Metacarpal Fractures (www.sportsmd.com/)
Background
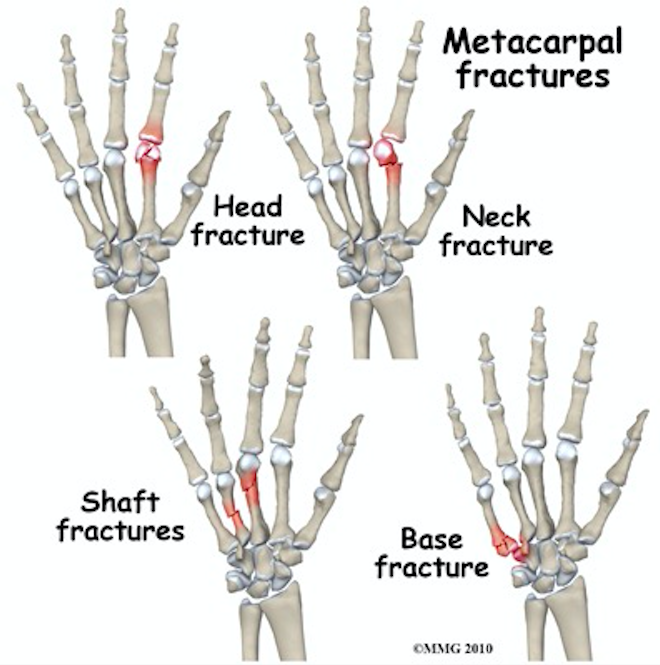
- Definition: Fracture of a metacarpal bone, through the head, neck, shaft, or base
- Mechanism
- Varies based on location of fracture
- Neck fractures
- Most common fracture pattern
- Often result from a direct axial force, such as a punch, hence the term “boxer’s fracture”
- Shaft fractures
- Direct force can result in transverse fractures
- Twisting forces lead to oblique or spiral fracture patterns
- Base fractures
- Most often direct blow or twisting force
- Head fractures
- Most often crush injuries or a direct blow
- Most commonly traumatic, but also susceptible to stress fractures from repetitive use
- Epidemiology
- An estimated 1.5 million hand fractures occur annually in the US alone (Geissler 2007)
- Most commonly affect males in the second and third decade of life
- Fractures of the 2nd through 5th metacarpals account for 88% of all metacarpal fractures (Kollitz 2014)
- The 5th metacarpal is the most common among these.
