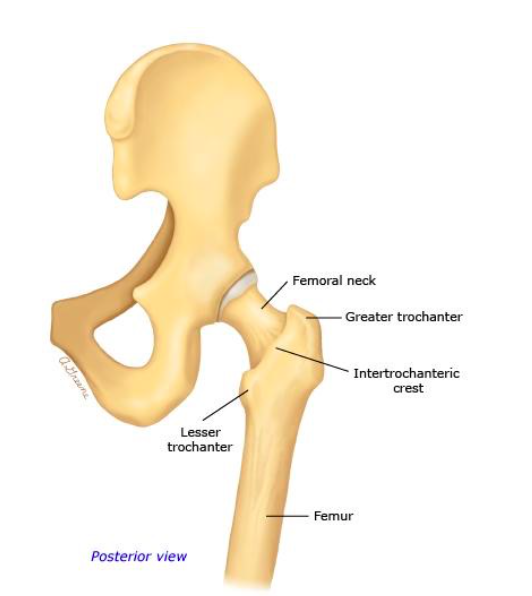
Hip Anatomy
Definition: Fracture of the proximal femur, through the neck, which connects the femoral head with the femoral shaft
Mechanism
- Elderly: Low energy fall is the most common cause
- Young: High energy trauma
Epidemiology (Skinner 2014, Egol 2015)
- Estimated 6.3 mil hip fractures worldwide by 2050
- 50% of hip fractures in US involve the femoral neck
- 80% women, 20% men
- Old>>Young
- White>Black
Fracture Classification Systems
- Pauwel – based on angle fracture forms with horizontal plane
- Garden – based on degree of valgus displacement
- Type I – Incomplete/Valgus Impacted
- Type II – Complete and nondisplaced on AP and lateral views
- Type III – Complete with partial displacement
- Type IV – Complete displaced
- For ED purposes, can simply classify as “displaced” or “nondisplaced”
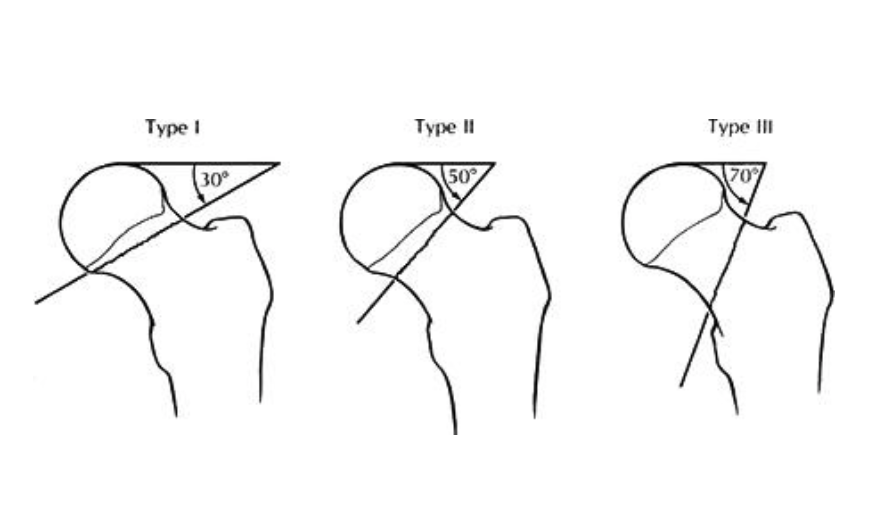
Pauwels’ Classification (intranet.tdmu.edu.ua)

Short and Externally Rotated (gurgaonkneeandshoulderclinic.com)
Physical Exam
- Examine the patient from head to toe looking for other areas of trauma
- Displaced fracture
- Leg shortened, externally rotated
- Non ambulatory
- Typically in considerable amount of pain in hip and/or groin area
- Nondisplaced fracture
- No deformity
- Patient may be ambulatory
- May complain of vague pain in hip, groin, buttocks, thigh, knee
- Perform a complete neurovascular exam focusing on distal pulses and sensation

