atrial event outside the refractory period will be inhibited
Common Indications for Permanent Pacemaker Placement
- Sinus node dysfunction: symptomatic sinus bradycardia, frequent/prolonged sinus pauses, impaired response to demand/exercise
- 3rd degree or advanced 2nd degree (Mobitz II) AV block with any of the following
- Symptomatic bradycardia
- Ventricular dysrhythmia resulting from AV block
- Symptomatic bradycardia secondary to necessary drugs for dysrhythmia management
- Symptomatic bradycardia resulting from 2nd degree AV block
- Chronic bifascicular or trifascicular block with intermittent 3rd degree or 2nd degree AV block
- Exertional 2nd or 3rd degree AV block
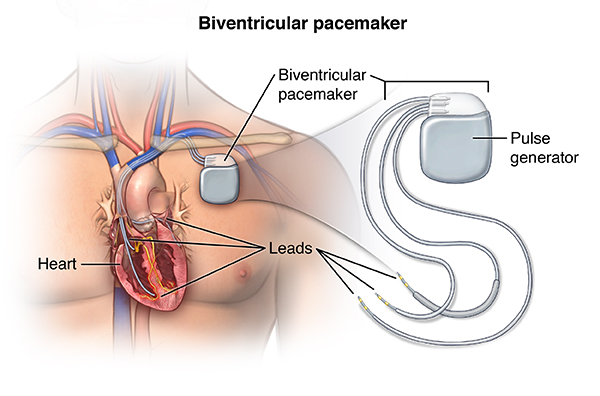
Biventricular Pacing (spectrumhealth.com)
Pacemaker Components
- Pulse Generator
- Houses power source (almost always lithium battery)
- Battery duration: 4-10 years (depends on features of device)
- Power decreases gradually with lithium battery; no abrupt cessation of activity
- Electronic Circuitry
- Leads
- Single lead: endocardial lead positioned in contact with right ventricle
- Dual lead: endocardial lead positioned in contact with right atrium and right ventricle
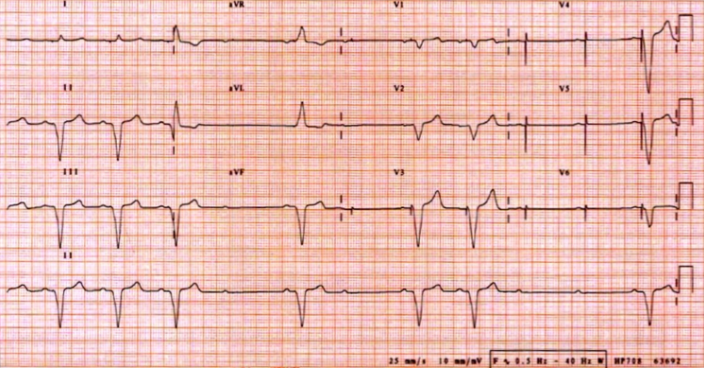
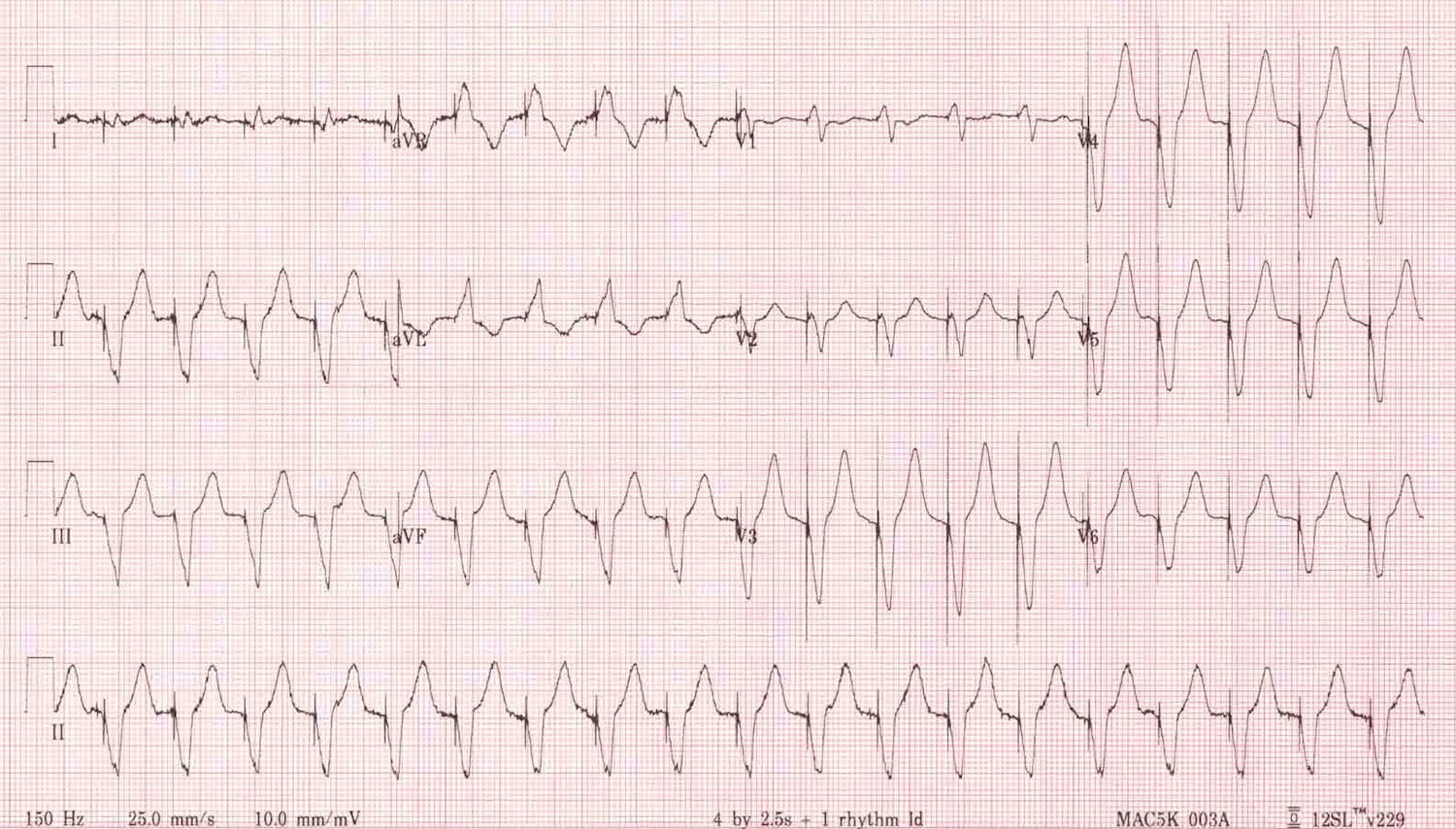
Sample Normal EKGs
- EKG appearance depends on type of pacemaker in use
- Single Ventricular Lead
- Narrow “spike” represents pacemaker generated electrical stimulus