- Substantial personal and industrial economic losses due to lost productivity
Dermatomes of the Hand (www.ebmconsult.com)
Physical Exam
- Inspection and palpation
- Assessment of motor function by individual tendon function, as demonstrated below
- Perfusion, including distal capillary refill time
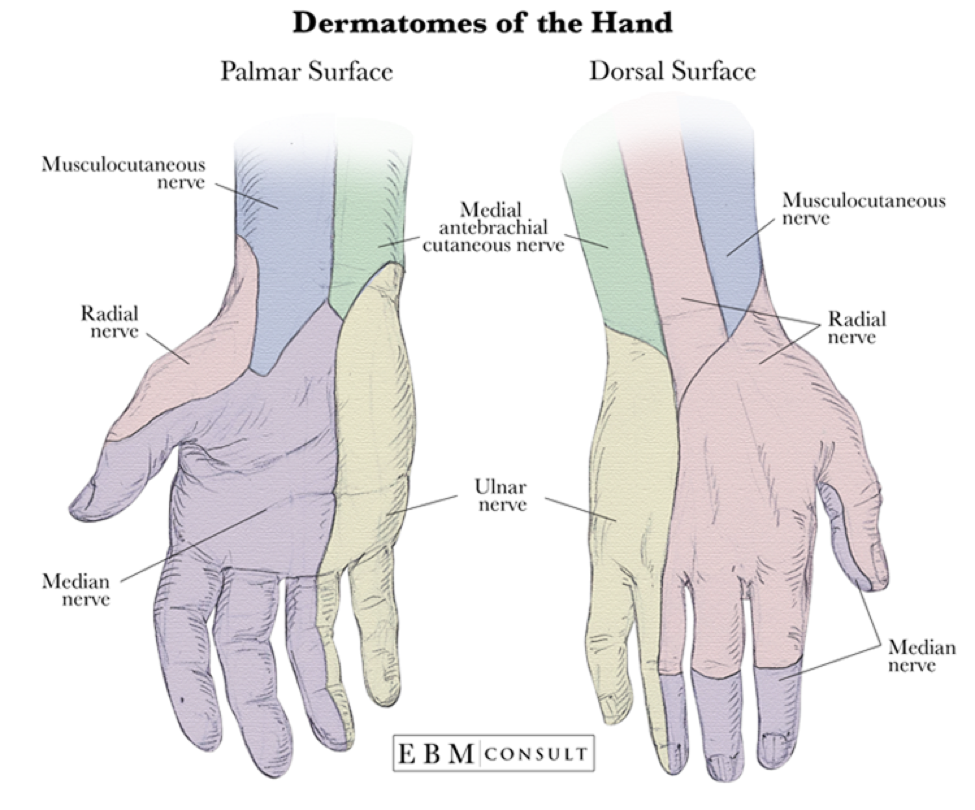
- Sensation through radial, medial, ulnar innervations
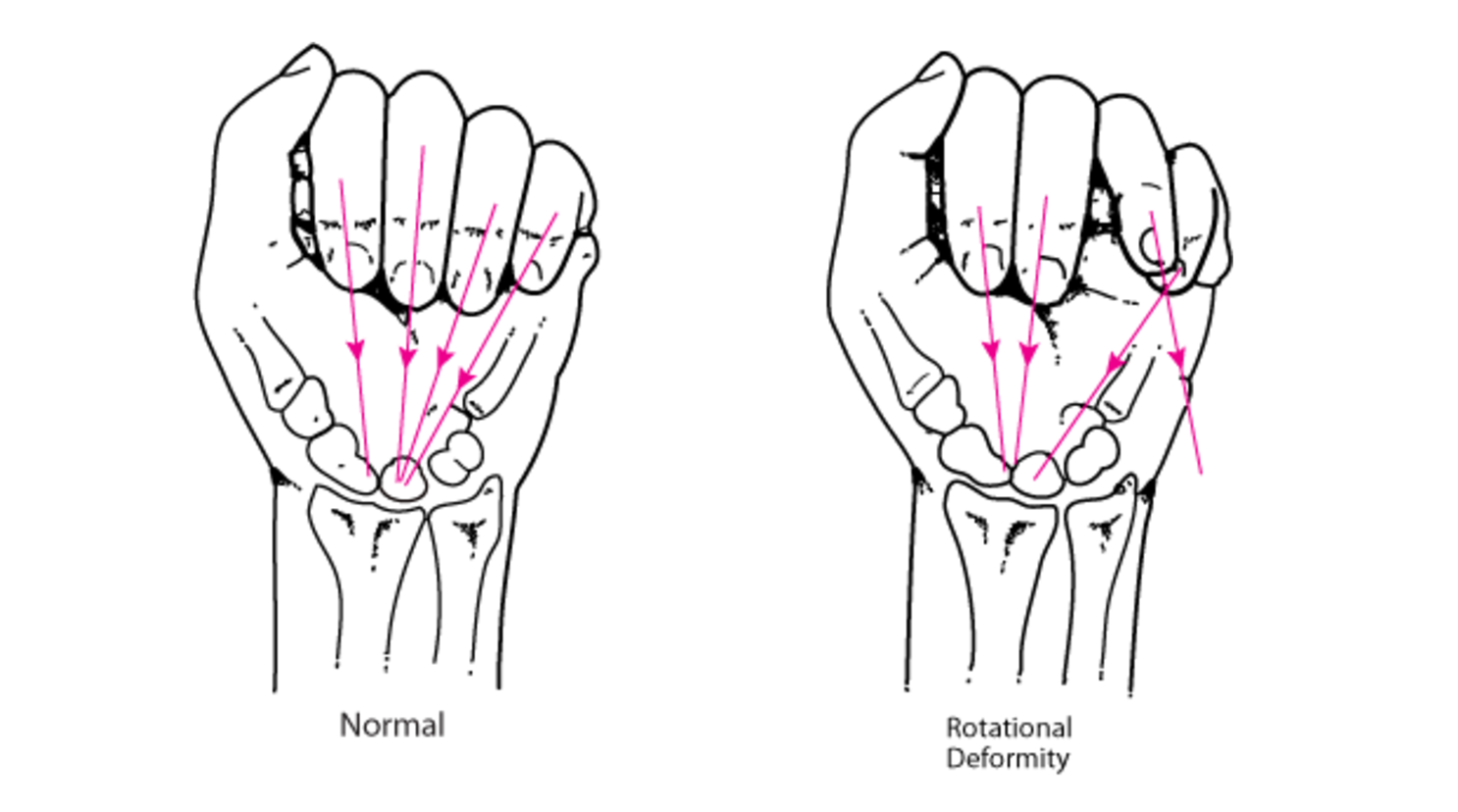
- Rotational alignment
- Specific exam consideration in suspected metacarpal injuries
- Misalignment invariably requires surgical intervention
- Assess by having the patient flex the MCP and the PIP joints in a semi-clenched fist
- Axis of each digit should be close to parallel, and should converge near the scaphoid pole or mid-wrist
- Rotational malalignment, as seen below, will result in the axis of the affected digit to deviate from the others
Rotational Alignment (www.merckmanuals.com)
Concomitant injuries:
- Any open wound over the MCP should raise concern for “fight bite.”
