Background
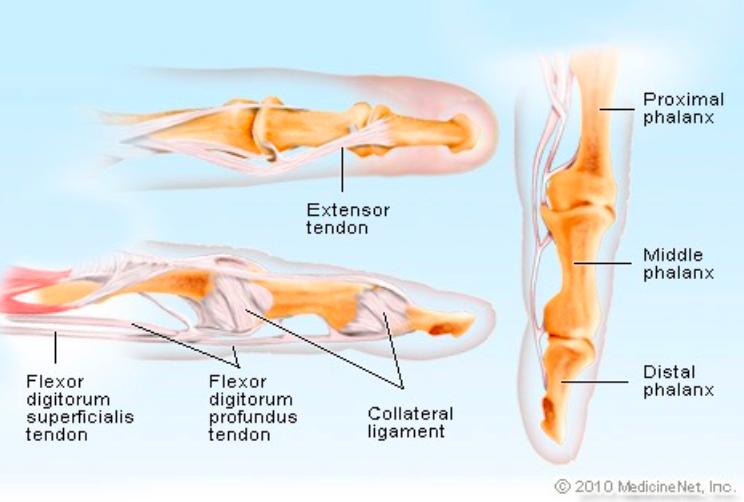
Finger Anatomy (medicinenet.com)
- Routine assessment of tendon/ligament function is important in all patients with finger trauma: significant injury can occur even in the absence of fracture.
- Important tendon and ligament groups of the finger:
- Extensor digitorum (dorsal aspect of finger)
- Flexor digitorum superficialis and profundus (volar aspect of finger)
- Collateral ligaments (radial and ulnar aspects of finger)
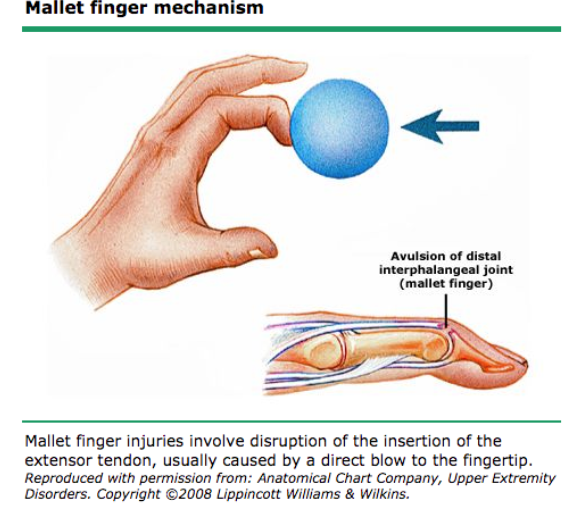
Mallet Finger Mechanism (uptodate.com)
Extensor Mechanisms of Injury (“Finger Pointing Down”/Volar)
- Mallet Finger
- Definition: Disruption of the extensor tendon insertion into the dorsal aspect of the distal phalanx
- Mechanism: Forced flexion of the DIP joint by either a traumatic blow to the distal phalanx or crush injury to the dorsal finger
- Epidemiology
- 5.6% of all tendon/ligament injuries to the hand/wrist (Botero 2016)
- Occurs frequently during manual labor or sports
- Younger males (high-energy mechanism) and older females (low-energy mechanism) are most commonly injured.
- Middle, ring, and small finger are most frequently involved
- Physical Exam
- DIP held in 45 degrees of flexion at rest
- Unable to actively extend
- Tenderness along dorsal aspect of the finger
- Doyle Classification
- Type I: tendon-only rupture
- Type II: open
- Type III: open with deep soft tissue injury
- Type IV: associated fracture
- A: distal phalanx physis (peds)
- B: 20-50% articular surface
- C: >50% articular surface
-

Mallet Finger with Avulsion Fracture (Schwartz)
Xray Findings
- Usually DIP in flexion with no associated fracture.
