Introduction
- Constellation of findings including: Proteinuria, hypoalbuminemia, hyperlipidemia, and edema caused by a variety of renal glomerular diseases
- 75% are primary and caused by minimal change nephropathy
- Most common: 1.5-8 years, Male > Female
- Overall mortality is low (2-5%), higher with chronic and relapsing disease
Physiology
- Total Body Water = IntraCellular Fluid (2/3) + ExtraCellular Fluid (1/3).
- ExtraCellular Fluid = Intravascular Volume (1/4) + Interstitial Fluid (3/4).
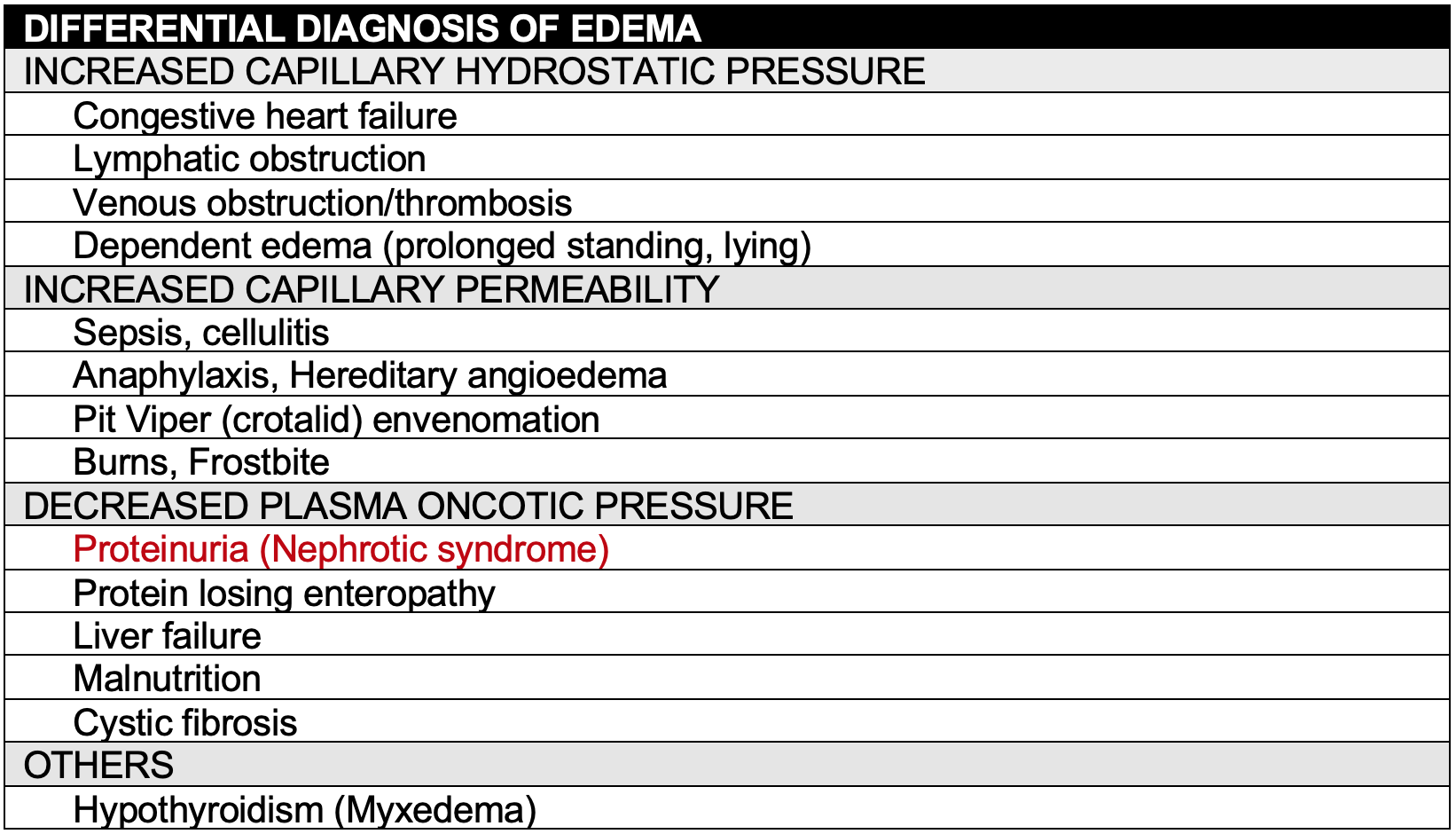
- Starling’s law governs fluid distribution. Edema caused by:
- ↑ Capillary hydrostatic pressure gradient
- ↓ Oncotic pressure gradient
- ↑ Capillary permeability
History
- Swelling is the most common presenting symptom (98%)
- Other symptoms: Irritability, fatigue, abdominal pain, diarrhea
- Less common: Foamy urine and/or hematuria
Physical Exam
- Pitting edema
- First in areas of low tissue resistance: Periorbital, scrotal/labial, pretibial
- Focal swelling → Generalized edema: Ascites, anasarca, and pleural effusions
- Hypertension, may precipitate seizures
- Respiratory distress due to pleural effusion, empyema, pulmonary embolism
- Abdominal distension/tenderness secondary to ascites, peritonitis
- Rash, purpura, petechiae, adenopathy, or arthritis suggests a multi-system etiology
Laboratory / Imaging
- UA: > 1+ protein (If ↑ RBC and/or WBC, consider nephritis, other renal diseases)
- Urine Protein/Creatinine ratio > 2
- Serum: Hypoalbuminemia < 2.5 gm/dl
- Serum: Hyperlipidemia (↑ Cholesterol, LDL, triglycerides)
- Serum: Basic metabolic panel to assess renal function (BUN, Cr, HCO3, K)
- Serum: Troponin for suspected MI
- CXR/EKG: Chest pain, cough, shortness of breath
- Consider CT angiogram for PE, duplex doppler ultrasound for DVT
Renal Biopsy
- A renal biopsy is not indicated for a typical presentation
- Considered if:
- < 1 year of age (higher risk of congenital disease)
- > 10 years of age
- History, physical exam, or laboratory data indicate a secondary cause of nephrotic syndrome or primary nephrotic syndrome other than minimal change
Complications
- Fluid Overload
- An increase in total body water through 3rd spacing of fluids can result in pulmonary edema, pleural effusion and ascites
- Patients may be intravascularly depleted with a normal or ↑ total body water
- Traditional signs of dehydration may be absent
- ↑ BUN, Creatinine: Due to ↓ intravascular volume or renal insufficiency/failure
- Infection
- Immunocompromised and at risk of sepsis and focal infections due to:
- Urinary excretion of immunoglobulins
- Standing free fluid in the pleural (empyema) and peritoneal cavities (peritonitis)
- Treatment with steroids
