Introduction:
- Leukemia is the most common pediatric malignancy, accounting for 30% of pediatric cancer
- Acute lymphoblastic leukemia (ALL) is 5 times more common than acute myeloid leukemia (AML)
- ALL is more common in early childhood, while AML has biphasic peaks in infancy and adolescence
History and Physical:
- Nonspecific symptoms are common, and may include fever, fatigue, and anorexia
- More specific signs include splenomegaly, hepatomegaly, generalized lymphadenopathy, pallor, ecchymoses, and petechiae
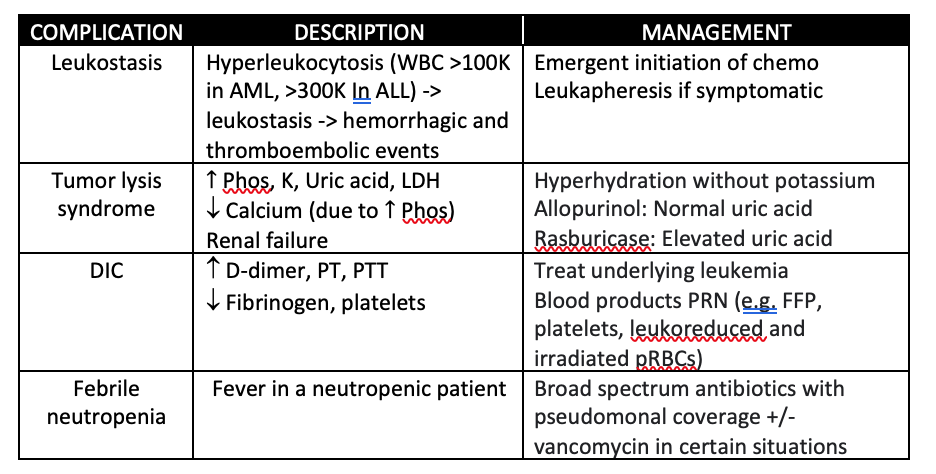
- DIC is concerning for acute promyelocytic leukemia (APML)
- Mediastinal mass (potentially leading to SVC syndrome and respiratory distress) is concerning for T-cell ALL
- Headache, vomiting, lethargy, and cranial nerve abnormalities are concerning for CNS involvement
- Mass effect due to chloroma is concerning for AML
- Testicular pain or swelling is concerning for testicular involvement
Differential Diagnosis:
- Malignant conditions: Burkitt lymphoma, aplastic anemia, small round blue cell tumors
- Non-malignant conditions: immune thrombocytopenia, B12/folate deficiency, infections (e.g. HIV, EBV, tuberculosis)
- Medications (e.g. chemotherapeutic agents, valproic acid, mycophenolate mofetil)
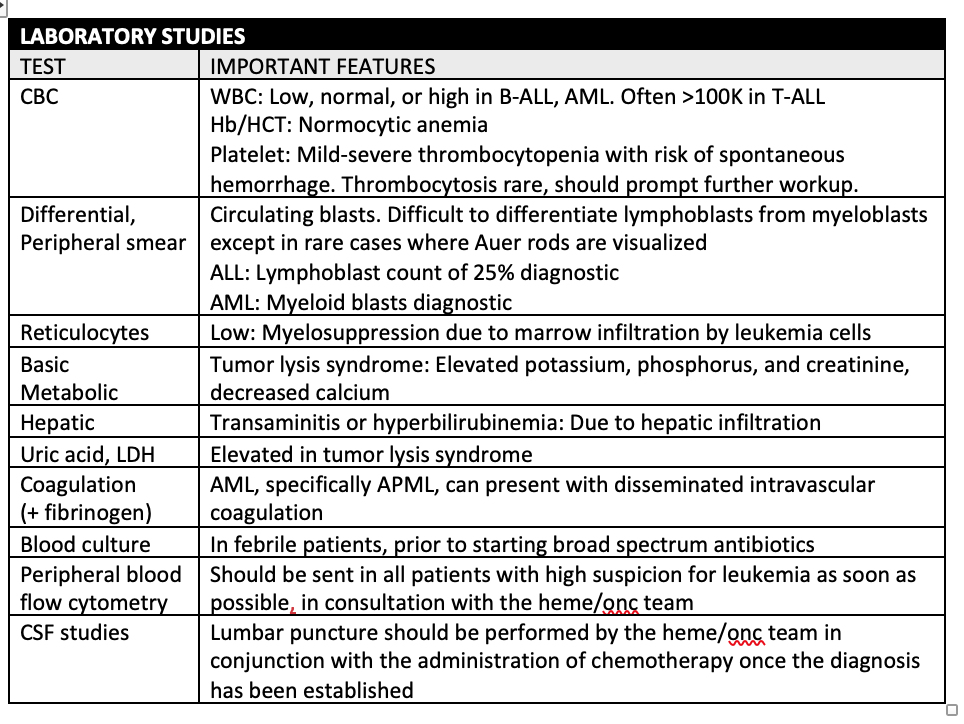
Laboratory Studies:
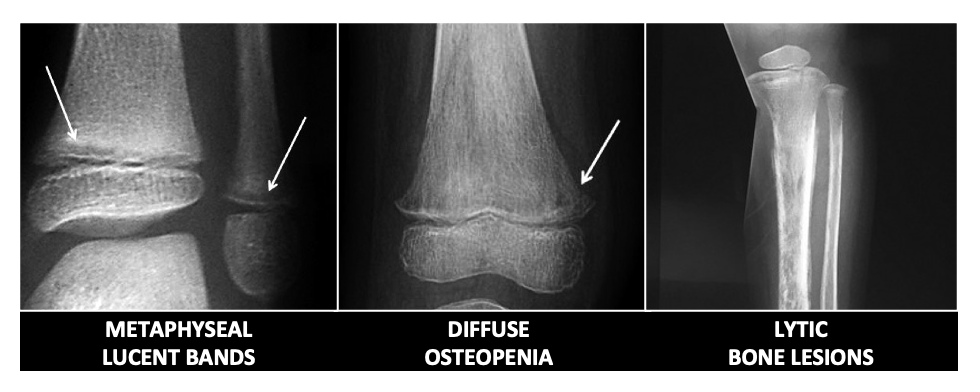
Radiographic Studies:
- Chest imaging (either plain films or CT) is useful when there is concern for mediastinal mass
- Head imaging can be obtained when there is concern for intracranial involvement
- Bony radiographs can show metaphyseal radiolucent bands, subperiosteal new bone formation, and osteolytic lesions of the cortex and medullary cavity
Management and Disposition:
- ED management for patients with suspected leukemia involves consultation with pediatric hematology/oncology specialists, as well as management of complications (see table). Febrile patients should receive broad-spectrum antibiotics
- Patients with high suspicion for leukemia should be admitted for further evaluation and management
References:
- Elgarten CW, Aplenc R. Pediatric acute myeloid leukemia: updates on biology, risk stratification, and therapy. Curr Opin Pediatr. 2020 Feb;32(1):57-66. doi: 10.1097/MOP.0000000000000855. PMID: 31815781.
- Hunger SP, Mullighan CG. Acute Lymphoblastic Leukemia in Children. N Engl J Med. 2015 Oct 15;373(16):1541-52. doi: 10.1056/NEJMra1400972. PMID: 26465987.
- Madhusoodhan PP, Carroll WL, Bhatla T. Progress and Prospects in Pediatric Leukemia. Curr Probl Pediatr Adolesc Health Care. 2016 Jul;46(7):229-241. doi: 10.1016/j.cppeds.2016.04.003. Epub 2016 Jun 6. PMID: 27283082.
- Lyengar V, Shimanovsky A. Leukemia. [Updated 2020 Aug 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560490/