- If avulsion fracture fragment present, will see it at dorsal base of distal phalanx
- Usually DIP in flexion with no associated fracture.
- ED Management
- Type I: DIP Joint Immobilization for 6-10 weeks with no flexion
- Joint Immobilization for 6-10 weeks
- Can apply dorsal or volar splint with full extension of DIP joint – maintain with no flexion
- No difference in outcomes between variety of splints as long as full extension is maintained (Valdes 2015)
- Orthopedic follow-up in 1-2 weeks
- Type II/III
- Emergent surgical repair of open wound
- Prophylactic antibiotics: first generation cephalosporin + gentamicin
- Type IV
- Usually requires surgical pinning (either closed reduction and percutaneous pin fixation or ORIF) to prevent complications
- Splint in extension as with Type I injuries
- Ensure follow-up scheduled within 1 week
- Type I: DIP Joint Immobilization for 6-10 weeks with no flexion
-
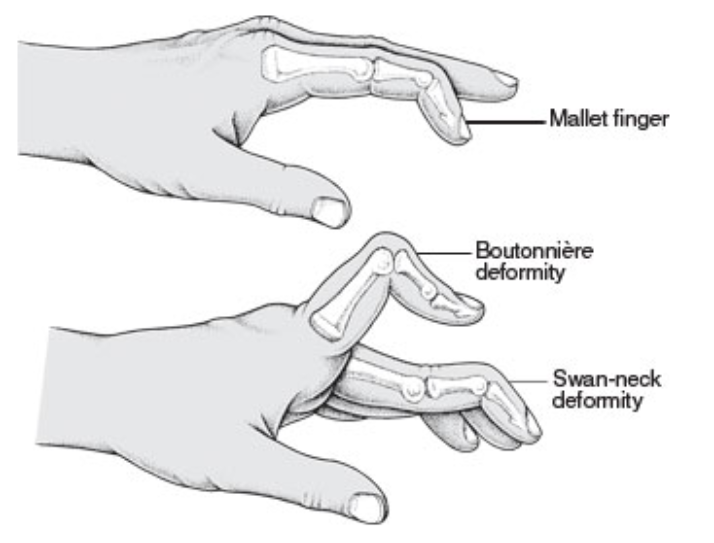
Swan-Neck Deformity
Prognosis
- If not properly treated, can result in a swan-neck deformity, with hyperextension at PIP and flexion at DIP as the lateral bands become laterally displaced. Ensure patients understand that any flexion at DIP joints sets them back to day 1 (Perron 2001)
- Even properly treated patients may have a perpetual extensor lag of up to 10 degrees
- Boutenneire Deformity
- Definition: “buttonhole” gap when extensor digitorum central slip is disrupted and the lateral bands displace volarly (Scalcione 2012) (Figure 10)
- Mechanism: forced extension of PIP while in rigid extension or volar dislocation at PIP joint (“jammed” finger)
- Epidemiology: most commonly seen in basketball players or martial artists
- Physical Exam
- Finger held in flexion at PIP and hyperextension at MCP and DIP
- In acute stage (<2 months), exam findings may be subtle
- Perform the Elson test
- Patient’s PIP in 90 degrees flexion (central band taut and lateral bands loose)
- Ask patient to extend PIP while applying pressure to middle phalanx
- Normal = active extension at PIP (DIP stays loose)
- Abnormal = no active extension at PIP (DIP taut and extended to lift finger)
- In chronic stage, classic deformity becomes more obvious and contracture does not allow for active or passive extension at PIP
- Classification (Scalcione 2012)
- Stage 1: 10-15 degrees flexion at PIP with ability to passively correct
- Stage 2: 30-40 degrees flexion with ability to passively correct but start of joint contracture
