Introduction:
- Hand, foot, and mouth disease (HFMD) is common in children, especially those younger than 10 years of age.
- Many cases are caused by coxsackievirus A16 (a member of the enterovirus group) and enterovirus A71, although there are many different serotypes.
- Some of these serotypes, including coxsackievirus A6, may cause more severe symptoms.
- While most cases occur during the summer and early fall months, the disease can be seen year-round.
- Because HFMD is spread through both direct contact and droplets, it is common in the pediatric population.
Differential Diagnosis:
The distinguishing features of the differential diagnoses are as below:
- Viral pharyngitis: pharyngitis without vesicles
- Herpangina: pharyngeal lesions only
- Herpetic gingivostomatitis: lesions more common on lips and gums, with severe pain
- Aphthous stomatitis: mucosal ulcers, not associated with viral symptoms
- Varicella zoster: lesions at different stages of healing
- Kawasaki disease: CRASH and burn (usually accompanied by conjunctivitis, adenopathy, hand/ foot changes, and cracked lips/ strawberry tongue)
- Henoch-Schonlein Purpura: non-blanching rash located primarily on buttocks and legs
- Measles: cephalocaudal spread, rash preceded by viral prodrome with three C’s, ill-appearing
- Erythema multiforme: targetoid rash more common
- SJS/ TEN: ill-appearing, with both skin and mucous membrane involvement
Clinical Manifestations:
- Patients with HFMD may have general viral symptoms, including fever, decreased oral intake, odynophagia, and general malaise.
- Herpangina refers to the painful blisters in the posterior pharynx.

- Patients may also experience erythematous lesions (including macules, papules, pustules, and vesicles) on their palms and soles (hence the name); however, the rash may also be widespread and can be mistaken for conditions such as varicella.

- In rare cases, enteroviruses can cause CNS manifestations such as encephalitis, aseptic meningitis, acute transverse myelitis, and Guillain-Barre syndrome.
Management:
- For the majority of patients, treatment is supportive.
- NSAIDs and Tylenol are useful for the treatment of pain.
- Magic mouthwash (a combination of a 1:1:1 ratio of liquid Benadryl, Maalox/Mylanta, and viscous lidocaine) can be helpful for herpangina.
Disposition:
- Most patients will be discharged with supportive care. As HFMD is highly contagious, they should limit their contact with others as much as possible while symptomatic.
- Those with CNS manifestations should be admitted for further management.
Sequelae:
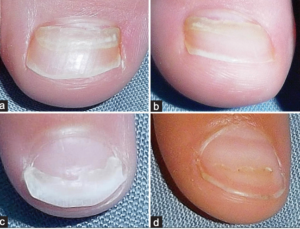
- Patients with coxsackievirus may experience onychomadesis, or separation of the proximal nail plate from the nail matrix.
- Although this is a benign finding, it can be distressing to parents, and they should be warned in advance.
References:
- Guerra AM, Orille E, Waggoner BC, et al. Hand Foot And Mouth Disease. [Updated 2020 Aug 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431082/Jubelt B, Lipton HL. Enterovirus/picornavirus infections. Handb Clin Neurol. 2014;123:379-416. doi: 10.1016/B978-0-444-53488-0.00018-3. PMID: 25015496.
- Kim EJ, Park HS, Yoon HS, Cho S. Four cases of onychomadesis after hand-foot-mouth disease. Ann Dermatol. 2014;26(6):777-778. doi:10.5021/ad.2014.26.6.777
- Mao Q, Wang Y, Yao X, Bian L, Wu X, Xu M, Liang Z. Coxsackievirus A16: epidemiology, diagnosis, and vaccine. Hum Vaccin Immunother. 2014;10(2):360-7. doi: 10.4161/hv.27087. Epub 2013 Nov 14. PMID: 24231751; PMCID: PMC4185891.
Images:
- https://www.cdc.gov/features/handfootmouthdisease/index.html
- https://en.wikipedia.org/wiki/Herpangina
- Dobrev H, Hristova R. A case of onychomadesis following hand, foot, and mouth disease. Our Dermatology Online 1.2016. p101.
