Background
- Digoxin is the most common formulation of digitalis, a cardiac glycoside used in the management of systolic heart failure and atrial arrhythmias.
- The use of medicinal plants containing cardiac glycosides dates back to the ancient Egyptians. Modern digitalis is derived from the foxglove plant and has been used for the last 200 years
- Although the use of digoxin has declined over the past 2 decades, digoxin toxicity exposure rates have risen, possibly because of increased use in the elderly.
- There are an estimated ~3,500 emergency hospitalizations for digoxin toxicity in the US each year.
- Digoxin toxicity can present acutely or chronically.
- Acute presentations can occur with accidental or intentional ingestions.
- Chronic presentations are seen with renal failure, supratherapeutic dosing, or drug-drug interactions, especially inhibitors of p-glycoprotein(e.g. amiodarone, erythromycin, sertraline).
Pharmacology
- Digoxin undergoes hepatic metabolism independent of CYP-450 system and is renally excreted.
- Half-life is 1.5-2 days in healthy adults, but can be 4-6 days in patients in renal failure.
- Digoxin has a narrow therapeutic window, typically 0.5-1.0 ng/mL, with toxicity range beginning at concentrations greater than 2.0 ng/mL.
- Serum digoxin concentrations do not necessarily correlate with toxicity, or degree of toxicity. There are many reports of asymptomatic patients with elevated digoxin concentrations, as well as clinical toxicity with concentrations in the therapeutic range.
Mechanism of Action and Pathophysiology
- Digoxin reversibly inhibits Na+-K+ ATPase pump in the myocardium, inhibiting Na+-Ca2+ exchange and increasing intracellular calcium concentration.
- Increased intracellular Ca2+ concentration increases cardiac contractility.
- In toxic doses, intracellular calcium elevates further and triggers afterdepolarizations. This increases the risk of arrhythmias while shortening the refractory period and increasing automaticity.
- Digoxin also has neurohormonal effects, which increases parasympathetic tone. Increased vagal tone leads to stronger atrioventricular nodal blockade, leading to more uncontrolled arrhythmia.
- Extra-cardiac Manifestations
- The manifestations of digoxin toxicity are divided into cardiac and extra-cardiac effects.
- The most common extra-cardiac symptoms of digoxin toxicity are anorexia, nausea, fatigue and visual disturbance.
- The classically described visual disturbances are enhanced perception of yellow and green and seeing halos of light, but these manifestations are actually less common than blurred vision.
- Other neuropsychiatric effects are possible, including headache, confusion, hallucinations and delirium.
- The key laboratory abnormality in acute digoxin toxicity is hyperkalemia, which results from inhibition of the Na+-K+
- In acute toxicity, hyperkalemia strongly correlates with mortality. In a 1973 landmark study performed before the development of digoxin-specific antibody fragments, there was 0% mortality with K+ <5 mEq/L and 100% mortality with K+ >5.5 mEq/L.
- In chronic toxicity, hypokalemia can exacerbate toxic effects of digoxin on the myocyte and increase risks of arrhythmias.
- Cardiac Manifestations
- The cardiac manifestations of digoxin toxicity are an immediately life-threatening complication. They result from increased automaticity, shortened refractory period and AV nodal blockade.
- Digoxin can cause mild PR prolongation and a characteristic scooping of the ST segment. These changes do not necessarily indicate toxicity and can be seen with therapeutic levels of digoxin.
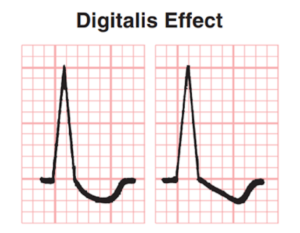
The scooped ST segments characteristic of digoxin
- Digoxin can precipitate all degrees of AV heart block and almost any arrhythmia (except for a rapidly conducted supraventricular tachycardia).
- The most characteristic arrhythmias associated with digoxin toxicity are bidirectional ventricular tachycardia with alternating wide QRS complexes and atrial tachycardia with AV block. Still, these arrhythmias are not specific for digoxin toxicity.