- Followed by LBBB formation QRS complex
- Note: RBBB formation signifies lead displacement
- Dual Chamber Pacing
- Two narrow “spikes” seen representing an atrial stimulus (1st spike) and ventricular stimulus (2nd spike)
- First spike results in atrial depolarization. Second spike results in ventricular depolarization
- Ventricular response variable
- Narrow QRS
- Conducted from intrinsic atrial activity
- Conducted from pacemaker generated atrial spike via the AV node
- Atrial spike conducted through AV node and generates QRS
- Wide QRS
- Generated by ventricular lead stimulus
- Narrow QRS
- Absence of paced complexes in a patient with a pacemaker does not always indicate pacemaker dysfunction. It may reflect adequate native conduction and, thus, inhibition of the pacemaker
Normal Functioning Pacemaker EKGs

Pacemaker Pocket Infection (researchgate.com)
Complications
- Infectious Complications
- Rare
- Pocket infection: 2%
- Bacteremia: 1%
- Signs/Symptoms: warmth, swelling, erythema, pain, fever
- Blood cultures: (+) in 20-25% of patients (commonly S. Aureus, S. epidermidis)
- Can result in pacemaker pocket erosion
- Treatment
- IV antibiotics (i.e.vancomycin)
- Needle aspiration: should only be performed under fluoroscopy to avoid cutting components of the device
- Cardiology consultation for removal and replacement
- Rare
- Thrombophlebitis
- Common complication (30-50% with some venous obstruction) (Kucher 2011)
- Symptoms
