Overview: Ocular ultrasound is a fast and simple technique that can be performed at the bedside to help differentiate between various ophthalmologic emergencies.
Indications:
- Eye pain, acute change in vision, eye trauma
- Suspected elevation in intracranial pressure (ICP)
- When overlying edematous or contused periorbital tissue prohibits direct visualization of the eye
Contraindications:
- Suspected globe rupture as any pressure placed on the eye can potentially exacerbate damage
- NB: If you are concerned about globe rupture, do not ultrasound the eye and obtain a CT instead.
Technique:
- With the head of the bed at 45 degrees, apply a large tegaderm over the closed eye of interest. Apply a copious amount of standard, water-soluble ultrasound gel on top of the tegaderm
- Using the high-frequency linear probe with minimal topical pressure, gently scan the eye in both the sagittal and axial planes
- Ask the patient to look up, down, left or right as needed to improve your view
- Image the contralateral eye for comparison if you are having difficulty differentiating normal from abnormal
Normal Anatomy:
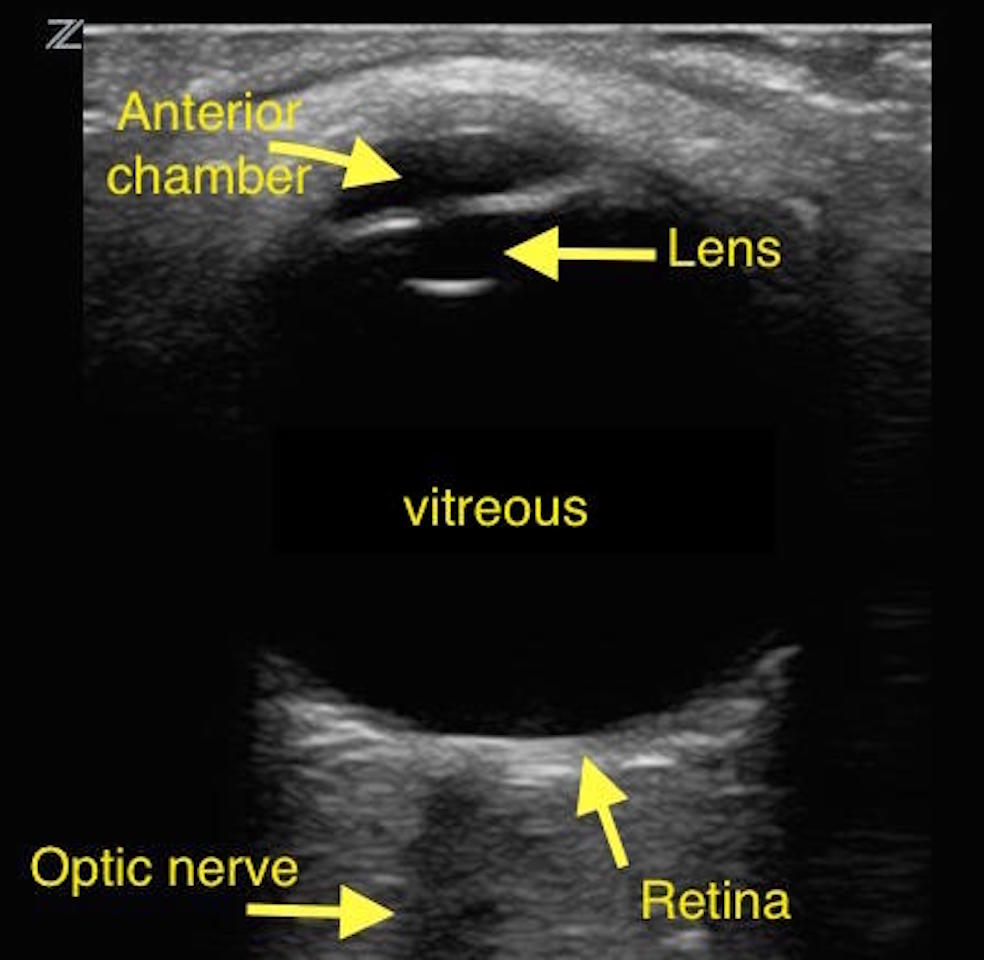
Normal Anatomy
Ultrasound Differential for Trauma:
- Globe rupture
- Do NOT perform ultrasound if known globe rupture
- Presentation:
- Painful vision loss after high impact blunt or penetrating trauma
- Can visualize distortion of pupil, extrusion of vitreous fluid and prolapse of internal structures on physical exam
- Findings:
- Decrease in size of the globe
- Anterior chamber collapse
- Vitreous hemorrhage (see below)
- Disruption of normal globe architecture
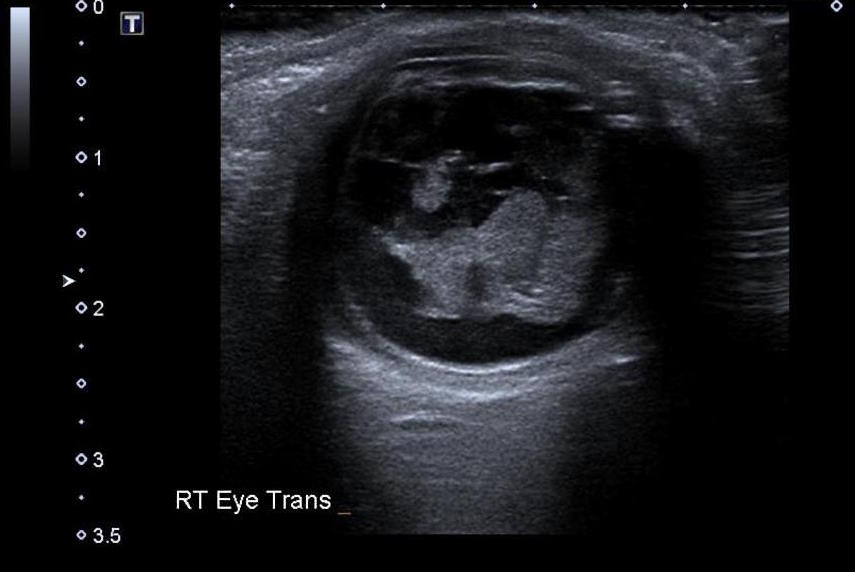
Globe Rupture – Source: Dr Craig Hacking, https://radiopaedia.org/
From the case https://radiopaedia.org/cases/35142
- Retrobulbar Hematoma
