Definition: Fracture at the metaphysis or the articulation of the distal radius
Mechanism: Most common mechanism is a fall on an outstretched wrist that is dorsiflexed
Epidemiology
- One of the most common fractures seen in the ED. >650,000 annually
- Represent 1/6th of all fractures treated in Emergency Departments
- Increased incidence with age; women at higher risk then men
Physical Exam
- Variable gross wrist deformity with displacement of the hand in dorsal or volar relation to the wrist, dependent on the fracture pattern.
- Neurovascular assessment of the hand
- Critical to perform complete neurologic exam
- Median nerve injury common
- Thenar paralysis (Ape hand deformity): Inability to oppose or abduct thumb
- Sensory loss of palmar aspect of first, second, third, and radial half of fourth fingers
- Carpal tunnel compression syndromes are common (13-23%).
- A full examination of the ipsilateral elbow and shoulder is required to assess for injuries caused by translated force
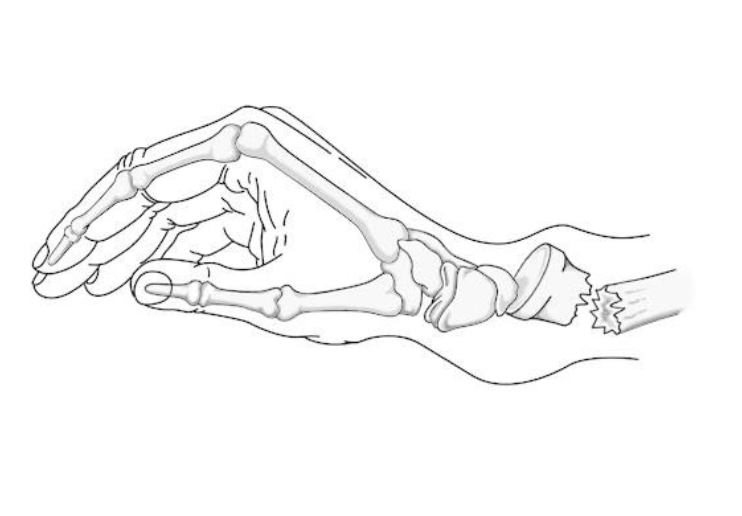
Colles’ Fracture (studyblue.com)
Fracture Classification
- Descriptive Classifications
- Open vs Closed
- Displacement
- Angulation
- Comminution
- Loss of length
- Eponyms
- Colles’ (or “dinner fork” deformity):
- 90% of distal Radius fractures
- Extra-articular, dorsally angulated distal radius
- Caused by fall onto hyperextended, radially deviated wrist
- Eponym traditionally only included non-articular fractures. Currently accepted to describe intra-articular fractures
-
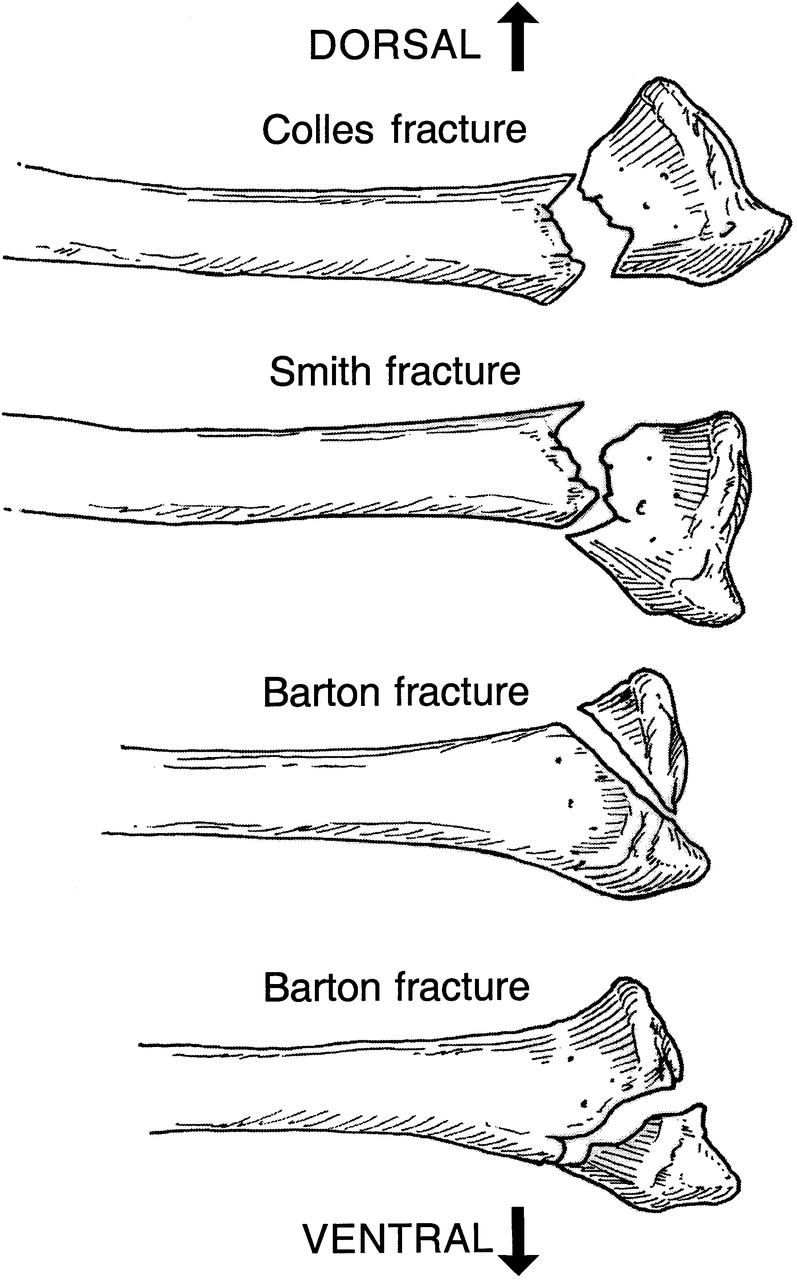
Common Distal Radius Fractures (fprmed.com)
Smith (“reverse Colles’” or “garden spade” deformity):
- Distal volar displacement or angulation of fracture
- Often caused by fall onto dorsiflexed, supinated wrist
- Typically unstable and require open reduction and internal fixation (ORIF)
- Barton
- Intraarticular dorsal or volar (more frequent) rim fracture
- Extreme dorsiflexion of pronated wrist
- Usually unstable and not easily reducible. Requires ORIF
- Chauffer/Hutchinson:
- Radial styloid avulsion fracture
- Dorsiflexion and ulnar deviation causing compression of scaphoid against styloid
- Associated w/ intercarpal ligamentous injury
- Sugar tong splint with urgent orthopedic evaluation for likely ORIF
- Die Cast
- Depressed fracture of articular surface at the lunate fossa
- Easy to miss because the carpal arc is not disrupted
- Requires urgent orthopedic follow up for likely ORIF
- Colles’ (or “dinner fork” deformity):