- Occur in only 0.5 -3.5% of patients due to collateralization
- Pain, swelling, venous engorgement of the ipsilateral arm
- Diagnostic Testing: Duplex sonography
- Treatment: Anticoagulation
- Pacemaker Syndrome
- Definition
- Loss of AV synchrony and loss of atrial “kick”
- Occurs when there is intact sinus node function but atria contract with tricuspid/mitral valves closed (i.e. during ventricular systole)
- Symptoms: Syncope/Near-syncope, orthostatic dizziness, exercise intolerance, generalized weakness, palpitations
- Treatment: replacement of single chamber pacemaker to dual chamber pacemaker
- Definition
Pacemaker Manufacturer
- In order to interrogate a pacemaker, the device manufacturer must be known
- The majority of the time, this information can be determined from the medical record or, the patient will carry a device manufacturer card with all of the information
- Algorithm to determine manufacturer using X-ray (Jacob 2011)
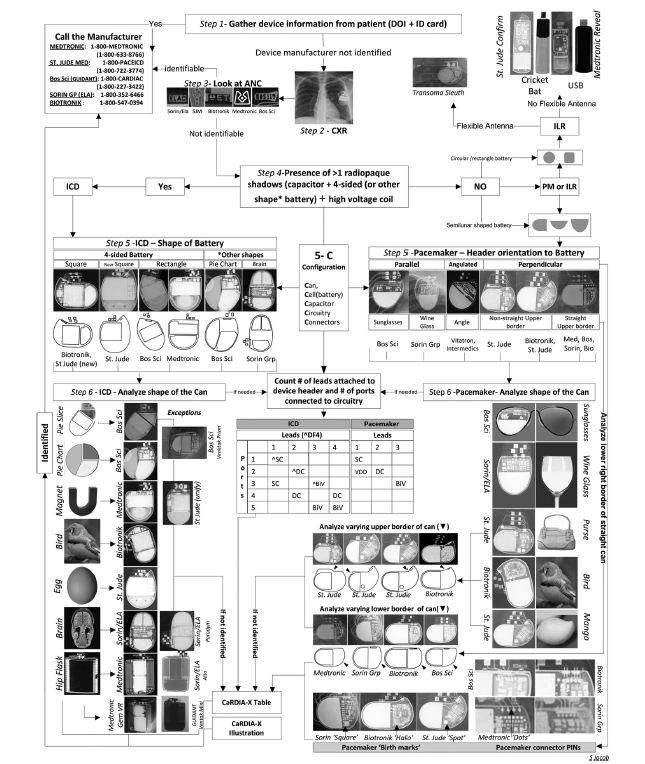
CaRDIA-X Algorithm
Effect of Magnet on Pacemaker (Core EM Video Link)
- Magnet application over a pacemaker will lead the pacemaker to default to the “magnet mode”
- Typically will lead to asynchronous pacing mode (does not turn off the pacemaker)
- Results in a constant paced rate regardless of the native rate or rhythm (eliminates sensing function)
- Either AOO, VOO or DOO
- The pacemaker will pace either the atrium, ventricle or both but will not sense or have a response to sensing