- Stage 3: >40 degrees flexion and joint destruction
-
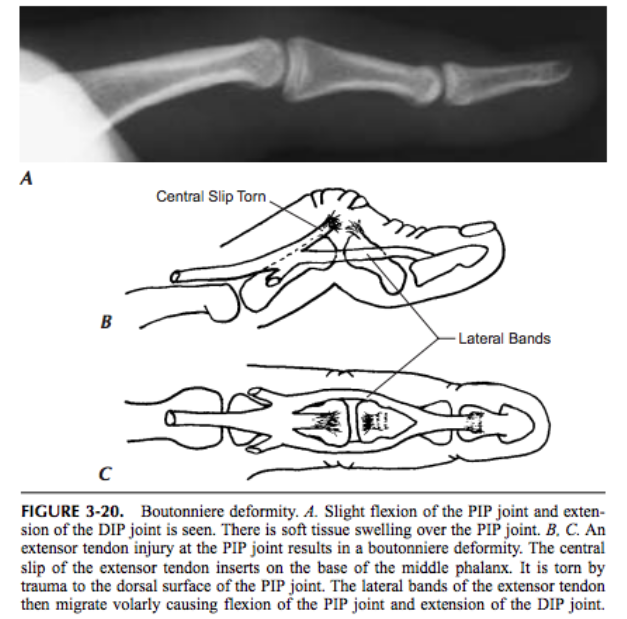
Xray of Boutounneire Deformity (Schwartz)
X-Ray Findings
- Flexion at PIP, extension at DIP
- Non-urgent MRI as outpatient can confirm the diagnosis
- ED Management
- Acute Injury
- Splint PIP joint in extension for 6 weeks leaving MCP and DIP free to move to prevent contracture
- Have patient follow up in 1-2 weeks
- Chronic Injury
- Splint if possible but may be unable to fully extent at PIP
- Refer to orthopedist for attempt at non-operative management and possible surgical repair
- Surgical indications: open wound (emergent surgery with prophylactic antibiotics), acute avulsion fracture from middle phalanx, or chronic injury remaining after 6 weeks in splint
- Acute Injury
- Prognosis
- If diagnosed during acute phase, can avoid permanent deformity
- If missed, difficult to correct without surgical intervention.
Jersey Finger
- Definition: Disruption of the flexor digitorum profundus tendon at insertion into the volar surface of the distal phalanx
- Mechanism: Forced extension (i.e. gripping a sports jersey)
- Epidemiology
- Much less common than mallet finger
- 75% involve ring finger because when gripping objects this fingertip is 5mm longer than others (Perron 2001)
- Physical Exam
- Finger held in slight extension with absence of active flexion at DIP (Figure 14)
- Loss of normal flexion cascade (Figure 15)
- Tenderness along volar aspect of finger
- Palpate volar surface of the entire metacarpal and phalanx to locate site of flexor tendon disruption, as retraction into the palm requires more urgent surgical repair
- Immobilize PIP to test isolated flexion at DIP
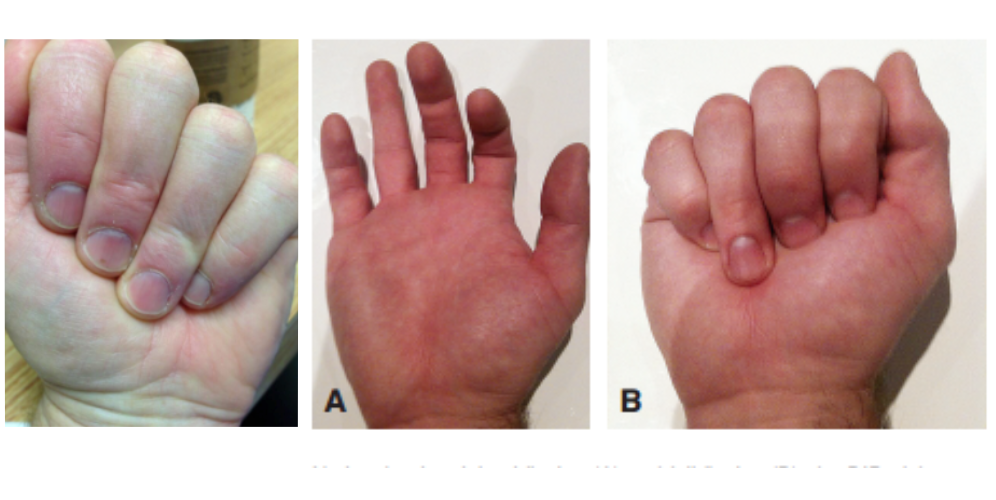
Jersey Finger (Normal vs. Abnormal Finger Cascade)
- Leddy + Packer Classification (Scalcione 2012)

Jersey Finger Splint (http://orthoinfo.aaos.org/)
- Type I: FDP retracted to palm
- Type II: FDP retracted to PIP joint
- Type III: Large fracture which limits retraction to DIP joint
- Type IV: Osseous fragment and avulsion of tendon from fracture
- Type V: Ruptured tendon with bone avulsion remaining attached to distal phalanx
- X-Ray Findings
- Avulsion of FDP tendon usually not visible but may see osseous avulsion fragments
- ED Management
- All require surgical repair
- Type I
- Surgical tendon repair within 1 week (level of retraction disrupts vascular supply)
- Ensure follow up scheduled within next 1-2 days
- Type II-V
