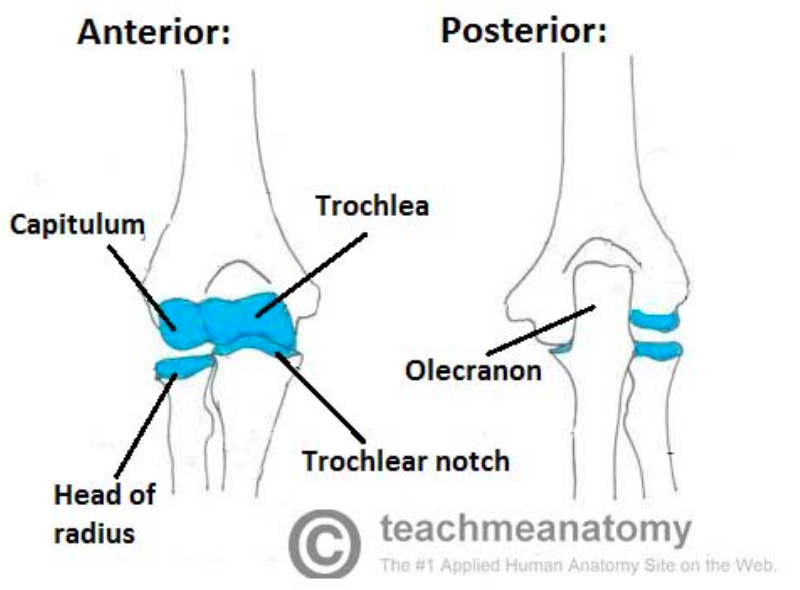
Articulations of the Elbow Joint (teachmeanatomy.info)
Definition: Fracture of proximal ulna at the level of articulation with humerus
Mechanism
- Most commonly secondary to direct trauma to olecranon
- Fall on outstretched hand with flexed elbow
- Low-energy fractures are due to abrupt contraction of both the triceps and brachialis muscles
- Stress fracture is less common and seen predominantly in throwing athletes (e.g. baseball) with a gradual onset of pain worse with repeated throwing motions
Epidemiology
- Represent 10-20% of upper extremity fractures (Schwartz 2008)
- Olecranon fractures in younger patients are often due to high-energy direct trauma
- Elderly patients can sustain olecranon fractures from low-energy mechanisms such as a fall from standing
Physical Exam
- Palpable defect may be appreciated with displaced or comminuted fractures
- Posterior elbow tenderness to palpation with associated joint swelling
- Forearm Extension
- Triceps inserts into the posterior proximal ulna
- Commonly associated with a displaced olecranon fracture
- Loss of forearm extension by the triceps muscle
- Test forearm extension against resistance. Loss of extension mechanism can be masked if patient simply allows arm to drop with gravity
- Perform full neurovascular exam
- Confirm presence and strength of circulation distal to injury at both ulnar and radial arteries.
- Look for signs of hypoperfusion such as a pale limb, prolonged capillary refill, and decreased limb temperature
- The ulnar nerve runs posterior to the medial epicondyle into the cubital tunnel and can be injured with olecranon fractures.
- Check for sensory deficits over the palmar surface of the fifth digit and motor weakness in interossei muscles of the hand. Abnormalities indicates ulnar nerve injury
- Closely examine for lacerations, which could suggest open fracture given close proximity of olecranon and overlying skin
- Test elbow instability and for ligament injury
- Apply varus and valgus stress with elbow flexed at 30 degrees
- Instability with varus stress indicates medial collateral ligament injury
- Instability with valgus stress indicated ulnar collateral ligament injury.
- Assess for evolving compartment syndrome

Comminuted Olecranon Fracture (accessemergencymedicine.mhmedical.com)
X-Ray Findings
- Images required: AP, Oblique and True Lateral
- Importance of True Lateral
- Shoulder, elbow and wrist must be in the same plane to assess the anterior humeral, radiocapitellar line, and olecranon. Elbow in 90 degrees flexion
- Normal: Proximal radial lines meets anterior humeral line approximately center of capitulum. Supracondylar ridge is in hourglass or figure 8 at distal humerus.
- Without a true lateral elbow film it is difficult to accurately determine amount of fracture displacement and intra-articular involvement (both are needed for classification and management)
- Unopposed tricep muscle action after fracture can cause wide displacement of fracture.
- Look for associated fractures or dislocations of coronoid process, radial head, and distal humerus
- CT may be needed for surgical planning
Olecranon Fracture Images

Olecranon Avulsion Fracture (Case courtesy of Dr David Cuete, Radiopaedia.org. From the case rID: 27347)

Comminuted Olecranon Fracture (Case courtesy of Dr Jeremy Jones, Radiopaedia.org. From the case rID: 6384)