- Risk: Asynchronous ventricular pacing can lead to pacemaker-induced ventricular tachycardia
Pacemaker Malfunction
- Problems with Sensing
- Undersensing
- Definition: Pacemaker fails to sense native cardiac activity resulting in asynchronous pacing
- Can be complete or intermittent
- Commonly results from exit block
- Exit block: Failure of an adequate pacemaker stimulus to depolarize the chamber. Endocardium in contact with pacing lead requires higher stimulation threshold for conduction
- Exit block results from changes in cardiac tissue over time (i.e. an RV Infarction, progressive cardiomyopathy)
- EKG Findings
- Pacing spikes occurring earlier than the programmed rate
- Spike may not be followed by QRS complex if within the refractory period
- Presence of spikes within QRS complexes also suggestive (asynchrony)
- Oversensing
- Definition: Pacemaker mistakes electrical signals as native cardiac activity and thus, pacemaker function is inhibited
- Sources: Large P or T wave, pectoralis muscle contraction, cell phone signal (typically when on ipsilateral ear)
- Undersensing
- Problems with Pacing
- Output Failure
- Definition: No paced stimulus is generated from the device resulting in decreased or absent pacemaker function
- Causes: Oversensing, Lead displacement, Fracture of pacing wires
- Failure to Capture
- Definition: Electrical stimulus does not result in depolarization of the myocardium (no QRS complex generated)