- Surgical tendon repair within several weeks
- Follow up in 1 week
- Temporizing splint: dorsal splint with 30 degrees wrist flexion, 70 degrees MCP flexion, 30-45 degrees PIP and DIP flexion (Figure 17) (Perron 2001)
- Prognosis: Poor functional capacity without surgical repair
Collateral Ligament Injuries (Finger “Pointing Left/Right”)
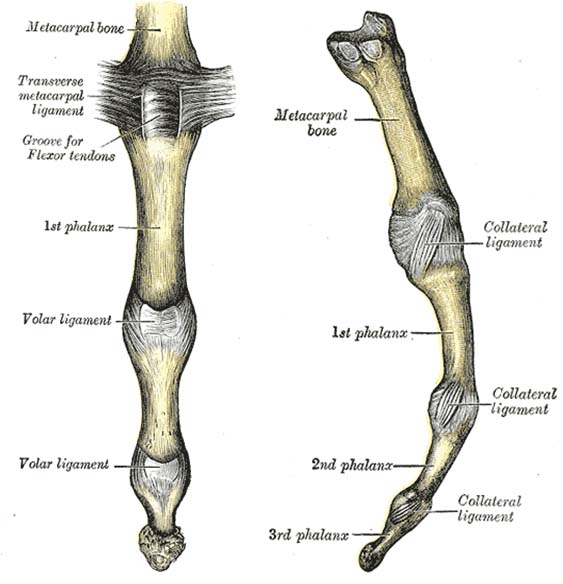
Digital Collateral Ligaments (teachmeanatomy.info)
- Digital Collateral Ligament
- Definition: Disruption of the radial or ulnar collateral ligaments
- Mechanism: Either “jammed” finger or dorsal/volar dislocation
- Epidemiology
- Majority (60%) involve the thumb (see Gamekeeper’s/Skier’s Thumb)
- 4th/5th digits: Most commonly involve radial collateral ligament
- 2nd digit: Most commonly involves ulnar collateral ligament
- 3rd digit: Equal involvement of radial and ulnar ligaments
- Physical Exam
- Unstable “pinch” mechanism: radial or ulnar deviation of distal phalanx when trying to pinch between thumb and affected finger
- Laxity to varus or valgus stress
- Xray Findings
- Rarely show significant abnormalities

Buddy Taping (Andrade)
- Stress views can be used to confirm to diagnosis: will see radial or ulnar “opening” of the joint space
- If clinical suspicion of injury is high, can treat without stress views
- Rarely show significant abnormalities
- ED Management (Andrade 2011)
- Buddy taping for 3 (simple tear) to 6 (complex tear) weeks
- Orthopedic follow-up in 1-2 weeks
- Surgical repair required for injury to radial collateral ligament of the index finger since absolutely required for pinching
- Prognosis: Persistent pain after conservative therapy may require surgical intervention
- Gamekeeper’s/Skier’s Thumb
- Definition: Injury to the ulnar collateral ligament at MCP of thumb
- Mechanism: Forceful radial deviation of the thumb
- Epidemiology
- Gamekeepers: Repetitive use injury (ex. breaking rabbit necks)
- Skiers: Acute injury (ex. thumb vs. fixed ski pole)
- Represents 86% of all injuries to base of thumb (Scalcione 2012)
- 60% of collateral ligament injuries (Scalcione 2012)

Radial Stress in Gamekeeper’s Thumb (Andrade)
- Physical Exam
- Thumb deviation of 35 degrees or 15 degrees further than unaffected thumb indicative of complete tear (Andrade 2011)
- May require digital block to appropriately stress
- Classification
- Partial tear: ligament remains partially attached
- Complete tear: ligament fully detached
- Stener lesion
