Definition
- Legg-Calve-Perthes Disease (LCPD) is a pediatric hip disorder exemplified by idiopathic avascular necrosis (AVN) of the femoral head
- Sometimes referred to as Coxa Plana, it is named after its most characteristic finding, a pathognomonic “flattening” of the femoral head
- It belongs to a group of disorders known as the “Osteochondroses” categorized by degeneration and subsequent regeneration of the growing ends of bones (epiphyses).
- Named after a trio of physicians (Arthur Legg, Jaques Calve, and Georg Perthes), each of whom described the disease separately in the early 1900’s after the advent of x-ray imaging
Epidemiology
- Typically occurs between ages 4-9, but can affect individuals between ages 2-14
- There is a 4:1 predominance for the male population
- Occurs bilaterally in ~10% of cases
- Reported incidence ranges from 0.4-29 cases per 100K children
- It is associated with smaller stature and delay in skeletal maturity at the time of disease onset
Mechanism
- Femoral head AVN and resulting biomechanical/biological responses lead to a readily recognizable pattern of degenerative injury witnessed on imaging. The exact trigger for its development remains unknown.
-
- Initial Stage:
-
-
- Blood supply to the femoral head is disrupted with resulting bony necrosis
- Duration: occurs over several months
- Fragmentation Stage:
- Dead bone is resorbed, replaced by softer, woven bone
- Duration: occurs over 1-2 year period
- Bone loss causes collapse/deformity of the femoral head and associated structural reformations of the hip joint
- Reparation (Re-Ossification) Stage:
- Continued re-ossification of the ischemic epiphysis. generates formation of newer, stronger bone
- Duration: Occurs over years
- Healed Stage:
- Bone growth is complete
- Femoral head has reached its final shape/configuration
- Degree of deformity generally correlates with prognosis, along with an enduring altered biomechanical function
-
Clinical Presentation
- Most commonly presents with limp/antalgic gait due to decreased range of motion, particularly internal rotation and hip abduction. This typically occurs in the sub-acute phase, often experienced over weeks to months, frequently dismissed as “growing pains.”
- Pain usually mild/absent in the early stages, but often located in hip/groin region as disease progression occurs. Some patients may only experience distal medial thigh pain (”referred pain”) with respect to articular branches of the obturator nerve.
- Symptoms generally worsen with exercise/weight-bearing activity and are relieved with rest.
- Patients may also complain of muscle spasms and/or hip stiffness.
- Atrophy of thigh muscles from disuse and leg length discrepancy can additionally be witnessed (hip adduction contractures may exacerbate this disparity).
- Rarely, similar symptoms may appear following trauma.
Imaging
- Early stages of disease typically exemplify “normal” hip imaging.
- Plain radiographic changes can be delayed versus clinical onset of symptoms, thus MRI/bone scans may be performed for expedited diagnosis.
- Waldenstrom Classification (Figure 1) describes LCPD radiograph progression.
-
- Initial Stage:
- The ossific nucleus fails to grow, appearing small, dense and uniform.
- Cartilage of the femoral head continues to grow causing medial joint space to appear widened.
- Femoral head may shift laterally in the acetabulum.
- Fragmentation Stage:
- Crescent (Caffey’s) Sign (Figure 2): linear lucency parallel to articular surface of the femoral head; indicates subchondral fracture.
- Epiphysis becomes fragmented, with an increased widening of joint space.
- This results in flattening/widening of the femoral head (Coxa Plana) and it becomes indistinct.
- Reparation (Re-ossification) Stage:
- Normal bone density returns.
- A short and broad femoral neck (Coxa Magna) becomes apparent.
- The flattened shape of the femoral head now becomes distinct.
- Healed Stage:
- Findings depend on severity of disease, ranging from a “nearly normal” appearance, to severe flattening of the femoral head articular surface +/- head/neck widening.