X-Ray Fracture Patterns

Colles' Fracture (Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 12382)

Chauffer Fracture (Case courtesy of Dr Alexandra Stanislavsky, Radiopaedia.org. From the case rID: 12360)
X-ray Findings
- Necessary views: AP, Lateral and Oblique
- Review films for concomitant injuries, particularly carpal bone injuries which can easily be overlooked
- Key Measurements:
| Normal Range | Acceptable in Healed Wrist | |
| a) Radial Inclination/Tilt:
Measured on PA view by drawing a line perpendicular to the long axis of the radius and a tangential line from the radial styloid to the ulnar corner of the lunate fossa. |
13-30 degrees. | < 5 degree loss |
| b) Radial Length/Shortening:
Measured on PA view by measuring the distance from the tip of the radial styloid to the distal articular surface of the ulna. |
8-18 mm | < 5 mm Radial shortening |
| c) Volar Tilt:
Measured on Lateral view by drawing a line perpindicular to the long axis of the radius and a tangential line along the slope of the dorsal to volar surface of the radius |
0-28 degrees, avg of 11 degrees | Dorsal angulation of <5mm or within 20 degrees of contralateral wrist |

Hematoma Block (EM News)
ED Management
- Closed Reduction
- All closed fractures should undergo closed reduction even if operative management is expected
- Reduces swelling
- Relieves nerve compression
- Provides pain relief
- Always target optimal fracture reduction
- Closed reduction may be definitive management for non-displaced or minimally displaced fractures (ie. those fractures with acceptable healing parameters or those that can be reduced to those parameters)
- Closed reduction in high risk surgical patients may be definitive, even outside “acceptable” parameters
- All closed fractures should undergo closed reduction even if operative management is expected
- Reduction technique
- Supply adequate analgesia
- Hematoma block
- Systemic analgesia
- Procedural sedation if necessary
- Place Patient in traction with finger traps and hanging weights
- Hyperextension Traction Reduction
- For further guidance on reduction technique refer to the following videos:
- Supply adequate analgesia
- Place patient in a Sugar Tong Splint w/ wrist in Neutral Position and MCP joints free
- Repeat neurovascular exam after reduction and splinting
- Close Orthopedic follow up for repeat imaging and decision for operative management
Prognosis
- Colles’ fractures can be managed non-operatively if reduction is within acceptable anatomic limits