- Infections typically due to encapsulated organisms:
- Streptococcal pneumoniae, Haemophilus influenzae, Klebsiella pneumoniae, Neisseria meningitides, Group B streptococcus and Salmonella typhi
- Immunocompromised and at risk of sepsis and focal infections due to:
- Thrombosis
- Loss of antithrombin III, plasminogen, and protein S in the urine, in addition to hemoconcentration, predisposes to arterial and venous thrombosis
- Renal vein thrombosis should be considered in patients with significant hematuria or signs of renal insufficiency
- Respiratory symptoms may due to pulmonary embolism or myocardial infarction
- A D-dimer may be elevated at baseline and may not be diagnostic of pulmonary embolism or deep vein thrombosis
- Obtain a spiral chest CT if pulmonary embolism is suspected
- Obtain doppler sonography if deep vein thrombosis is suspected
- Obtain an EKG and troponins if myocardial infection is suspected
- Central venous catheters should be avoided
- Role of prophylactic anticoagulation is unclear, reserved for high-risk patients
Management
- Albumin infusion prior to diuresis to avoid exacerbating intravascular depletion.
- Abdominal pain, fever and peritoneal signs → Paracentesis
- Beside ultrasonography may be used to guide the procedure
- Antibiotics should cover gram positive and enteric pathogens (see above)
- Patients with significant respiratory distress due to a pleural effusion should undergo an ultrasound-guided therapeutic pleurocentesis
Medications
- Trial of corticosteroids is the 1st step in treatment of idiopathic nephrotic syndrome
- Prednisone: 2 mg/kg/day x 6 weeks then 1.5 mg/kg QOD x 6 weeks
- Antihypertensives for significant hypertension: ACE inhibitors, ARB
- Diuretics for severe edema: Lasix 1-2 mg/kg/day
- Antibiotics for suspected or confirmed focal infection or sepsis
- Statins for persistent hypercholesterolemia
- Consider anticoagulation for pulmonary embolism, DVT, MI, renal vein thrombosis
- Rituxumab, a monoclonal anti Cd20 antibody may be indicated if steroid refractory
Disposition
- Well appearing patients can be discharged with follow-up with pediatric nephrology
- Sodium restricted diet while edematous, hypertensive
- Pneumococcal vaccination as an outpatient
- Check first morning voids for protein (if in remission)
- Advise parents to seek medical attention for signs of disease progression
- Disease progression:
- Increasing edema, worsening abdominal distension
- Urinary protein found (if in remission)
- Decreased urine output
- Complications:
- Appears ill
- Abdominal pain, vomiting
- Fever
- Headache (Hypertension)
- Respiratory symptoms: cough, shortness of breath, chest pain
- Seizure
- Disease progression: