Definition: A life-threatening adverse reaction resulting from local anesthetic reaching significant systemic circulating levels. LAST is rare and almost always occurs within minutes of injection of the local anesthetic.
Causes
- Injection of local anesthetic into the systemic circulation (either errantly as part of a regional block i.e. Bier block)
- Rapid absorption of local anesthetic injected into a highly vascular area
- Use of local anesthetic doses in excess of the maximum dose (typically occurs with multiple subcutaneous injections)
- Common implicated procedures: bronchoscopy, circumcision, tumescent liposuction. Consider diagnosis in any patient coming from outpatient surgical center with cardiac arrest
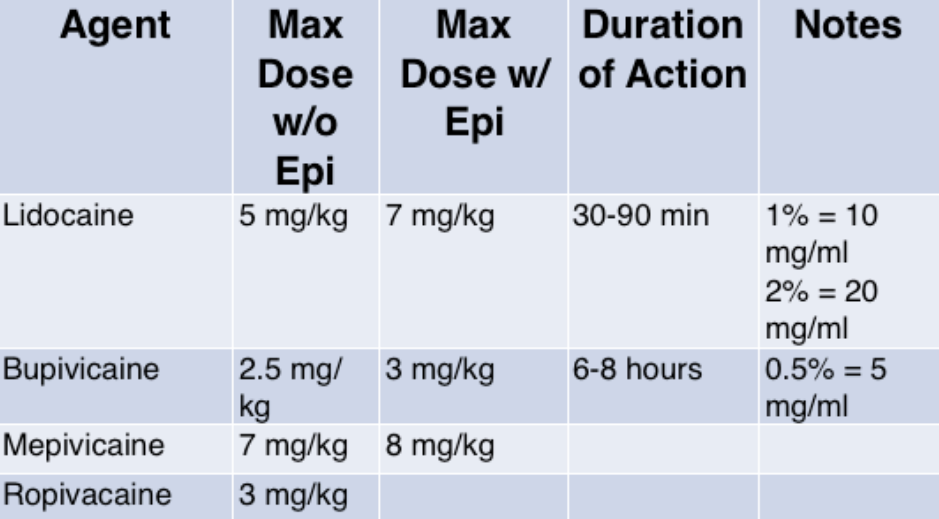
Commonly Used Anesthetics
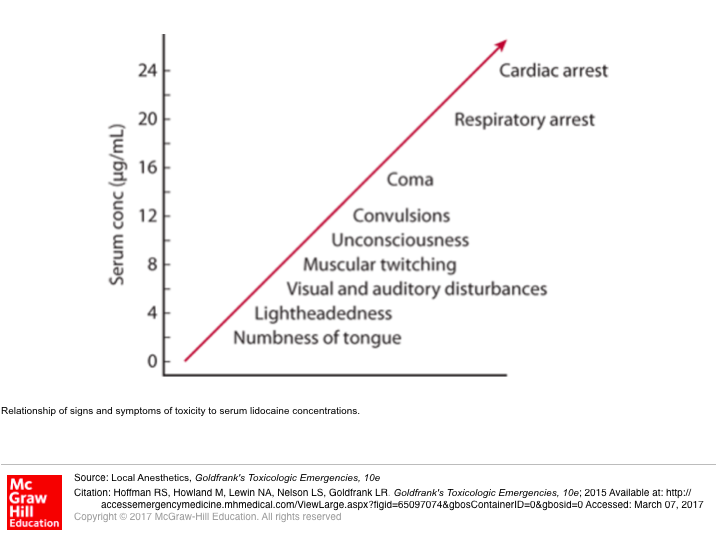
Relationship of Signs + symptoms of Lidocaine Toxicity to Serum Concentration
Signs + Symptoms
- CNS Symptoms
- Minor Signs/Symptoms
- Tongue and perioral numbness
- Parasthesias
- Restlessness
- Tinnitus
- Muscle fasciculations + tremors
- Major Signs/Symptoms
- Tonic-clonic seizures
- Global CNS depression
- Decreased level of consciousness
- Apnea
- Neurologic symptoms typically precede cardiovascular symptoms in lidocaine toxicity
- Minor Signs/Symptoms
- Cardiovascular Symptoms
- Early Signs: Hypertension and tachycardia
- Late Signs
- Peripheral vasodilation + profound hypotension
- Sinus bradycardia, AV blocs
- Conduction defects (Prolonged PR, Prolonged QRS)
- Ventricular dysrhythmias
- Cardiac arrest
- Cardiovascular symptoms typically present first in bupivacaine toxicity
Differential Diagnosis
- Anaphylaxis (rare with amide anesthetics)
- Effect of other sodium channel blockers (i.e. antihistamines, TCAs, cocaine, antimalarials)
- Anxiety
Management
- Prevention of toxicity
- Know + calculate maximum doses of local anesthetic agent prior to use
- Always aspirate prior to injection to ensure drug is not delivered intra-arterial or intravenous
- Ask patient about symptoms after injection
- Consider serial repairs of large or multiple wounds to minimize chance for toxicity
- Basic Management
- Institute basic management if ANY sign/symptom is present after local anesthetic use (i.e. new perioral numbness; don’t wait for CV findings!)
- Stop injection or infusion of agent
- Establish IV access if not already present
- Continuous cardiac monitor
- Aggressive Supportive Care
- Airway/Breathing
- Toxicity worsened by hypercapnea, hypoxia and acidosis
- Use 100% FiO2
- Hyperventilate
- Cardiovascular Collapse
- Consider epinephrine to augment cardiac output and improve peripheral vascular tone
- Consider bicarbonate infusion for severe acidosis
- Initiate high-quality CPR in arrest
- Manage seizures with benzodiazepines over propofol as propofol is a cardiac depressant (Goldfrank’s 2015)
- Airway/Breathing
- Lipid Emulsion Therapy (20% Intralipid)
- Mechanism of action: unclear. May act as lipid sink, may facilitate redistribution of local anesthetic from target organs
- Utility in lidocaine vs. bupivacaine
- Due to lidocaine short 1/2 life, may be unnecessary. CPR alone typically adequate
- Bupivacaine has longer 1/2 life making intralipid more useful in this form of LAST
- Dosing (Neal 2012, Cao 2015)
- Bolus: 1 – 1.5 ml/kg over 1 min
- Can repeat bolus every 3 minutes up to a total dose of 3 ml/kg
- Infusion: 0.25 ml/kg/min
- Continue infusion until hemodynamically stable for at least 10 minutes
- Can increase infusion to 0.5 ml/kg/min if BP worsens
- Bolus: 1 – 1.5 ml/kg over 1 min
- Continue CPR during infusion to circulate drug
Take Home Points
- The key in managing LAST is prevention. Know your dose, know your maximum dose, always aspirate prior to injection and ask patient about symptoms
- Lidocaine toxicity CV complications are typically preceded by neurological signs/symptoms. If these develop, stop administration, place patient on monitor and ready your antidote
- Bupivacaine toxicity can be sudden and catastrophic. If you are using the drug, undershoot your max dose and know where your antidote is
- Intralipid has been shown to be effective in LAST. Administer the drug anytime there are signs of hemodynamic compromise
References:
Schwartz DR, Kaufman B. Local Anesthetics. In: Hoffman RS, Howland M, Lewin NA, Nelson LS, Goldfrank LR. eds. Goldfrank’s Toxicologic Emergencies, 10e New York, NY: McGraw-Hill; 2015. Link
Neal JM et al, American Society of Regional Anesthesia and Pain Medicine. American Society of Regional Anesthesia and Pain Medicine checklist for managing local anesthetic systemic toxicity: 2012 version. Reg Anesth Pain Med 2012;37:16–8. PMID: 22189574
Cao D et al. Intravenous lipid emulsion in the emergency department: a systematic review. J Emerg Med 2015; 48(3): 387-97. PMID: 25534900

regarding vasopressors in the resus stage of LAST:
according to NYSORA
“experimental evidence involving animals has shown worsened outcomes when combined with lipid emulsion, perhaps due to increased myocardial intracellular acidosis. “