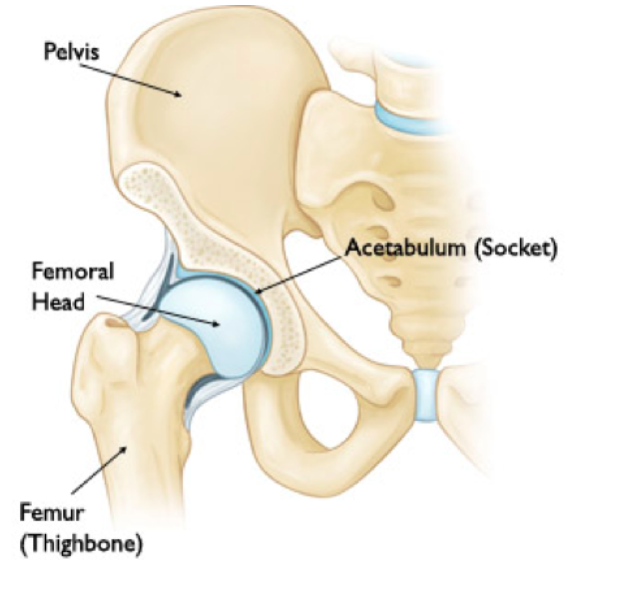
Hip Anatomy (http://www.health.act.gov.au/)
Definition: Separation of the femoral head from the acetabulum of the pelvis in either a posterior or anterior direction.
Classification and Mechanism
- Anatomic
- Anterior Dislocation (10%)
- Occurs with axial loading of hip in extension and abduction or from a significant posterior force on the joint forcing the femoral head anteriorly.
- Can be shifted inferiorly (extension > flexion) or superiorly (flexion > extension)
- Posterior Dislocation (90%)
- Occurs with axial loading of hip in flexion and adduction. dashboard injury where the patient’s knee hits the dashboard/steering wheel in flexion and forces the femoral head posteriorly.
- Anterior Dislocation (10%)
- Complexity: Stewart-Milford System (Egol, 2010)
| Type I | Simple dislocation without a fracture. |
| Type II | Dislocation with one or more rim fragments but with sufficient socket to ensure stability after reduction. |
| Type III | Dislocation with fracture of the rim producing gross instability |
| Type IV | Dislocation with fracture of the head or neck of the femur |
Mechanistic Considerations
- As the femoral head dislocates, it can injure the femoral neurovascular bundle
- Diminishes blood supply to the femoral head leading to avascular necrosis
- Avascular necrosis can develop within 6 hours stressing the need for prompt identification and reduction (Hougaard 1986)
- Reduction < 6 hours: 4.8% avascular necrosis
- Reduction > 6 hours: 52.9% avascular necrosis
Epidemiology
- Uncommon injury, typically secondary to trauma or in non-native joints
- Traumatic
- 70% of all hip dislocations are dunne to motor vehicle collisions
- Relatively rare in younger individuals, with only 5% occurring in individuals less than 14 years old (typically sports or fall- related). (Goodwin, 2011)
- Post-Hip Arthroplasty
- Dislocation one of the most common complications after arthroplasty, occurring due to laxity, implant positioning, improper implant choice and impingement. (Kendoff, 2013)
- Frequency: (Eysel 2014) (Weatherford, 2011)
- 2% after primary total hip arthroplasty
- 28% after revision and implant exchange surgeries
- 70% of dislocations occur within the first month and 75-90% posterior
- Traumatic
- Associated with other injuries in up to 95% of traumatic cases (Goulet, 1999)
- Acetabular fractures (70%)
- Other extremity fractures (39%)
- Closed head injuries (24%)
- Craniofacial injuries (21%)
- Thoracic injuries (21%)
- Femoral head fractures (14%)
Physical Exam
- General
- Severe pain
- Inablity to move the affected lower extremity
- Hip Exam
- Anterior Dislocation: mildly flexed, abducted and externally rotated
- Posterior Dislocation: flexed, adducted and internally rotated
- Special Considerations
- Complete a full trauma survey given frequency of associated injuries
- Direct particular attention to ipsilateral joints given the large force transmitted through the lower extremity to cause the dislocation
- Ipsilateral knee, patellar and femur fractures are common co-injuries
- Meniscal and PCL injuries are common with dashboard type injuries
- Complete a full neurovascular exam
- Sciatic nerve injuries occur in up to 10% of cases.