- Presentation:
- Proptosis
- Elevated intraocular pressure (>40 mmHg)
- Decreased visual acuity after trauma
- Findings:
- Hypoechoic fluid collection posterior to the globe
- Note: This is an ocular emergency and can lead to permanent vision loss if not decompressed rapidly
- In cadaver lab study: Sensitivity 85%, Specificity 89%, PPV 66%, NPV 95.9% for EM residents. EM US fellowship trained attendings had a sensitivity of 100% (Gibbons 2018)
- Presentation:
- Foreign Body
- Presentation:
- Secondary to eye trauma, notably projectile penetrating trauma
- Can present with or without pain and vision loss
- May be asymptomatic
- Note: Even asymptomatic foreign bodies can progress to permanent vision loss so all patients should be carefully evaluated
- Findings:
- Hyperechoic object, possibly producing shadow or comet tail artifact
- Can also see “twinkle” artifact when color doppler is applied
- In porcine model with metallic foreign bodies: Sensitivity 88%, Specificity 96%, PPV 96%, NPV 85% (Shiver 2005, PMID: 16179616)
- Presentation:
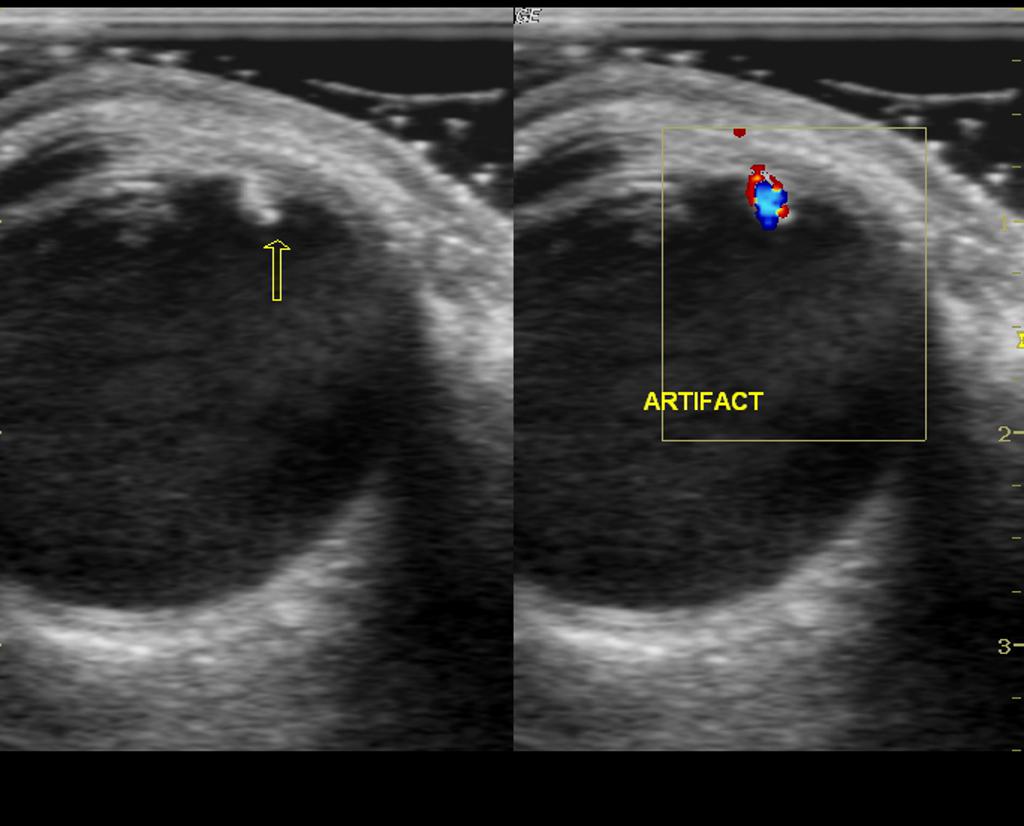
Foreign Body – Source: Dr Maulik S Patel, https://radiopaedia.org/
From the case https://radiopaedia.org/cases/21698
- Lens Detachment
- Presentation: May present as decreased vision with a normal pupillary response and without signs of open globe injury
- Note: Usually due to trauma. Occurrences in children or secondary to minor trauma should prompt investigation for an underlying genetic cause
- Findings: Posteriorly-displaced lens
- Sensitivity 84.6%, Specificity 98.3%, Positive Likelihood Ratio 49.5, Negative Likelihood Ratio 0.15 (Haghighi 2014, PMID: 26495362)
Ultrasound Differential for Painless Vision Changes
- Retinal Detachment
- Presentation:
- Acute onset of unilateral floaters and/or pinpoint flashing lights (photopsias)
- Can have visual loss or visual field cuts
- Note: Can be caused by trauma but more commonly occurs spontaneously or secondary to systemic disease (i.e. vasculopathies)
- Findings: Hyperechoic linear structure in the posterior chamber that has separated from the posterior choroid and is tethered centrally to the optic nerve (Note: the retina is a continuation of the optic nerve)
- Sensitivity 75%, Specificity 94%, Positive Likelihood Ratio 12.4, Negative Likelihood Ratio 0.27 (Kim 2019, PMID: 29774966)
- Presentation:
- Vitreous Detachment
- Presentation:
- Acute unilateral visualization of floaters
- Can have visual loss or visual field cuts
- Note: This is a common cause of retinal detachment
- Findings: Hyperechoic linear floating structure often with increased echogenicity between the structure and the posterior surface of the globe
- Note: Similar in appearance to retinal detachment but will not be tethered to the optic disc
- Sensitivity 80.9%, Specificity 33.3% (Woo 2016, PMID: 27769323)
- Presentation:
Vitreous Detachment – Source: Dr. Matt Riscinti and Dr. Bryan Flores,
http://www.thepocusatlas.com/orbital
- Vitreous Hemorrhage
- Presentation:
- Sudden painless visual loss or visual “haze”
- Can be spontaneous or secondary to trauma
- Findings: Swirling, slightly hyperechoic, “washing machine” appearing material in the posterior chamber
- Note: You may have to increase the gain to adequately visualize. Prompting the patient to move the eye side to side will demonstrate swirling
- Sensitivity 43%, Specificity 93.8% (Woo 2016, PMID: 27769323)
- Presentation:
-
- Note: Each of these ocular pathologies can appear alone or in combination and can be difficult to differentiate. All three will require ophthalmologic consultation.
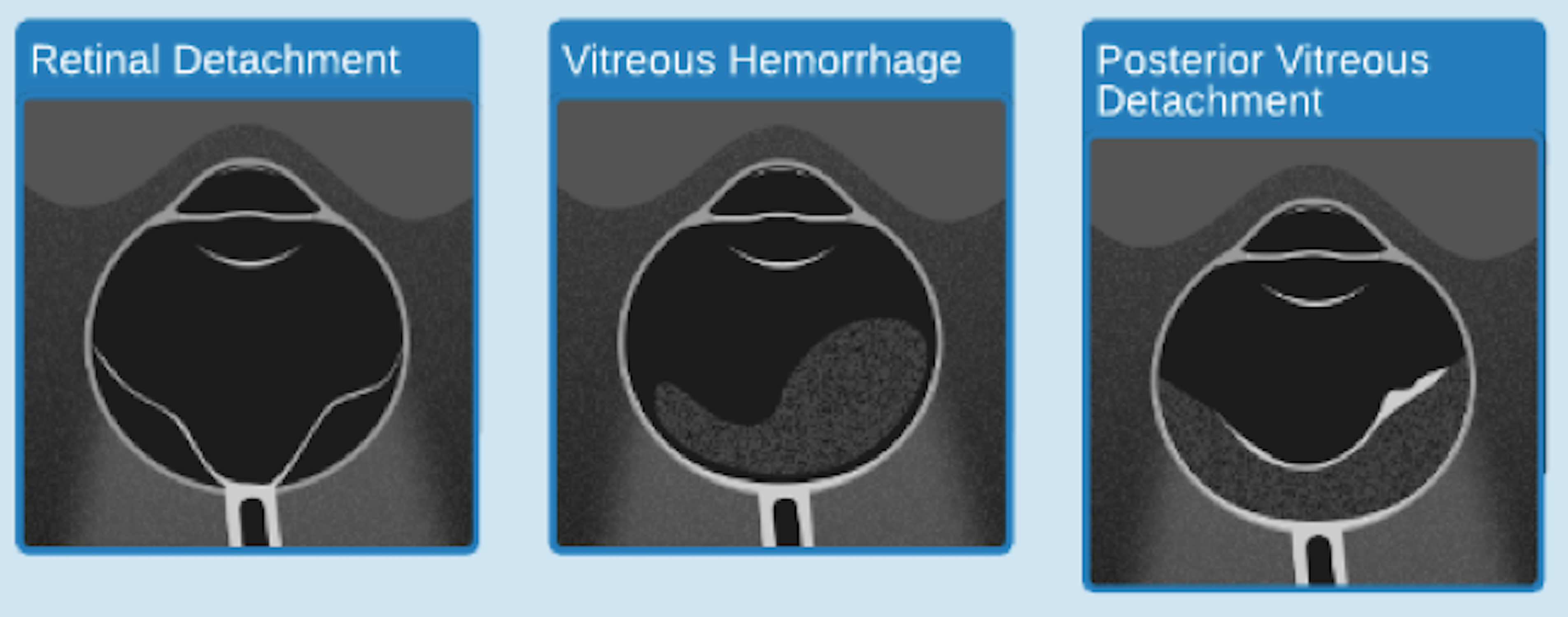
Source WikiEM https://wikem.org/w/images/Image.png
Evaluation of increased intracranial pressure (ICP):
- The optic nerve sheath communicates directly with the intracranial space. Therefore, increased ICP is reflected in dilation of the optic nerve, often with anterior bulging of the optic disc, which is seen as papilledema on fundoscopic exam
- Ocular ultrasound can be used to measure the optic nerve sheath diameter and identify bulging of the optic disc (Teismann 2013, PMID: 24050798)
- To measure the nerve sheath diameter, remember 3×5. In both eyes, measure the diameter of the optic nerve sheath 3 mm distal to the posterior aspect of the globe
- <5 mm is normal, 5-6 mm is indeterminate, >6mm is elevated
- The sensitivity of a 5 mm cut off is quoted as 88% to 100% with a specificity of 63% to 95% depending on the study (Shevlin 2015)
- The presence of papilledema on ultrasound can help if you are in the indeterminate range, but its absence does not indicate normal ICP
- For a deep dive into the evidence see: https://emcrit.org/pulmcrit/pulmcrit-algorithm-diagnosing-icp-elevation-ocular-sonography/
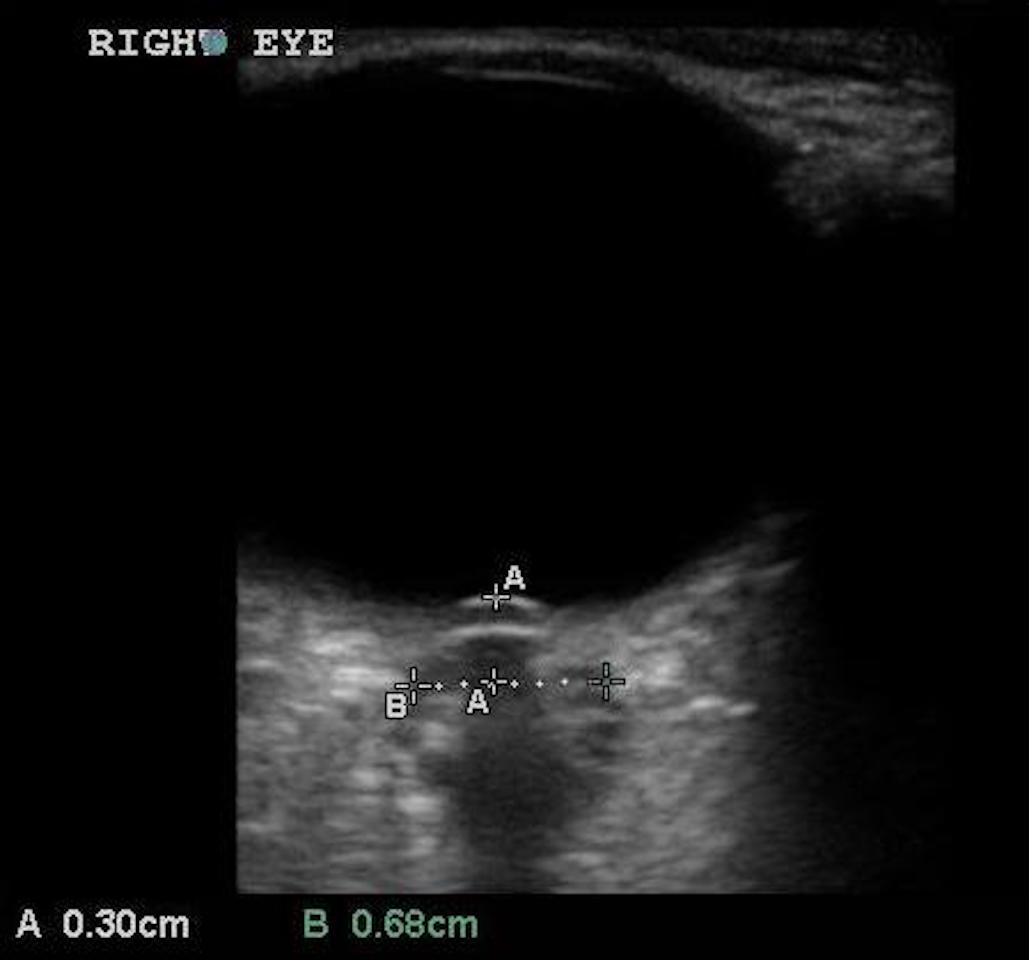
Elevated ICP: Dilated Optic Nerve Sheath with Papilledema
Take Home Points:
- Ocular ultrasound is quick and easy to perform
- Consider ultrasound any time you are presented with a patient with eye trauma or vision changes
- Use a Tegaderm and plenty of gel
- Do not apply pressure on an eye if you are concerned about globe rupture
- To check for elevated ICP remember 3×5. Measure 3 mm posterior to the globe, less than 5 mm is normal
References