- Loss of reduction and need for eventual surgical management is associated with:
- Higher degrees of initial displacement
- Elderly patients
- Metaphyseal comminution
- Potential complications of Colles’ fractures:
- Median nerve neuropathy, sometimes requiring carpal tunnel release
- Osteoarthritis at radiocarpal and radioulnar articulations
- Finger/Wrist/Elbow stiffness – minimize likelihood with aggressive occupational therapy
- Extensor pollicis longus tendon rupture as late complication, more frequently post ORIF.
- All distal radius fractures have potential complications that include neuropathies, tendon injuries, and osteoarthritis
Take Home Points
- Every distal radius requires closed reduction and placement of a sugar-tong splint
- Document a thorough neurovascular exam prior to and after reduction with particular attention to the median nerve
- Emphasize early orthopedic surgery follow up for further management
- Don’t miss concomitant hand, wrist, forearm and elbow injuries such as lunate dislocation, carpal fractures, or radial head dislocation.
Read More
Radiopaedia: Distal Radial Fracture
Radiopaedia: Chauffer Fracture
Orthofilms: Closed Reduction of a Distal Radius Fracture
DeAngelis MA, Wald DA. Wrist. In: Sherman SC. eds. Simon’s Emergency Orthopedics, 7e. New York, NY: McGraw-Hill; 2014. Link
Egol K et al. Handbook of Fractures. Philadelphia: Wolters Kluwer; 2015: 266-278
Petron, DJ. Distal Radius Fractures in Adults. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (Accessed on June 8th, 2016)


I love Mellick’s fantastic videos and they did an amazing reduction but I always found their hyperflexion approach to reduction interesting as I’d never been taught/read that this was good for the median nerve which can be frequently involved……
Love CoreEM, thanks for all your generous education
Great article, thanks!
Quick question though – why a haematoma block rather than a Biers? I can see the clear advantages of a haematoma block when looking at ED resources (Biers requires the patient needs to be in a monitored bed, nurse-intensive), however I feel that you can get better reduction results with a Biers as you can apply great traction and remoulding/reduction with minimal discomfort to the patient.
I’d love to hear your thoughts!
Sinead – I think a Biers block would be fine if you have that skill. Many Emergency Physicians (at least in the US) are not trained to do Biers blocks