- Check dorsiflexion of the ankle and large toe (will be weak in anterior and posterior dislocations)
Imaging Modalities
- Initial imaging should include a plain hip with AP pelvis
- If suspicion for associated fracture, subsequent CT is recommended to fully characterize the injury .
- If a fracture is present, your orthopedics colleagues may prefer to manage the injury operatively and any closed manipulation may cause injury to surrounding neurovascular structures.
- Posterior Dislocation

Posterior Hip Dislocation (Case courtesy of Dr Hani Salam, Radiopaedia.org. From the case rID: 10397)
- Anterior Dislocation
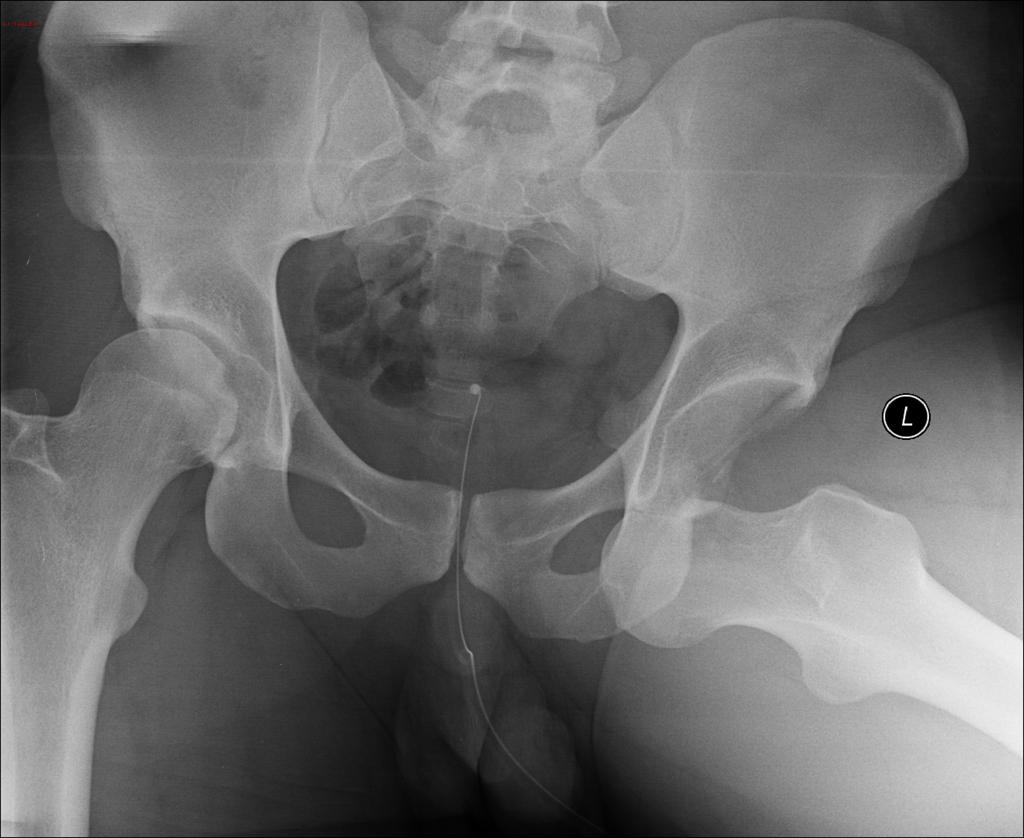
Anterior Hip Dislocation (Case courtesy of Dr Sajoscha Sorrentino, Radiopaedia.org. From the case rID: 14836)
- Concomitant Fracture
- Common in traumatic dislocations but may be difficult to visualize with X-rays
- CT scan superior imaging modality if concern for fracture
- Fracture of the anterior articular surface of the femoral head (black arrow)
- Fracture of the posterior margin of the acetabulum (green arrow)
- Fragment of bone (grey arrow) in the soft tissues posterior to the acetabulum, which had arisen from the posterosuperior femoral head
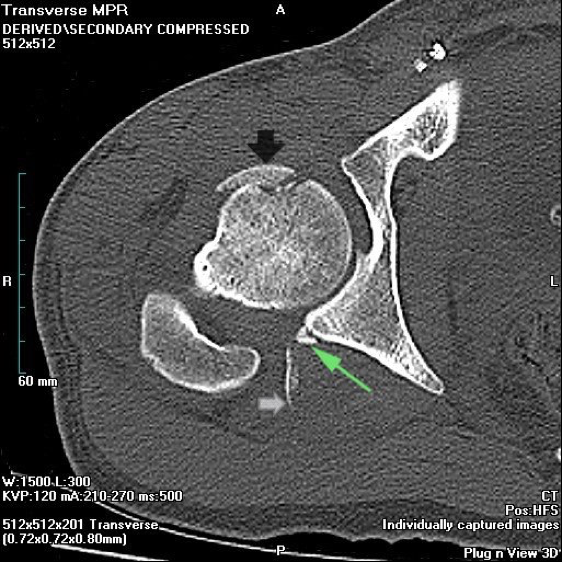
Fracture of Femoral Head with Dislocation (http://www.radpod.org)
Management
- Closed Reduction
- Urgent reduction (<6 hours) should be performed in most cases to reduce the risk of osteonecrosis
- If there is an associated hip/femoral neck fracture, the patient may require closed reduction under anesthesia or an open reduction in the OR
-

Allis Maneuver (Waddell 2016)
Closed Reduction Techniques (Meyer, 2016)
- Allis Maneuver
- Place the patient supine in the bed with the physician either on the bed (as shown) or standing beside the patient
- While an assistant stabilizes the pelvis, hold the ipsilateral leg just below the knee, flex it to 90 degrees and apply traction in line with the femur
- As the hip begins to reduce, extend the hip and externally rotate to allow the femoral head to slide back into the acetabulum
- Allis Maneuver
-

Bigelow Maneuver (Waddell 2016)
Bigelow Maneuver