Base of Right Femoral Neck Fracture (Case courtesy of Dr M Osama Yonso, Radiopaedia.org. From the case rID: 18409)
Diagnostic Imaging:
- Required radiograph views
- AP pelvis, AP and cross table lateral hip, AP/lateral femur
- Frog leg view contraindicated – may cause worsening displacement or displace a nondisplaced fracture
- Evaluation of X-Rays
- Look for disruption along Shenton’s Line
- Evaluate the neck-shaft angle (normal is 120-130 degrees)
- If X-rays negative, consider advanced imaging for occult fracture
- Up to 10% of hip fractures will be missed on X-ray
- Approximately 2% of occult hip fractures on X-ray and CT are identified on MRI (Hakkarinen 2012)
- MRI currently gold standard but new research suggests CT may be just as good (Thomas 2016)
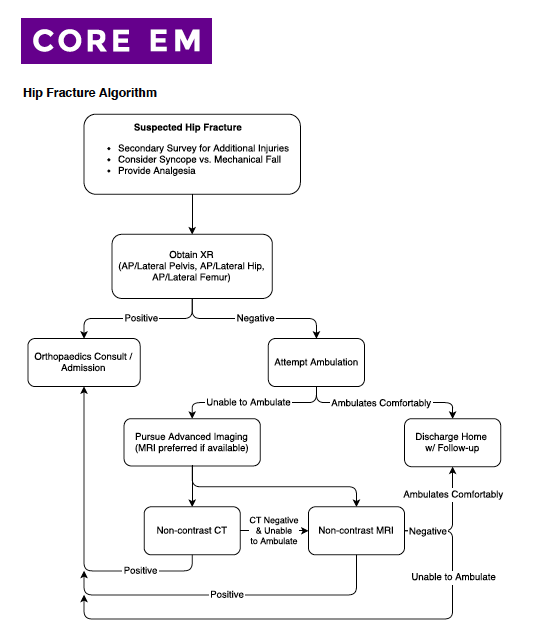
Hip Fracture Imaging Algorithm
Femoral Neck Fracture X-Rays

Base of Right Femoral Neck Fracture (Case courtesy of Dr M Osama Yonso, Radiopaedia.org. From the case rID: 18409)

Displaced Right Femoral Neck Fracture (Case courtesy of Dr Jeremy Jones, Radiopaedia.org. From the case rID: 6383)

Left Subcapital Fracture (Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 2717)