- Human oral floral contaminating the extensor tendon sheath or MCP joint
- These injuries often require exploration or washout
- Assess for tendinous injury as demonstrated above
- Compartment syndrome in the case of crush or high-velocity injuries
Diagnostic Imaging
- AP, lateral, and oblique plain radiographs are typically sufficient to diagnose most metacarpal fractures
- Measures of angulation should be determined using the lateral view
Diagnostic Imaging of Hand Injuries
Management
- Simple, closed fractures
- Closed reduction and splinting
- Reduce a dorsally angulated neck fracture prior to splinting
- Often achieved w/ the Jahss technique
- Fractures of the head, neck, or shaft should be splinted with a gutter splint
- In a gutter splint, maintain 90 degrees of flexion at the MCP joint
- provides tension on the collateral ligaments of the MCP, preventing shortening and subsequent stiffening while the joint is immobilized
- The most common fracture patterns, wherein the 4th and/or 5th metacarpals are involved, can be splinted with an ulnar gutter splint, as demonstrated below
- Less commonly, the radial metacarpals are effected. In this case, a radial gutter splint provides appropriate immobilization.
- Base fractures require dorsal and volar wrist splinting, with MCPs remaining free
- In a gutter splint, maintain 90 degrees of flexion at the MCP joint
- Prompt orthopedic follow up should be considered in any of the following conditions, as they likely require surgery (Eiff 2011):
- Displaced or comminuted fractures through the head
- Any fracture of the base of any metacarpal
- Angulated or displaced fractures of second or third metacarpal
- Any malrotation
- Unable to hold reduction position
- Malunion with painful grip or pseudoclawing
- Emergency orthopedic evaluation should be obtained in the case of any open fracture or open tendinous/joint injury (e.g. fight bite)
- Additional consideration should be given to patients with greater dependence on hand function for their socioeconomic stability, as in the case of laborers or craftsmen, may benefit from early surgical management rather than conservative management
- Range of motion therapy under the guidance of hand specialist.
Prognosis
- Prognosis is good for most metacarpal fractures, as many can be successfully managed nonoperatively
- Most common complication is joint stiffness, which is often responsive to range of motion exercises
Take homes
- Open fractures and concomitant open tendinous/joint injuries (e.g. fight bite) require immediate orthopedic evaluation for possible operative management
- Most fractures are simple and closed and can be managed with gutter splinting and close referral
- Pay attention for rotational deformities, associated open injuries, and compartment syndromes
Read More
OrthoBullets: Metacarpal Fractures
Radiopaedia: Metacarpal Fractures
LITFL: Boxer’s Fracture
Pediatric EM Morsels: Metacarpal Fractures
References
Blomberg, Joshua. (2017, August) Metacarpal Fractures. Retrieved from http://www.orthobullets.com/hand/6037/metacarpal-fractures?expandLeftMenu=true
Campagne, Danielle. “Metacarpal Neck Fractures (Except Thumb) – Injuries; Poisoning.” Merck Manuals Professional Edition, www.merckmanuals.com/professional/injuries-poisoning/fractures/metacarpal-neck-fractures-except-thumb
Eiff, M. Patrice, and Robert Hatch. Co-author Charles Webb. “Metacarpal Fractures.” Fracture management for primary care. Philadelphia, PA, Elsevier Saunders, 2018. ISBN-10: 143770428X
Geissler, William B, and William O McCraney. “Operative Management of Metacarpal Fractures.” Fractures of the hand and wrist, edited by David C. Ring and Mark S. Cohen, Informa Healthcare, 2007.
Kollitz KM et al. Metacarpal fractures: treatment and complications. Hand 2014; 9:16. PMID: 24570632
Merle, Michel, and Gilles Dautel. Emergency surgery of the hand. Philadelphia, PA, Elsevier, 2017. ISBN: 0323481728