- Place the patient in the supine position with the physician standing beside the bed
- Place your forearm beneath the patients knee and grasp the ankle with your opposite hand (as shown)
- While an assistant stabilizes the pelvis, flex the hip to 90 degrees and apply traction in line with the femur while abducting, externally rotating and extending the hip until reduced
-

Rochester Maneuver (Waddell 2016)
Rochester/Whistler Maneuver
- Place the patient in the supine position with both legs flexed and the physician at the standing beside the bed
- Slide your arm beneath the knee of the affected side and then hold the knee of the contralateral side
- Place your hand on the ankle of the affected leg and apply downward traction at the ankle, internally and externally rotating as needed
-

Stimson Gravity Maneuver (Waddell 2016)
Stimson Gravity Maneuver
- Place the patient in a prone position with the legs over the side of the bed in 90 degrees flexion
- Place one hand on the patient’s ipsilateral calf, just below the knee, and the under beneath the ipsilateral ankle (as shown)
- Apply downward force on the lower extremity using the hand on the calf and use the hand on the ankle to apply internal/external rotation until the hip is reduced
- Captain Morgan
- Place the patient in a supine position with the pelvis stabilized by and assistant or strapped to the bed
- Stand on the side of the patients bed and place your knee, flexed at 90 degrees, beneath the patients ipsilateral leg, just distal to their knee (as shown)
- Place your forearm beneath the patients knee and grasp the ankle with your opposite hand (as shown)
- Apply upward traction with the hand behind the patient’s knee and internally/externally rotate at the ankle until the hip is reduced
- Open Reduction
- Reduction in the OR
- Consider in cases of irreducible dislocation, evidence of incarcerated fragments, unstable fracture-dislocation, delayed presentation (>6-12 hrs) or if the reduction is not concentric. (Bhandari, 2012)
- Post-Reduction Management
- Imaging
- A post-reduction X-ray should be obtained in all cases (native or non-native) and a CT is recommended in traumatic cases of dislocation to rule out fracture.