Base of Right Femoral Neck Fracture (Case courtesy of Dr M Osama Yonso, Radiopaedia.org. From the case rID: 18409)
ED Management
- Analgesia
- Systemic analgesia. Typically in form of parenteral opiate
- Nerve Block
- Consider ultrasound guided femoral nerve block and/or fascia iliaca compartment block
- Advantage: can provide significant reduction in pain without systemic effects often seen with opiates (i.e respiratory depression, nausea, hypotension)
- Medical Assessment
- Consider cause of fall
- Mechanical fall leading to trauma vs. syncope leading to fall
- Liberal use of EKG and tests evaluating for syncope beneficial
- Consider associated conditions
- Systemic infection
- Dehydration
- Rhabdomyolysis (especially if found down for unknown period of time)
- Consider cause of fall
- Assess for other injuries
- Consider head and neck trauma in all patients
- Consider other orthopedic injuries
- Orthopedic surgery consultation for operative management
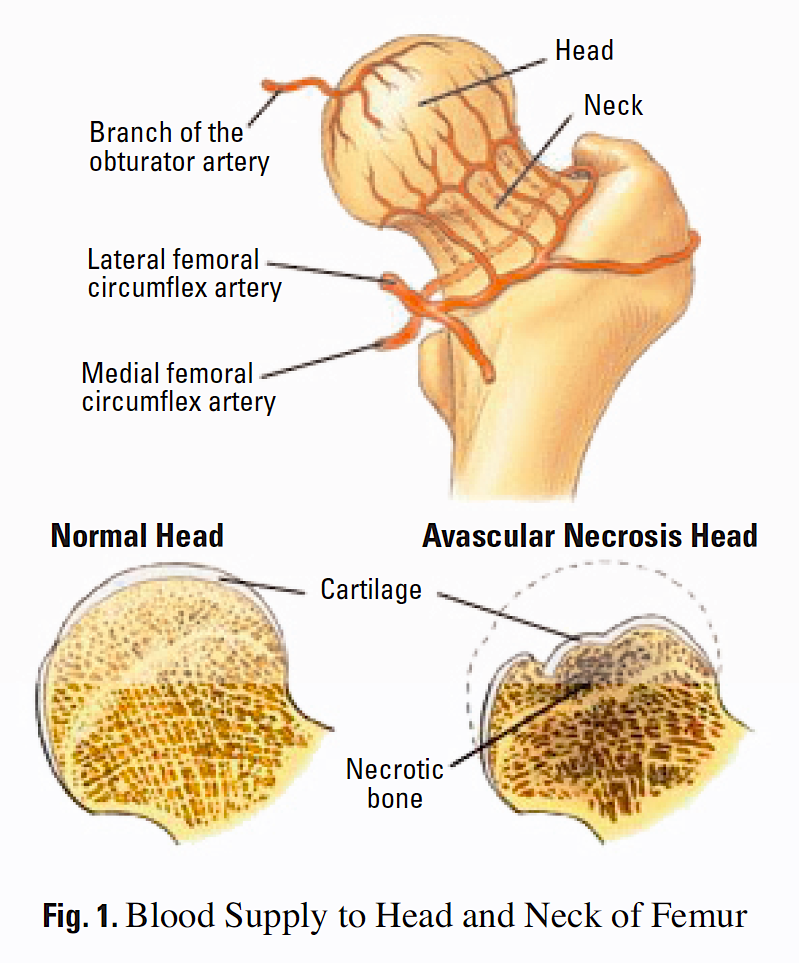
Femoral Neck Blood Supply (nutritionreview.org)
Prognosis
- One year mortality 20-30% (Brauer 2009)
- Increased mortality risk has been associated with
- Male sex
- Age >85
- Higher ASA classification
- Delay to surgery and early mobilization
- Complications
- Infection, Thromboembolism, Nonunion
- Avascular necrosis (AVN)
- Due to location of blood supply, femoral neck fractures have higher incidence of AVN than intertrochanteric fractures
- 5-15% of nondisplaced fractures develop AVN (Egol)
- Incidence of AVN increases with degree of displacement
Take Home Points:
- Investigate the cause of trauma in all patients presenting with femoral neck fractures (mechanical vs syncope)
- Assess for concomitant injuries, especially in the elderly patient
- Occult fractures are common – proceed to advanced imaging if index of suspicion high
- Provide adequate pain control and consider regional nerve block
Read More
The Ultrasound Podcast: Episode 24 – Femoral Nerve
Steele M, Stubbs AM. Hip and Femur Injuries. In: Tintinalli JE, Stapczynski J, Ma O,
Yealy DM, Meckler GD, Cline DM. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e New York, NY: McGraw-Hill; 2016.
Smith WR et al. Chapter 2. Musculoskeletal Trauma Surgery. In: Skinner HB, McMahon PJ. eds. Current Diagnosis & Treatment in Orthopedics, 5e New York, NY: McGraw-Hill; 2014.
References
Brauer CA et al. Incidence and Mortality of Hip Fractures in the United States. JAMA 2009; 302(14): 1573-9. PMID: 19826027
Egol, KA et al. Chapter 29. Femoral Neck Fractures. Handbook of Fractures. 2015. Link
Hakkarinen, DK. Magnetic Resonance Imaging Identifies Occult Hip Fractures Missed by 64-slice Computed Tomography. J Emerg Med. 2012; 43(2) 303-7. PMID: 22459594
Schnell S et al. The 1-Year Mortality of Patients Treated in a Hip Fracture Program for Elders. Geriatr Orthop Surg Rehabil 2010: 1(1): 6-14. PMID: 23569656
Skinner, Harry B., and Patrick J. McMahon. Current Diagnosis & Treatment in Orthopedics. McGraw-Hill Education, 2014.
Thomas RW et al. The Validity of Investigating Occult Hip Fractures Using Multidetector CT. Br J Rad 89.1060 (2016). PMID: 26838948

Is surgery always required to treat a femoral neck fracture?