
Neck of Femur Classification (http://www.oxfordmedicaleducation.com/)
Definition: Fracture in the proximal femur, between the lesser trochanter and greater trochanter.
Mechanism
- Elderly: > 90% are from a low energy fall (Egol 2010)
- Young: Typically a high-energy trauma, such as a motor-vehicle accident or fall from a height
Epidemiology
- Intertrochanteric fractures account for about 50% of proximal femur fractures (Egol 2010)
- Female to male ratio is 3:1, likely due to bone density changes in post-menopausal women (UptoDate 2017)

Hip Fracture Physical Exam (image.wikifoundry.com)
Physical Exam
- Non-displaced fracture
- Patients may have minimal pain
- Patients may be ambulatory despite presence of fracture
- Displaced fractures
- Pain in lower extremity
- Non-ambulatory
- Affected leg is shortened and externally rotated
Fracture Types
- Stable vs Unstable
- Stable
- Posteromedial cortex is intact or minimal comminution
- When load is applied, intact cortex will prevent external rotation and varus displacement
- Unstable
- Disruption of posteromedial cortex
- Comminution of posteromedial cortex
- Subtrochanteric extension
- Reverse obliquity fracture: fracture line proximally from medial cortex distally to lateral cortex
- Stable
- Occult Fracture
-
- Fracture not visible on plain X-rays
- Requires advanced imaging to diagnose
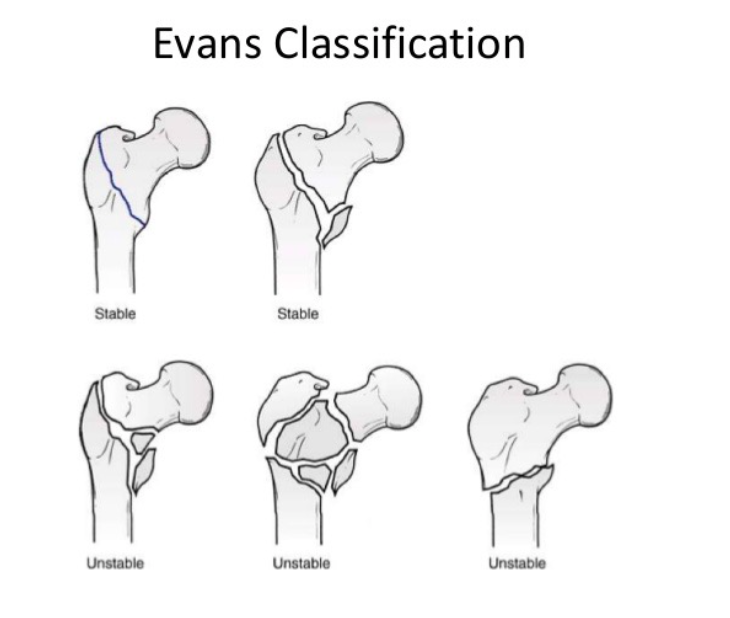
Evans Classification (https://image.slidesharecdn.com)

Intertrochanteric Fracture AP X-ray (Case courtesy of Dr M Osama Yonso, Radiopaedia.org. From the case rID: 16317)
Diagnostic Imaging
- X-Ray
- Required views: AP Pelvis, AP and cross table lateral Hip, AP Femur
- Will demonstrate fracture between the greater and lesser trochanter, with/out extension into the subtrochanteric region
- Occult Fractures
- X-rays will miss about 10% of hip fractures
- Of all hip fractures, 8% are identified by CT scan but missed on X-ray
- About 2% of all hip fractures are missed on X-rays and CT scan, but seen on MRI
- Advanced Imaging (CT and MRI)
- Consider if X-Rays are negative but patient is unable to bear weight or physical exam is concerning for fracture
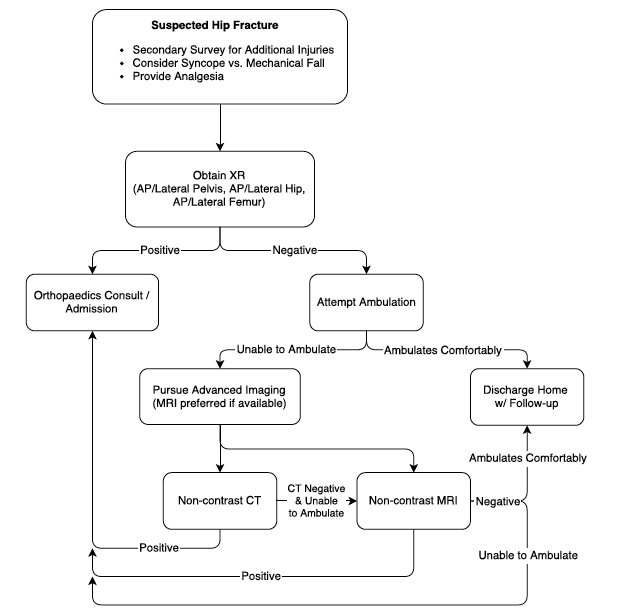
Hip Fracture Imaging Algorithm
X-ray Images

AP X-ray Intertrochanteric Fracture (Case courtesy of Dr M Osama Yonso, Radiopaedia.org. From the case rID: 21352)

Intertrochanteric Fracture (Case courtesy of Dr M Osama Yonso, Radiopaedia.org. From the case rID: 21352)

AP Pelvis X-Ray Intertrochanteric Fracture (Case courtesy of Dr Pir Abdul Ahad Aziz, Radiopaedia.org. From the case rID: 47715)

Oblique Pelvis X-ray Intertrochanteric Fracture (Case courtesy of Dr Pir Abdul Ahad Aziz, Radiopaedia.org. From the case rID: 47715)
ED Management
- Analgesia
- Femoral nerve block
- Pros
- Easy to perform by landmark or ultrasound technique
- Provides analgesia without systemic effects
- Cons: Does not provide analgesia to lateral thigh
- Pros
- Femoral nerve block
-
- Fascia iliaca compartment block
- Pros
- Injection away from nerve and artery reducing complications
- Provides analgesia to lateral thigh
- Cons: Requires larger volume of anesthetic
- Pros
- Fascia iliaca compartment block
-
- Systemic analgesia typically provided with opiates/opioids
- Assess for secondary injuries
- Assess for additional fractures
- Consider head and cervical spine trauma in all patients
- Consider complications from fall (i.e. prolonged immobility on ground)
- Investigate cause of fall (i.e. mechanical fall vs. syncope)
- Monitor blood loss
- About 40% of patients with hip fractures require blood transfusions (Desai 2014)
- Patients with intertrochanteric fractures are twice as likely to need blood transfusion as those with a femoral neck fracture
- Non-operative
- Pursued for patients at very high-risk of perioperative mortality or non-ambulatory at baseline
- Non-weight bearing
- Goal: Early bed to chair mobilization to prevent complications such as pneumonia, VTEs, ulcers
- Operative
- Stable: Sliding hip screw
- Unstable: Intramedullary hip screw or arthroplasty
Prognosis
- 1 year mortality: 20-30% (Brauer 2009)
- Mortality higher than in femoral neck fracture (Haentjens 2007)
- Increased mortality associated with
- Age over 85
- Pre-existing medical conditions or ASA classification III and IV
- Male
- Operative delay for more than 2 days
- Low rates of non-union and malunion, because of extensive blood supply
Take Home Points
- Occult fractures are common. A negative X-ray with a high clinical suspicion should be followed by a CT and/or MRI
- Do not forget to assess for secondary injury and monitor blood loss
- Provide adequate analgesia with a regional nerve block or opioids
- It is important to diagnose hip fractures early because there is a high mortality rate with delay in operative management
Read More
Orthobullets: Intertrochanteric Fractures
UptoDate: Hip Fractures in Adults
Highland EM Ultrasound: Femoral Block
Ultrasound Podcast: Lower Extremity Nerve Block Mastery with Mike Stone!
References
Egol KA et al. Handbook of Fractures. Lippincott Williams & Wilkins; 2010. Link
Desai SJ et al. Factors affecting transfusion requirement after hip fracture: can we reduce the need for blood?. Can J Surg. 2014;57(5):342-8. PMID 25265109
Brauer CA et al. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573-9. PMID 19826027
Haentjens P et al. Survival and functional outcome according to hip fracture type: a one-year prospective cohort study in elderly women with an intertrochanteric or femoral neck fracture. Bone. 2007;41(6):958-64. PMID 17913614