- Initial Stage:
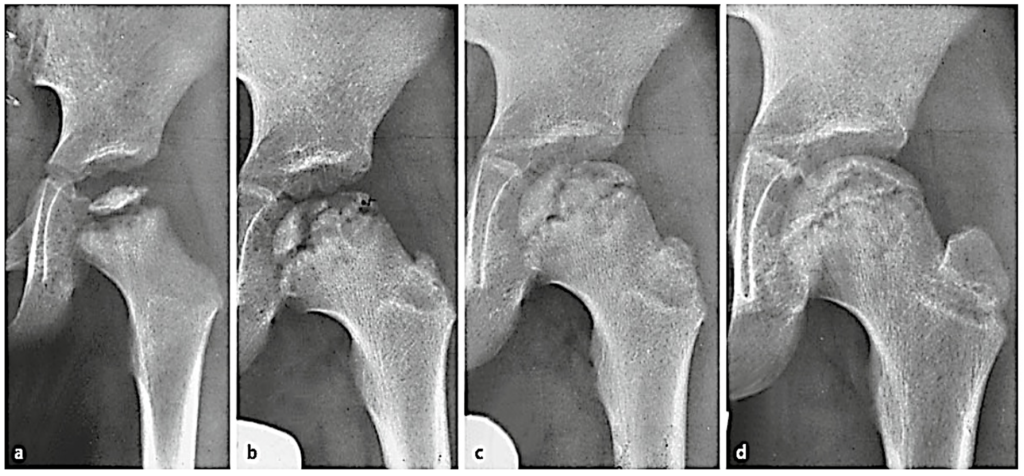
Figure 1. LPCD radiographic progression according to the Waldenstrom Classification: a) initial stage, b) fragmentation stage; c) reparation stage; d) healed stage. (Hefti, 2015)
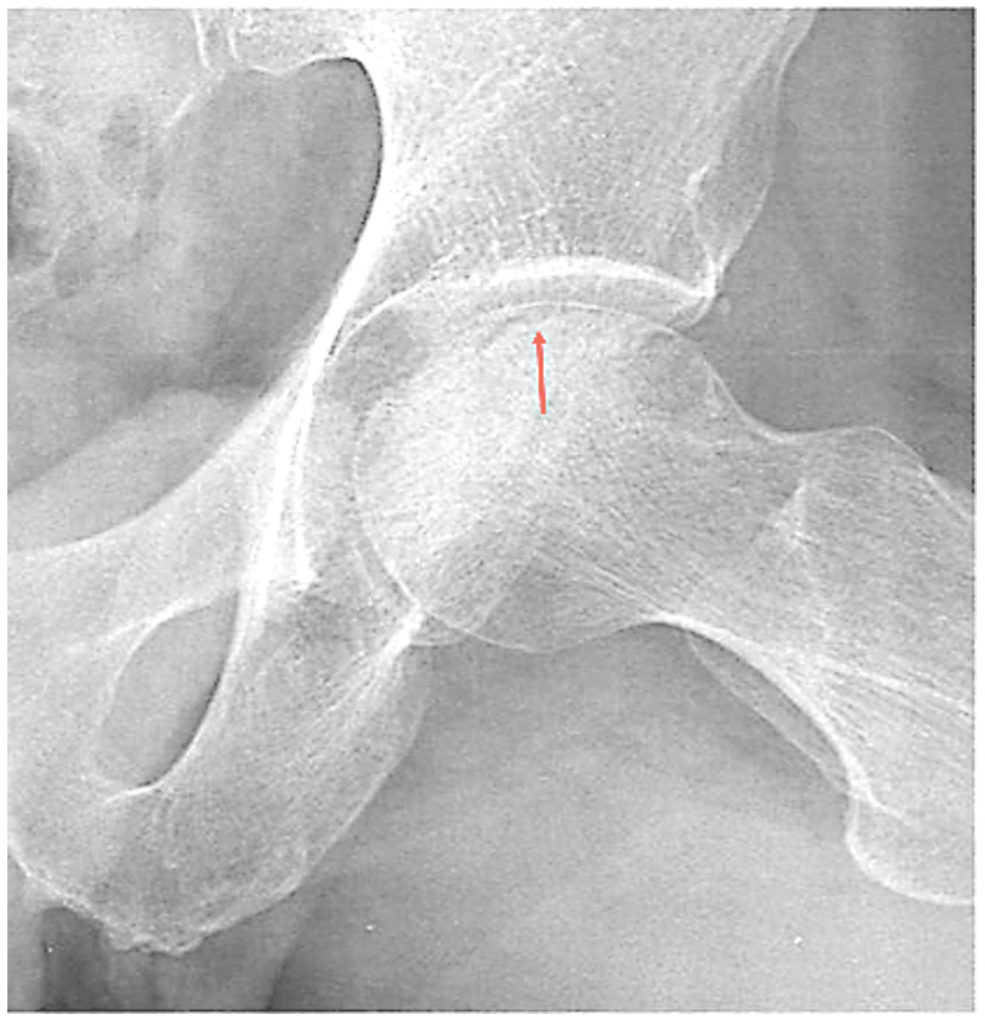
Figure 2. Crescent (Caffey) Sign: heralds the fragmentation stage. (radiopaedia.org)
Classification
- There are multiple classification systems, yet the Lateral Pillar (Herring Classification)system has demonstrated the best agreement and associated predictive value. However, this classification is employed during the fragmentation stage, thus it cannot be implemented regarding prognostic value.
- Categories are determined by the amount of involvement of the lateral pillar of the femoral head on Hip AP radiographs:
-
- Category A: No involvement of lateral pillar (normal height).
- Category B: Greater than 50% lateral pillar height maintained.
- Category C: Less than 50% lateral pillar height maintained.