Olecranon Fracture (Case courtesy of Dr Jeremy Jones, Radiopaedia.org. From the case rID: 12389)
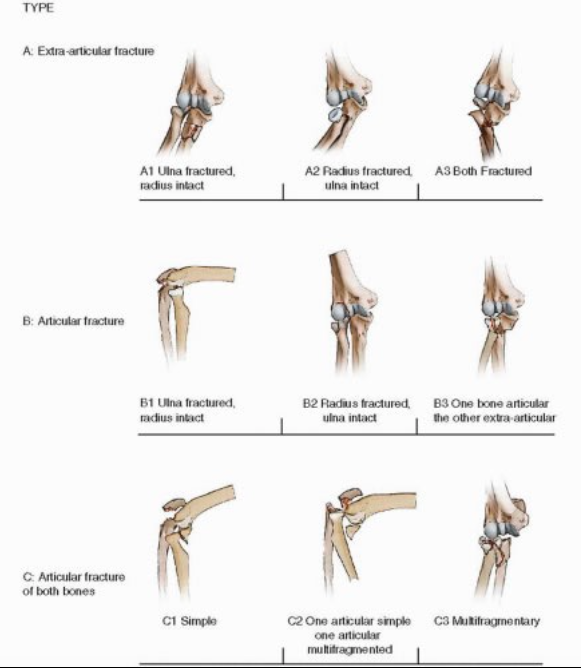
AO Classification (http://musculoskeletalkey.com/)
Classification Systems
- Unstable Fractures
- Significant displacement (> 1-2 mm)
- Loss of extension at the elbow
- Elbow instability on exam
- Evidence of neurovascular compromise
- Open fractures
- AO Classification System
- Simplest and most commonly used
- Combines proximal ulna and radius fractures into one group
- AO Classification
- Type A: extra-articular
- Type B: Intra-articular
- Type C: Intra-articular fractures of both the radial head and olecranon
- Mayo Classification System
- Based on stability and displacement/comminution of the fracture
- Mayo Classification
- Type 1: Non-displaced with non-comminution (subtype A) or comminution (subtype B)
- Type II: Displaced > 3 mm but collateral ligaments are intact, considered stable. Can be non comminuted (subtype A) or comminuted (subtype B)
- Type III: Displaced and unstable, forearm unstable in relation to humerus, assumes ligamental compromise, can be either non-comminuted (subtype A) or comminuted (subtype B)
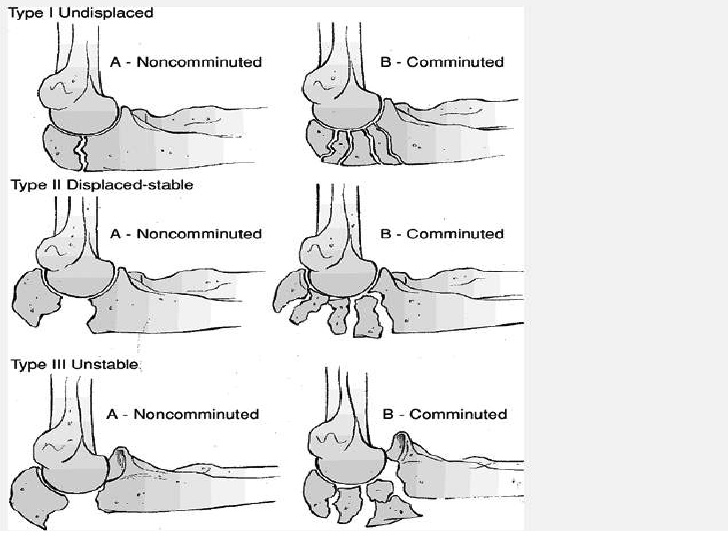
Mayo Classification (http://image.slidesharecdn.com/)
ED Management
- Unstable fractures, as detailed above, require emergent orthopedic consultation for operative fixation.
- Apply splint at 50-90% flexion and analgesia.
- Intravenous antibiotics for open or suspected fractures.
- Stable, nondisplaced fractures with intact extensor function
- Immobilized in a long arm posterior splint with 90 degrees of flexion, neutral forearm
- Orthopedic follow up within 1-2 days.
Prognosis
- High rate of union with appropriate treatment >90% (Chow 2006)
- Nondisplaced fractures can begin range of motion exercises at 1 week.
- The most frequently patient-reported complication after surgery is painful hardware. After fracture is healed hardware can be removed.
- Depending on surgical technique more than 20% of patients require a second surgery for hardware removal (Wheeless 2013)
- Patients may have a permanent 10-15 degree loss of extension (Wheeless 2013)
Take Home Points
- Appreciation of loss of elbow extension mechanism or elbow instability on physical can help determine need for surgical intervention
- Olecranon fractures can be associated with injury to the ulnar nerve, which runs posterior to the medial epicondyle into the cubital tunnel
- Posterior elbow lacerations should raise concern for open fracture
- Frequent reevaluations and high suspicion for compartment syndrome
- Low-energy mechanism of injury can cause olecranon fractures in elderly patients, maintain a low threshold for imaging
Read more
Radiopedia: Olecranon fractures
Radiopedia: Lateral elbow x-rays
Orthobulltes: Olecranon fractures
References
Chow YC. Elbow and Forearm Injuries. In: Tintinalli JE, Stapczynski J, Ma O, Yealy DM, Meckler GD, Cline DM. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. New York, NY: McGraw-Hill; 2016. Link
Germann CA. Elbow. In: Sherman SC. eds. Simon’s Emergency Orthopedics, 7e. New York, NY: McGraw-Hill; 2014. Link.
Greenberg MI. Greenberg’s text-atlas of emergency medicine. Philadelphia : Lippincott Williams & Wilkins, c2005. (2005) ISBN:0781745861
Jordanov MI et al. .Chapter 9. Upper Extremity. In: Block J, Jordanov MI, Stack LB, Thurman R. Block J, Jordanov M.I., Stack L.B., Thurman R Eds. Jake Block, et al.eds. The Atlas of Emergency Radiology. New York, NY: McGraw-Hill; 2013. Link
Schwartz DT. Chapter III-1. Elbow Fat Pad—Monteggia Fracture. In: Schwartz DT. eds. Emergency Radiology: Case Studies. New York, NY: McGraw-Hill; 2008. Link
Wheeless, C. R. “Fractures of the Olecranon Duke Orthopaedics Wheeless’ Textbook of Orthopaedics.” (2013). Link