- Causes: Exit block, myocardial infarction, lead displacement, wire fracture, electrolyte abnormalities
- Output Failure
Failure to Capture (LITFL)
- Pacemaker Associated Dysrhythmias
- Sensor-induced tachycardia
- Pacemakers designed to respond to physiologic stress by increasing heart rate (i.e. during exercise, hypercapnia, tachypnea)
- Pacemaker reacts to stimuli not intended to increase heart rate (vibrations, electrocautery, muscle contractions) resulting in inappropriate rate (rate will not exceed pacemaker’s upper rate limit)
- Treatment: Application of a magnet will terminate the pacemaker’s oversensing and result in pre-set pacemaker rate
-
Pacemaker Mediated Tachycardia (learningecg.blogspot.com:)
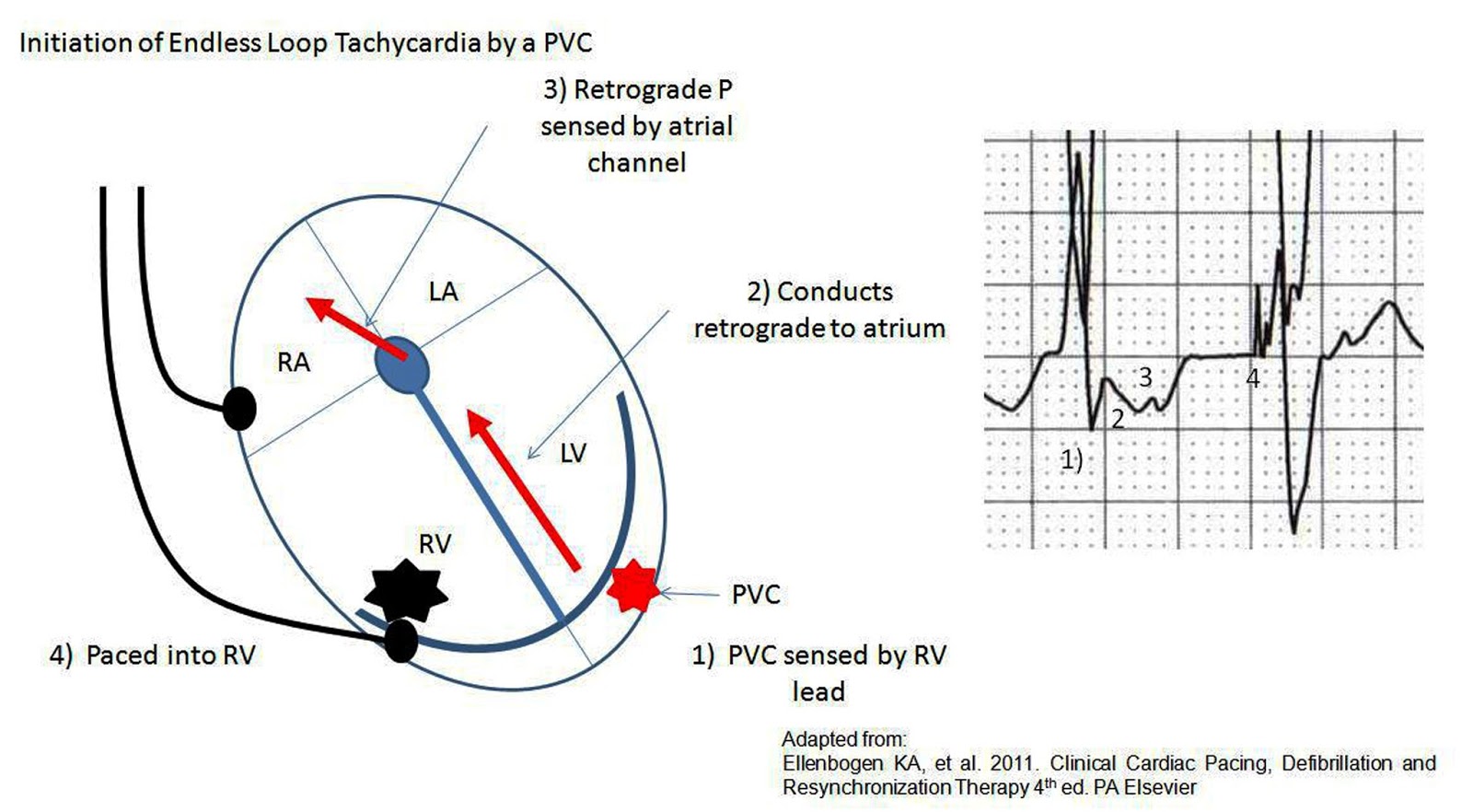
Pacemaker mediated tachycardia (PMT) (aka endless loop tachycardia)
- Re-entry Tachycardia: Ventricular depolarization conducts retrograde into the atria leading atrial lead to detect activity as incoming P wave resulting in ventricular depolarization (viscous cycle develops)
- Treatment
- Administer AV blocker (adenosine, beta blocker, calcium channel blocker)
- Apply magnet over pacemaker
- Sensor-induced tachycardia
Pacemaker Mediated Tachycardia (LITFL)
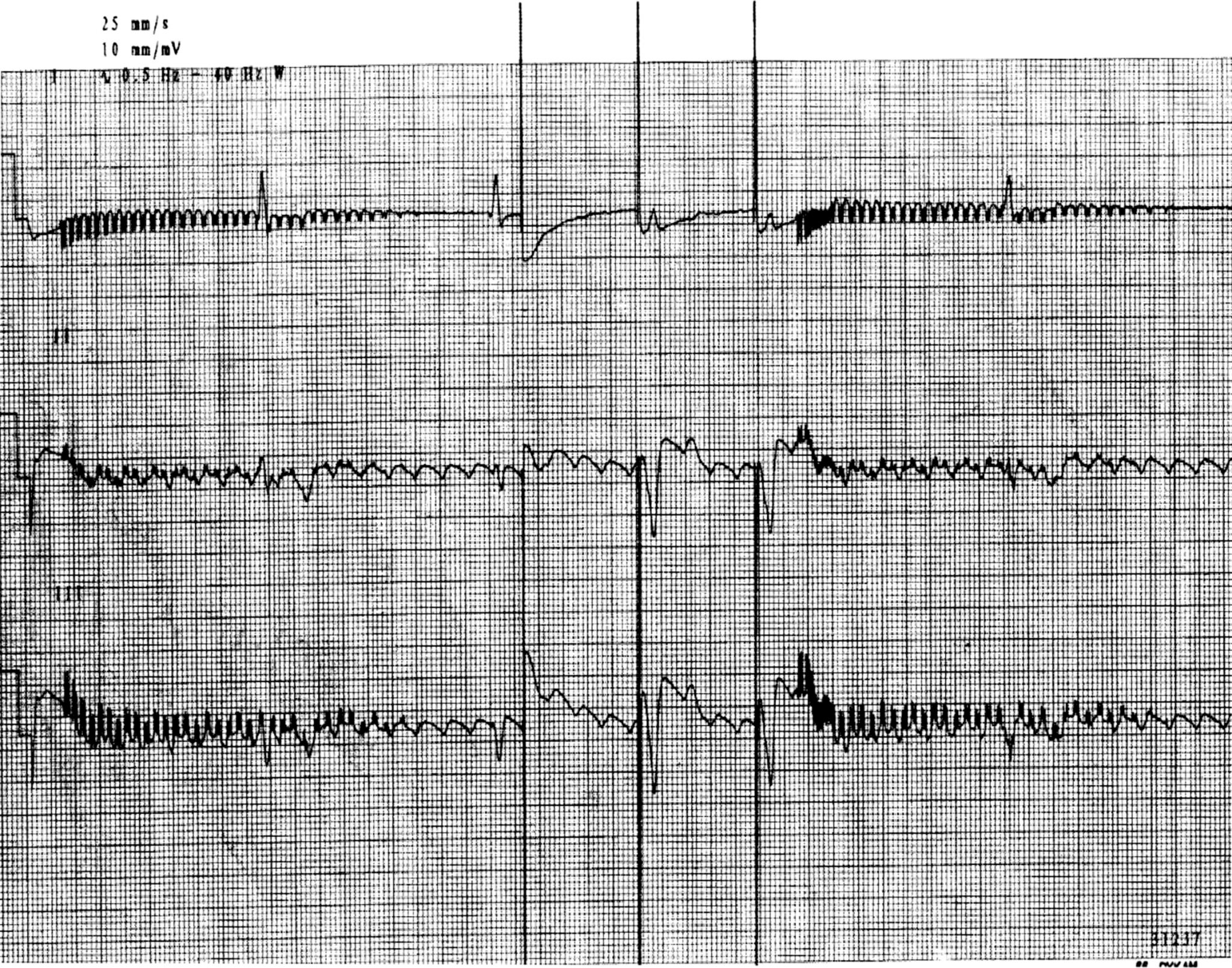
- Runaway pacemaker (Ortega 2005)
- Life-threatening malfunction seen in older-generation pacemakers resulting from low battery voltage