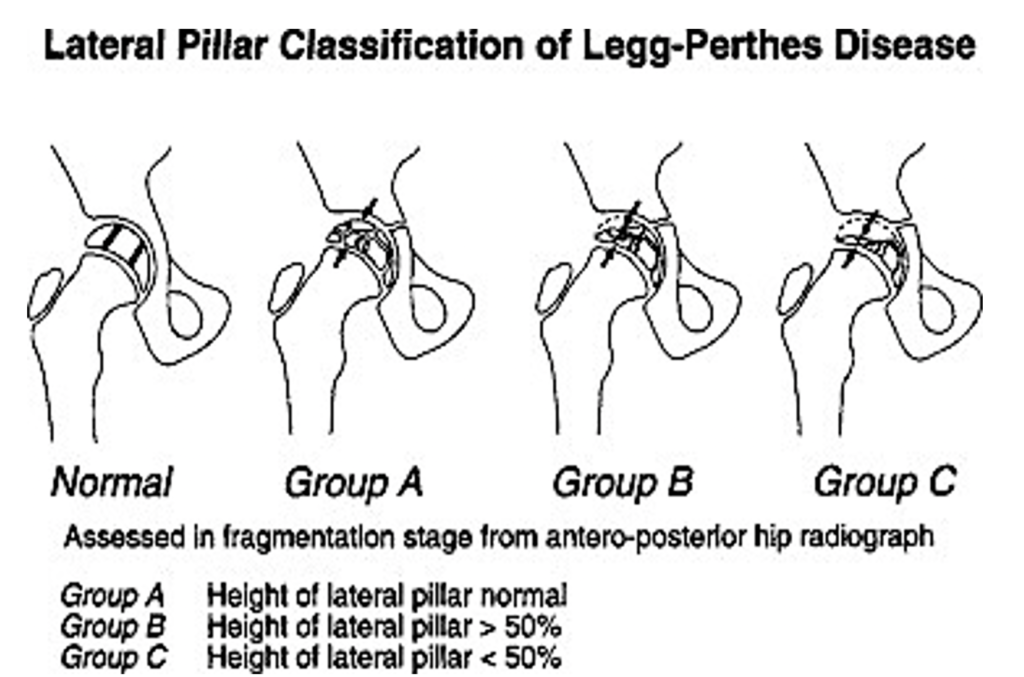
Figure 3: Lateral Pillar (Herring) Classification. Shapiro, F. (2002). Pediatric orthopedic deformities. Elsevier.
ED Management
- Obtain AP Pelvis, AP/Lateral views of the affected hip.
- Exclude other causes of hip pain, including infection/fracture, as this is a diagnosis of exclusion.
- Patients presenting with “knee pain” should have a full examination of the hip joint, as it may be the source of their symptoms.
- Provide adequate analgesia.
- Counsel patients to limit physical activity, reduce repetitive high impact movements.
- Patients may remain weight bearing, however short-term use of crutches can be used for pain relief/off-loading the affected extremity.
- Provide close orthopedic follow-up as some patients require bracing, surgery, and/or other modes of therapeutic intervention to diminish/prevent long-term complications.
Prognosis
- Goals of management are to reduce the incidence of osteoarthritis/associated long-term complications.
- Single best prognostic indicator of outcome is age at onset-younger age of onset is correlated with a decreased severity of disease.
- This concept is centered upon a greater time frame for bone revascularization/remodeling, allowing the femoral head to recover/remain spherical following disease resolution.
- Correspondingly, an increased deformity of the femoral head has been identified in those with patients that tend to develop more severe osteoarthritis.
Take-Home Points:
- Consider Legg-Calve-Perthes disease in any pediatric patient presenting with a antalgic gait/limp and/or hip, thigh or knee pain.
- Exclude other causes of hip pain prior to LCPD diagnosis.
- Initial x-rays may be “normal”, but follow a characteristic disease progression.
- Goals of treatment are to diminish pain, maintain active hip motion, and prevent/minimize potential permanent femoral head deformity to reduce development of degenerative arthritis.
- Treatment is aimed at minimizing damage throughout the LCPD process, not “curing”the disease.
- Close orthopedic follow-up is required to assist in managing disease onset, monitoring expected course of structural/functional changes and provide treatment and potential interventional guidance.
References
Hefti, F. (2015) Pelvis, hips and thighs. In: Pediatric Orthopedics in Practice. Springer, Berlin, Heidelberg.
Kim, H.K. and Herring, J.A. (2011). Pathophysiology, classifications, and natural history of Perthes disease. Orthop Clin North Am, 42 (3): 285 – 295.
Loder, R.T. and Skopelja, E.N. (2011). The epidemiology and demographics of legg-calvé-perthes’ disease. ISRN Orthopedics, 2011:1-14.
Purcell, D. et al. Emergency Orthopedics Handbook. Springer. 2019.
Shapiro, F. (2002). Pediatric orthopedic deformities. Elsevier.
Sharieff, G.Q. (2018). Pediatrics. In: Sherman SC. eds. Simon’s Emergency Orthopedics, 8e New York, NY: McGraw-Hill.
Stulberg, S.D., Cooperman, D.R., & Wallensten, R. (1981). The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am, 63(7), 1095-108.
Tintinalli, J. (2015). Tintinalli’s emergency medicine A comprehensive study guide. McGraw-Hill Education.