Definition: Ebola virus disease (EVD), also known as Ebola hemorrhagic fever, is due to a virulent pathogen spread by human-human transmission. The disease has the potential of causing multi-organ failure with high mortality rates in the absence of a standard treatment or vaccination.
Epidemiology:
- Endemic to parts of Western Africa
- Current outbreak (December 2013 to present): 26,933 total cases and 11,120 deaths (Ebola 2015)
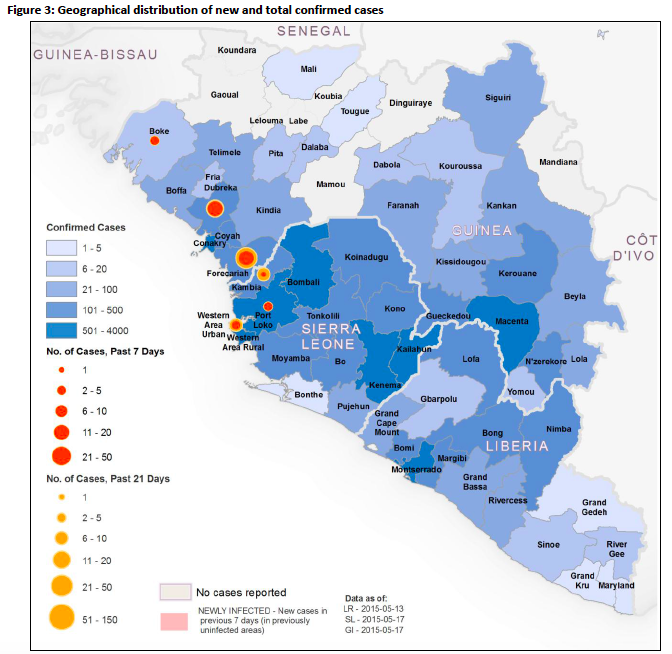
- Predominant transmission occurring in West Africa (Sierra Leone, Guinea, Liberia)
- Incubation period: 3-21 days
Pathophysiology:
- Current strain 97% homology with Zaire ebolavirus, which is the most virulent strain with prior fatality rates as high as 90% (Tattevin 2014)
- Ebola virus causes a systemic inflammatory response that impairs the vascular, coagulation, and immune systems (Feldman 2011)
- Transmission requires direct contact through broken skin or mucous membranes with body fluids of symptomatic infected or convalescent patients
- Symptoms (incubation period) occur within 21 days of direct contact
- Mean incubation time from prior outbreaks ranged from 3-13 days (Tattevin 2014)
- If a patient presents with symptoms greater than 21 days post-contact, can likely be ruled out.
- Fatalities due to combination of hypovolemic (vomiting/diarrhea) and septic shock, massive bleeding (typically GI), and end-organ failure
- Usually occurs between days 6-16 (Tattevin 2014)
Symptoms:
- Fever
- Nausea/vomiting/diarrhea
- Flu-like symptoms (i.e. headache, myalgias/arthalgias)
- Anorexia
Physical Exam Findings: poly-organ involvement and life-threatening signs manifests later as disease progresses
- HEENT: conjunctival injection, oropharyngeal erythema
- CV: hypotension
- Resp: tachypnea, rales (pulmonary edema late finding)
- Abdomen: hyperactive bowel sounds
- GU: anuria/oliguria
- Skin: diffuse non-pruritic maculopapular rash, desquamation, petechiae/ecchymosis, mucosal membrane hemorrhage
- Neuro: altered mental status, lethargy
ED Management/Treatment:
- Identification/Isolation
- Who to Isolate: patients with concerning symptoms + fever AND who have traveled to/reside in high-risk countries OR have had direct contact with an Ebola positive or suspected patient.
- Immediate identification precludes all management given the high susceptibility of transmission to other patients and health care providers.
- Patients should remain in isolation until alternative diagnosis can be proven.
- Medical staff should be trained in donning/doffing personal protective equipment, and receive frequent recertification to practice of applying PPE.
- Supportive Care
- Supportive care central as there is no specific treatment for Ebola
- Fluid substitution and electrolyte repletion will likely be the most immediate problem to be addressed.
Diagnostic Testing:
- Physical Exam Diagnosis
- Given the delay in serologic testing and potential of false negative results (depending on time course of illness), diagnosis should be based on clinical assessment.
- Differential diagnosis should also include malaria, typhoid fever, Chikugunya, yellow fever, fulminant viral hepatitis, influenza and sepsis.
- Serologic Diagnosis
- Definitive diagnosis of EVD based upon detection of viral antigen via ELISA or viral RNA by RT-PCR.
- Viral antigen and nucleic acid can be detected as early as day 3 of symptoms, but can take up to 10 days (Meyers 2015).
- Antibody testing can also be tested using ELISA, but is less frequently used.
- Specimens should be collected and sent to international/national reference centers.
- Other common laboratory findings may include: leukopenia, thrombocytopenia, elevated BUN/Cr, elevated AST/ALT, prolonged PT/PTT
Convalescent Period
- In Ebola positive patients, virus will clear from blood and urine first, however viral antigens may still be present in semen as long as 3 months into convalescent period.
- Newly reported in NEJM May 2015, found a recovering Ebola patient who developed ocular symptoms (blurring of vision, foreign body sensation, and photophobia) 10 weeks after clearance of viremia in blood (Varkey 2015)
- +EVD within aqueous humor, but negative in tears/conjunctiva
- Sight threatening panuveitis improved with prednisolone, atropine and timolol drops, in addition to oral prednisone.
- Limited data of other convalescent symptoms.
Take Home Points:
- Identify and isolate patients with concerning symptoms who have either traveled to or reside in high-risk/endemic areas (Guinea/Sierra Leone/Liberia) AND/OR have had direct contact with persons with known or suspected Ebola within a three-week timeframe.
- Diagnosis based on clinical assessment as serologic testing may provide a false negative result or a delay in diagnosis.
- No standard of treatment, however important to provide supportive care (airway management, fluid/electrolyte resuscitation) with appropriate personal protective equipment.
References:
Ebola Situation Report — 20 May 2015. Geneva: World Health Organization, 2015. (http://apps.who.int/ebola/en/current-situation/ebola-situation-report-20-may-2015)
Feldman H, Geisbert TW. Ebola haemorrhagic fever, Lancet 2011;377:849-62. PMID: 21084112
Meyers L, Frawley T, Goss S, Kang C. Ebola virus outbreak 2014: Clinical review for emergency physicians. Ann Emerg Med 2015;65:101-8. PMID: 25455908
Tattevin P, Durante-Magoni E, Massaquoi M. Does this patient have Ebola virus disease? Intensive Care Med 2014;40:1738-41. PMID: 25183574
Varkey JB, Shantha JG, Crozier I, Yeh S. Persistence of Ebola virus in ocular fluid during convalescence. NEJM 2015. PMID: 25950269