- Post-Discharge Care
- Exercise Precautions (non-fractured):
- Controlled passive range-of-hip motion exercises and early mobilization
- Extremes of motion should be avoided for 4-6 weeks to allow for capsular and soft-tissue healing
- Anterior: avoid hyperextension of the hip with external rotation
- Posterior: avoid flexion of the hips past 45 degrees
- Weight-bearing
- Institution specific
- No associated fracture: Generally full weight-bearing as tolerated
- Associated fracture: depends on surgical vs. non-surgical management by orthopedics
- Immobilization
- Anterior: an abduction pillow may be helpful
- Posterior: use a simple knee immobilizer
- Exercise Precautions (non-fractured):
- Imaging
- Complications:
- Osteonecrosis resulting from avascular necrosis
- Chronic Pain/Arthritis
- Post-traumatic arthritis can occur in up to 37.5% of patients with traumatic hip dislocation. (Srikrishnamurthy, 1983)
Take Home Points
- Early identification and reduction is key to prevent complications
- Always perform a full trauma and neuro exam, particularly of ipsilateral joints as concomitant injuries are common with traumatic dislocations
- Don’t be reassured by negative post-reduction XRs as small fractures can occur. You should always consider CT
Read More
ALiEM: PV Card: Hip Injuries
Orthobullets: Hip Dislocation
EMin5.com: Hip Dislocations
Radiopedia: Hip Dislocation
Sanders S et al. Traumatic hip dislocation–a review. Bull NYU Hosp Jt Dis. 2010;68(2):91-6. PMID: 20632983
Kovacevix D et al. Injuries about the hip in the adolescent athlete. Sports Med Arthrosc. 2011 Mar. 19 (1): 64-74. PMID: 21293240
Zahar A et al. Dislocation after total hip arthroplasty. Current Reviews in Musculoskeletal Medicine. 2013;6(4):350-356. PMID: 24170479
Dargel J et al. Dislocation Following Total Hip Replacement. Deutsches Ärzteblatt International. 2014;111(51-52):884-890. PMID: 25597367
Weatherford, B (2011, November). Hip Dislocation. Retrieved from http://www.orthobullets.com/recon/5012/tha-dislocation
Hak DJ1, Goulet JA. Severity of injuries associated with traumatic hip dislocation as a result of motor vehicle collisions. J Trauma. 1999 Jul;47(1):60-3. PMID: 10421188
Hougaard K, Thomsen PB. Traumatic posterior dislocation of the hip – prognostic factors influencing the incidence of avascular necrosis of the femoral head. Arch Orthop Trauma Surg. 1986;106:32-35. PMID: 3566493
Upadhyay SS et al. An analysis of the late effects of traumatic posterior dislocation of the hip without fractures. J Bone Joint Surg Br. 1983 Mar;65(2):150-2. PMID: 6826619
Waddell BS et al. A Detailed Review of Hip Reduction Maneuvers: A Focus on Physician Safety and Introduction of the Waddell Technique. Orthopedic Reviews. 2016;8(1):6253. PMID: 27114811
Bhandari, M. Evidence-based Orthopedics. Chichester: Wiley Blackwell, 2012. Web.
This is very helpfull.
Thank you