Epidemiology:
- Prevalence of in-flight emergencies: 1 in 604 flights from literature review between 2008-2010 of five domestic and international airlines representing 10% of the global passenger volume at that time
- Types of in-flight emergencies when a single cause could be identified:
- Syncope/near syncope (32.7-37.4%)
- GI including nausea/vomiting (9.5-14.8%)
- Respiratory including asthma exacerbations (10.1-12.1%)
- Cardiovascular (7.0%) including cardiac arrest (0.2%)
- Other (Psych/intox, allergy, ob/gyn, other/unknown)
- In-flight emergencies rely on one large decision point: can the flight continue to its intended destination or does the situation require alternative landing plans, aka “diversion”?
- Physician passengers provide medical assistance in approximately 48% of in-flight medical emergencies
- When in-flight emergencies occur, the pilot staff consult with an on-ground aviation medical team to assist with decision making regarding diversion
- Flight attendants are trained in CPR and AED use
- 4-7.3% of in-flight emergencies required diversion (about 1 in 8,300 flights)
- Approximately 25% need post-flight transportation to a hospital
- 6% of all in-flight emergencies required hospitalizations with a mortality of 0.3%
- Most common admission criteria included possible strokes, respiratory distress, and cardiac symptoms
Pathophysiology:
- Passenger cabins (pressurized to 11-12 PSI) can cause volumes of gas to expand by up to 30% and can trigger discomfort in closed systems, physiologic gas-containing spaces of the body (sinuses, middle ear) or non-physiologic potential spaces (pneumothorax, potential spaces created following GI/ocular/intracranial surgery)
- Partial pressure of oxygen decreases at altitude (in healthy patients: as large a drop in mean arterial oxygen saturation as 93% from 97%)
- Weak case report and small-powered VTE risk profile analyses suggest increased platelet activation/venous stasis in conjunction with non-insignificant hypoxia as etiology of increased VTE risk
First Aid/Emergency In-Flight Medical Kits:
- FAA Code of Regulations, Title 14, part 121 subpart X Section 121.803
- 1 kit for 0-50 passengers; 2 kits for 51-150 passengers; 3 kits for 151-250 passengers; 4 kits for 250+ passengers
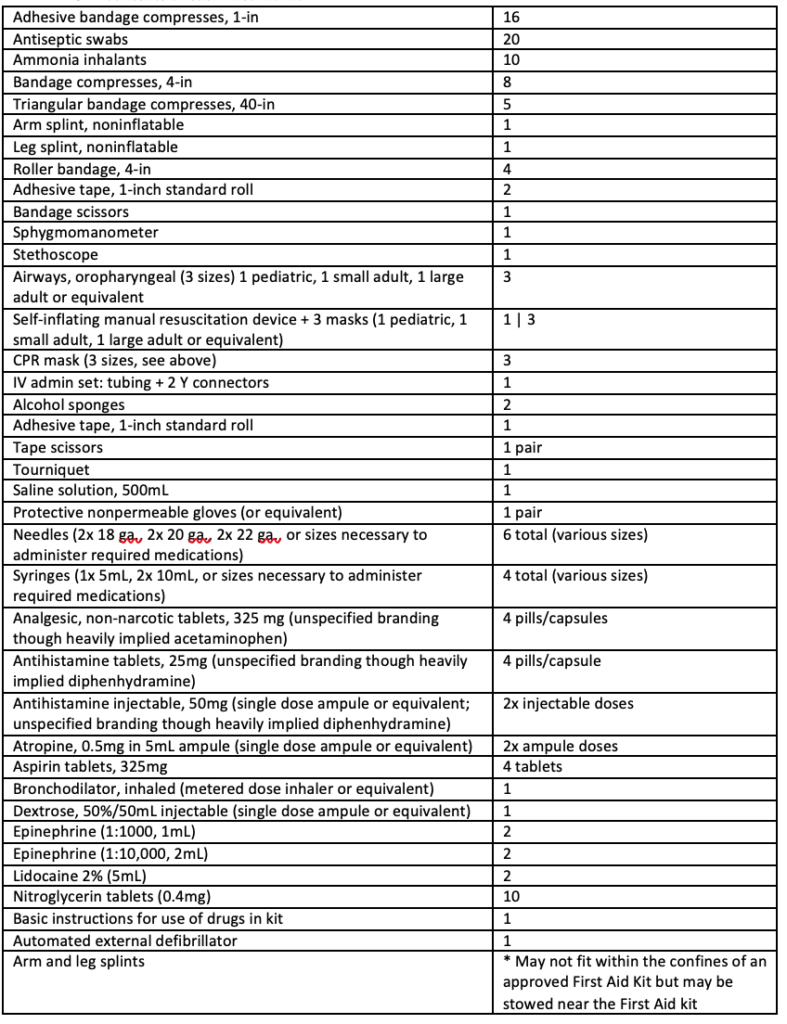
- Contents of each kit below (notice absence of pediatric or obstetric supplies)
Good Samaritan Law:
- In the United States, physicians are under no legal obligation to assist in in-flight medical emergencies
- The Aviation Medical Assistance Act (1998) provides Good Samaritans with protection from lawsuits alleging negligence “unless the individual, while rendering such assistance, is guilty of gross negligence or willful misconduct”
- For example, a physician passenger could be considered grossly negligent if the physician was intoxicated due to alcohol or sedative ingestion on the flight
- Of note, the physician provider must receive no monetary compensation: do not accept upgrades, travel vouchers, or travel miles
- The Aviation Medical Assistance Act also protects American airline companies from liability in seeking physician provider assistance if the flight crew “in good faith” believes the provider is medically qualified
- Intercontinental flights rely on the laws of the country in which the airline is based
- For example, Australia, France, and Germany legally mandate that physicians provide aid (or else face fines or prison)
References:
https://jamanetwork.com/journals/jama/fullarticle/2719313 (Meta-analysis of epidemiology/pathophysiology of in-flight emergencies)
https://www.cmaj.ca/content/164/7/1037.long (postulation of VTE risk profiles in air travel)
https://www.cordem.org/globalassets/files/curricular-toolkit/good.samaritan/good.samaritan.laws.summary.handout.pdf
https://onlinelibrary.wiley.com/doi/10.1111/j.1538-7836.2010.03819.x
https://www.dovepress.com/medical-issues-in-flight-and-updating-the-emergency-medical-kit-peer-reviewed-fulltext-article-OAEM (The Emergency Medical Kit)
https://www.law.cornell.edu/cfr/text/14/121.803 (FAA Guidelines on Emergency Medical Equipment)
https://www.nejm.org/doi/10.1056/NEJMoa1212052?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200www.ncbi.nlm.nih.gov (Outcomes of in-flight medical emergencies)