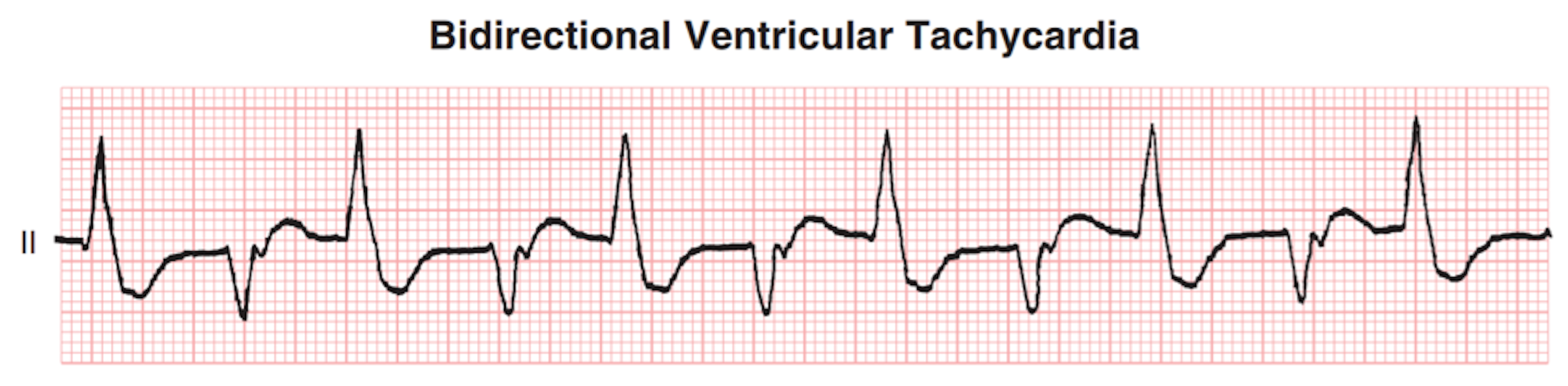
(Goldberger 2018)
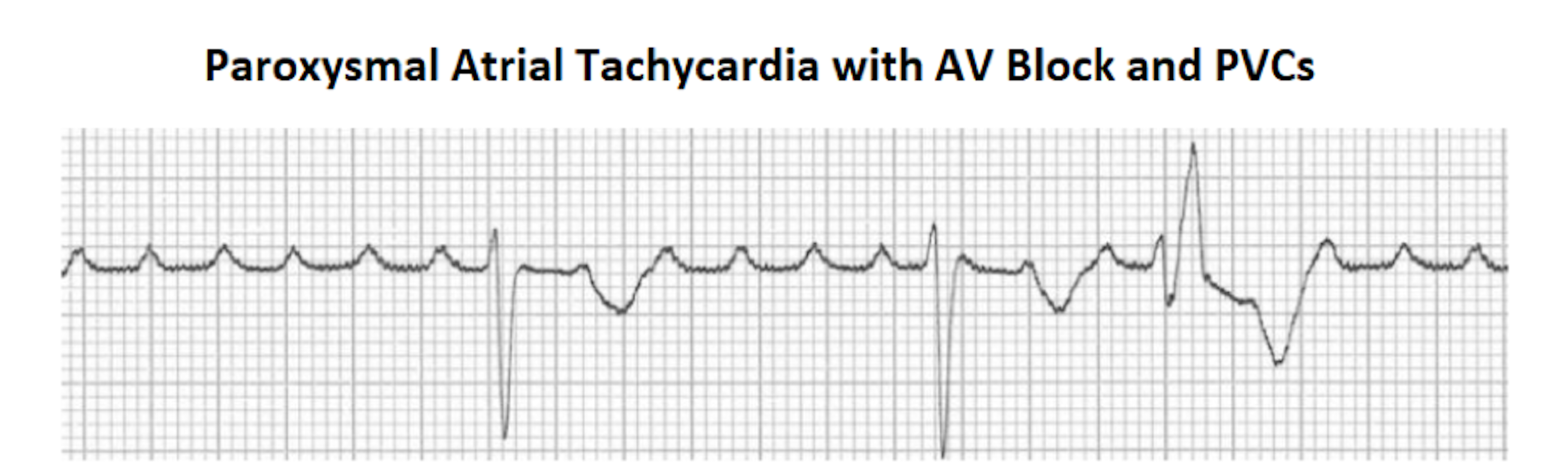
(Burns 2019)
- Other common cardiac manifestations of digoxin toxicity include new-onset AV block, frequent PVCs, sinus bradycardia, and junctional rhythms.
- In atrial fibrillation, digoxin toxicity can cause significant slowing of the ventricular rate with increased PVCs.
Treatment
- The key treatment for life-threatening digoxin toxicity is the use of digoxin-specific antibody fragments (Fab), which bind digoxin and rapidly reverse toxicity.
- Treatment with antidigoxin-Fab has been shown to be effective in 80-90% of cases, with improvement within 1 hour and complete reversal of symptoms. usually within 4 hours.
- The early use of digoxin-specific Fab in patients with life-threatening digoxin poisoning decreases mortality.
- Antidigoxin-Fab is indicated in any patient with severe cardiac manifestations of toxicity, including ventricular arrhythmias, high-degree AV block, and hyperkalemia.