- UCL retracts proximally and overlies the adductor tendon (major muscle tendon in the thumb)
- Proper healing prevented with this injury
- Xray Findings
- AP/lateral/oblique usually normal
- Stress views may be necessary
- If unable to see injury or obtain stress view, treat empirically
- MRI (96% sensitive and 95% specific) may be obtained as an outpatient
- ED Management:
- Partial tear: Thumb spica for 4 weeks
- Complete tear: Thumb spica with surgical repair within 3 weeks
- Schedule follow-up within 1 week
- Prognosis: If complete tear not repaired, possibility of adductor pollicus aponeurosis becoming stuck between the ruptured ends of the ulnar collateral ligament with permanent dysfunction
Take Home Points
- Ligament and tendon injuries can be subtle and require high clinical suspicion and thorough exam
- As with other orthopedic injuries, open injuries require emergency repair
- Examination of the affected finger may be limited by pain. Consider regional anesthesia to ensure a thorough examination or, empirically treat
- Appropriate ED management focuses on immobilization and timely orthopedic follow up – know which injuries require early consultation
Read More
ALiEM: Elson’s Test
Emergency Medicine Ireland: Anatomy for EM 035 – Hand Part 03
Emergency Medicine Ireland: Anatomy for EM 036 – Hand Part 04
Emergency Medicine Ireland: Anatomy for EM 037 – Hand Part 05
References
Botero SS et al. Review of Acute Traumatic Closed Mallet Finger Injuries in Adults. Arch Plast Surg. 2016;43(2):134-144. PMID: 27019806
Doyle JR. Extensor Tendon Acute Injuries. In: Greep DP, editor. Operative hand surgery. 3rd ed. New York: Churchill Livingstone. 1993;1950-87.
Valdes K, Naughton N, Algar L. Conservative Treatment of Mallet Finger: A Systematic Review. J Hand Ther. 2015;43(2):134-144. PMID: 26003015
Perron AD et al. Orthopedic Pitfalls in the Emergency Department: Closed Tendon Injuries of the Hand. Am J Emerg Med. 2001;19(1):76-80. PMID: 11146026
Scalcione LR, Pathria MN, Chung CB. The Athlete’s Hand: Ligament and Tendon Injury. Semin Musculoskelet Radiol. 2012; 16(4):338-349. PMID: 23047281
Weischhoff GG et al. Traumatic Finger Injuries: What the Orthopedic Surgeon Want to Know. Radiographics. 2016; 36(4):1106-1128. PMID:27399238
Andrade A, Hern HG. Traumatic Hand Injuries: The Emergency Clinician’s Evidence-Based Approach. Emerg Med Pract. 2011; 13(6):1-24. PMID: 22164514
Schwartz DT, Reisdorff EJ. Emergency Radiology. McGraw-Hill. 2000.