Urinary Tract Infections/Pyelonephritis
Epidemiology:
- Occurs in as many as 15% of pregnant women and between 20-40% of pregnant women with asymptomatic bacteriuria will progress to pyelonephritis (Gorgas 2008)
Management:
- Uncomplicated UTI
- Suggested antibiotics include:
- Nitrofurantoin 100mg PO BID x7 days OR
- Cephalexin 500mg PO BID x7 days
- Pyelonephritis
- Hospital admission
- Suggested antibiotics include:
- Ceftriaxone 1g IV Q24H OR
- Aztreonam 2g IV Q8H for beta-lactam allergy
- Suggested antibiotics include:
Complications:
- Maternal sepsis
- Maternal renal injury
- Congenital abnormalities of the fetus
- Premature rupture of membranes
- Low birth weight
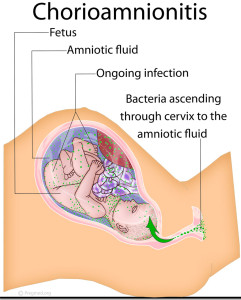
Chorioamnionitis
Definition: Also known as intraamniotic infection. Chorioamnionitis is a bacterial infection of fetal amnion and chorion membranes.
Epidemiology
- Occurs in 1 to 10% of all pregnancies (Gorgas 2008)
- Incidence increases significantly with preterm labor
Diagnosis
- Chorioamnionitis is defined as maternal fever >38°C and at least two of the following (Apantaku and Mulik 2007):
- Maternal tachycardia >100 beats/min for five minutes
- Fetal tachycardia >160 beats/min for five minutes
- Purulent or foul-smelling amniotic fluid or vaginal discharge
- Uterine tenderness
- Maternal leukocytosis
Evaluation (Abbrescia 2003)
- CBC
- Blood cultures
- Vaginal fluid for phosphatidylglycerol
- Tests for fetal lung maturity
- Cervical AND vaginal cultures
- Physical Exam
- Avoid digital cervical exam
- Speculum exam should be done with sterile speculum
- Ultrasonography for fetal well being
Management
- Given concern for neonatal sepsis, patients should be admitted for IV antibiotics, supportive cares, and possible early delivery
- Most commonly an ascending infection from normal vaginal flora, so antibiotics must be chosen to cover polymicrobial infections
- Ampicillin IV 2g Q6H AND Gentamicin IV 1.5mg/kg Q8H
- In PCN allergic patient substitute vancomycin 1 g IV Q12H for ampicillin
- Can only be considered cured with delivery of infected products of conception
Complications
- Placental abruption
- Premature birth
- Neonatal sepsis
- Neonatal death
- Cerebral palsy
- Maternal sepsis
- Need for cesarean delivery
- Postpartum hemorrhage
Postpartum Endometritis
Definition: Generalized uterine infection
Epidemiology
- Sepsis results in 15% of maternal deaths worldwide (Houry 2014)
- More common in surgical than vaginal deliveries
- May co-exist with surgical site infection
Diagnosis
- Classic triad includes: fever, lower abdominal pain and uterine tenderness, and foul smelling lochia
Management
- Hospital admission
- Cover for polymicrobial infection, including anaerobes
- Clindamycin 900 mg IV Q8H AND Gentamicin 5-7 mg/kg IV Q24H
Septic Abortion
Epidemiology:
- The World Health Organization estimates that one in eight pregnancy related deaths worldwide can be directly attributed to unsafe abortion procedures (Gorgas 2008)
Diagnosis:
- Clinical presentation includes fever, abdominal pain and uterine tenderness in setting of recent abortion
- Presentation can vary from mild infection to septic shock
Evaluation:
- Lactate
- Cultures of cervix, blood and urine
- Coagulation panel to screen for DIC
- Abdominal X-ray to evaluate for free air or retained surgical foreign bodies
- Pelvic ultrasound to evaluate for retained products of conception or surgical foreign bodies
Management:
- Hospital admission may be indicated as infection can progress to septic shock, organ failure, DIC and cardiovascular collapse
- Broad-spectrum antibiotics are indicated. Triple antibiotic coverage is recommended. Suggested regimens include:
- Ampicillin AND
- Gentamicin AND
- Clindamycin OR Metronidazole
- Update tetanus vaccination
- Usually requires dilation and curettage to remove any retained products of conception or foreign bodies.
References:
Abbrescia, K. and B. Sheridan (2003). “Complications of second and third trimester pregnancies.” Emerg Med Clin North Am 21(3): 695-710, vii. PMID: 12962354
Apantaku, O. and V. Mulik (2007). “Maternal intra-partum fever.” J Obstet Gynaecol 27(1): 12-15. PMID: 17365450
Desai, S. and S. Henderson. Labor and Delivery and Their Complications. In: Marx, J et al, ed. Rosen’s Emergency Medicine. 8th ed. Philadelphia, PA: Elsevier Saunders; 2014:2331-2350.
Gorgas, D. L. (2008). “Infections related to pregnancy.” Emerg Med Clin North Am 26(2): 345-366, viii. PMID: 18406978
Houry, D and B. Salhi. Acute Complications of Pregnancy. In: Marx, J et al, ed. Rosen’s Emergency Medicine. 8th ed. Philadelphia, PA: Elsevier Saunders; 2014: 2282-2299.