- Antidigoxin-Fab may also be used in patients with significantly elevated serum digoxin levels >10 ng/mL in acute ingestion.
- Use of antidigoxin-Fab may also be cost-effective in patients with evidence of chronic digoxin toxicity and levels as low as 3 ng/mL, especially in patients with renal dysfunction.
- Dosing of digoxin-specific Fab can be calculated based on the amount ingested or the serum digoxin level.
- Empiric therapy should be used in life-threatening cases instead of waiting for a serum level.
- Empiric therapy for acute poisoning: 10-20 vials
- Empiric therapy for chronic poisoning: 3-6 vials
- One potential side effect of antidigoxin-Fab is hypokalemia, as it will rapidly restore Na+-K+ ATPase activity.
- Potassium should be repleted in hypokalemia
- GI decontamination with charcoal may be helpful in acute ingestions, as charcoal not only helps with GI elimination but may also increase systemic clearance by acting as a “dialysis membrane”.
- For high-degree symptomatic AV block, IV atropine or temporary pacing may be judiciously used. A 2004 retrospective study showed that in accidental digoxin overdose, transvenous temporary pacing was safe for patients with symptomatic bradycardia.
- For ventricular arrhythmias, IV lidocaine may be helpful.
- Electrical cardioversion patients with digoxin toxicity may precipitate VT or VF and is contraindicated.
- In patients with symptoms of digoxin toxicity but no signs concerning for severe poisoning, patients can be observed with cardiac monitoring until symptoms resolve and digoxin concentrations are therapeutic.
Take Home Points
- Digoxin toxicity can be a life-threatening condition.
- Serum levels do not always correlate with the degree of clinical toxicity – i.e. therapeutic levels may be toxic OR supratherapeutic levels may be benign.
- Digoxin toxicity causes a wide variety of dysrhythmias, including ventricular tachycardias and high-degree AV blocks.
- Prompt treatment of any severe digoxin poisoning with digoxin-specific antibody fragments (Fab) is essential.
- Hyperkalemia is a poor prognostic indicator and should be a concerning sign in digoxin toxicity.
References
Antman EM, Wenger TL, Butler Jr VP, et al. Treatment of 150 cases of life- threatening digitalis intoxication with digoxin-specific Fab antibody fragments: final report of a multicenter study. Circulation 1990; 81: 1744-52. PMID: 2188752
Bauman JL, Didomenico RJ, Galanter WL. Mechanisms, manifestations, and management of digoxin toxicity in the modern era. Am J Cardiovasc Drugs. 2006;6(2):77-86. PMID: 16555861
Bayer MJ. Recognition and management of digitalis intoxication: implications for emergency medicine. Am J Emerg Med. 1991;9(2):29-34. PMID: 1997019
Bismuth C, et al. Hyperkalemia in acute digitalis poisoning: prognostic significance and therapeutic implications. Clin Toxicol. 1973;6(2):153-162. PMID: 4715199
Budnitz D, et al. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365(21):2002-2012. PMID: 22111719
Burns E. Digoxin Toxicty. Life in the Fastlane Medical Blog. 2019. < https://litfl.com/digoxin-toxicity-ecg-library/>.
Chen J, et al. Safety of Transvenous Temporary Cardiac Pacing in Patients with Accidental Digoxin Overdose and Symptomatic Bradycardia. Cardiology. 2004; 102(3):152-5. PMID: 15334025
Ehle M, Patel C, Giugliano R. Digoxin: clinical highlights: a review of digoxin and its use in contemporary medicine. Crit Pathw Cardiol. 2011;10(2):93-98. PMID: 21988950
Gheorghiade M, Adams KF Jr, Colucci WS. Digoxin in the management of cardiovascular disorders. Circulation. 2004;109(24):2959–2964. PMID: 15210613
Goldberger AL, Goldberger ZD, Shvilkin A. Goldberger’s Clinical Electrocardiography. Elsevier 2018. 211-216.
Hussain Z, Swindle J, Hauptman PJ. Digoxin use and digoxin toxicity in the post-DIG trial era. J Card Fail. 2006;12(5):343-346. PMID: 16762795
Lapostelle F, et al. Digoxin-specific Fab fragments as single first-line therapy in digitalis poisoning. Crit Care Med. 2008;36(11):3014-3018. PMID: 18824911
Sonnenblick M, et al. Correlation between manifestations of digoxin toxicity and serum digoxin, calcium, potassium, and magnesium concentrations and arterial pH. Br Med J (Clin Res Ed). 1983;286(6371):1089-1091. PMID: 6404339
Smith TW, et al. Digitalis glycosides: mechanisms and manifestations of toxicity. Prog Cardiovasc Dis. 1984;26(5):413-458. PMID: 6371896