- Pacemaker delivers runs of pacing spikes in excess of 2000 bp
- Can provoke ventricular fibrillation
- Can also cause failure to capture as spikes low amplitude
- Treatment
- Apply magnet over pacemaker
- Replace pacemaker
Runaway Pacemaker (LITFL)
- Lead displacement dysrhythmia
- Results from a dislodged pacing wire “floating” around the right ventricle
- EKG: May demonstrate changing QRS morphology
- CXR: May aid in diagnosis
- Twiddler’s Syndrome
- Dysfunction of the pacemaker resulting from patient manipulation of the pulse generator
- Repeated manipulation results in the pacemaker rotating on it’s axis and dislodgment of the pacing leads
- Can cause pacing of the diaphragm or brachial plexus (arm twitching)
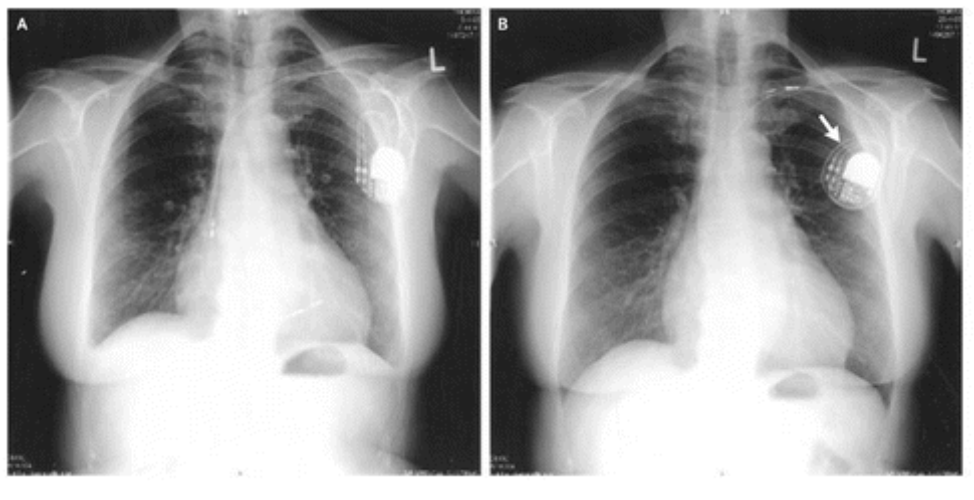
Twiddler’s Syndrome (NEJM)
Read More
LITFL: Pacemaker Rhythms – Normal Patterns
LITFL: Pacemaker Malfunction
Canadiem: Pacemaker Essentials: What We Need to Know in the ED
Core EM: How to Use a Magnet for Pacemakers + ICDs
Riemann JT, Squire B: Implantable Cardiac Devices, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2010, (Ch) 80: p 1064-75.
References
Kucher N. Deep-vein thrombosis of the upper extremities. NEJM 2011; 364:861. PMID: 21366477
Jacob S et al. Cardiac rhtyhm device identification algorithm using X-Rays: CaRDIA-X. Heart Rhythm 2011; 8(6): 915-22. PMID: 21220049
Ortega DF. Runaway pacemaker: A forgotten phenomenon? Europace 2005; 7(6): 592-7. PMID: 16216762