Gibbons, R., Zanaboni, A., Patterson, J., & Costantino, T. (2018). Point-of-Care Ultrasound Diagnosis of Retrobulbar Hematoma in Cadaveric Models. Annals of Emergency Medicine, 72(4).
Shiver, S. A., Lyon, M., & Blaivas, M. (2005). Detection of metallic ocular foreign bodies with handheld sonography in a porcine model. Journal of ultrasound in medicine, 24(10), 1341-1346. PMID: 16179616
Haghighi, S. H. O., Begi, H. R. M., Sorkhabi, R., Tarzamani, M. K., Zonouz, G. K., Mikaeilpour, A., & Rahmani, F. (2014). Diagnostic accuracy of ultrasound in detection of traumatic lens dislocation. Emergency, 2(3), 121. PMID: 26495362
Kim, D. J., Francispragasam, M., Docherty, G., Silver, B., Prager, R., Lee, D., & Maberley, D. (2019). Test characteristics of point‐of‐care ultrasound for the diagnosis of retinal detachment in the emergency department. Academic Emergency Medicine, 26(1), 16-22. PMID: 29774966
Woo, M. Y., Hecht, N., Hurley, B., Stitt, D., & Thiruganasambandamoorthy, V. (2016). Test characteristics of point-of-care ultrasonography for the diagnosis of acute posterior ocular pathology. Canadian Journal of Ophthalmology, 51(5), 336-341. PMID: 27769323
Teismann, N., Lenaghan, P., Nolan, R., Stein, J., & Green, A. (2013). Point‐of‐care ocular ultrasound to detect optic disc swelling. Academic Emergency Medicine, 20(9), 920-925. PMID: 24050798
Shevlin, C. (2015). Optic nerve sheath ultrasound for the bedside diagnosis of intracranial hypertension: pitfalls and potential. Critical Care Horizons, 1(1), 22-30.
All images courtesy of Dr. Marsia Vermeulen unless otherwise specified.

Thanks very informative
Thanks very informative
I remembered Detachment