Definition: Venous thromboembolism (VTE) of the deep venous system predominantly seen in the lower extremity.
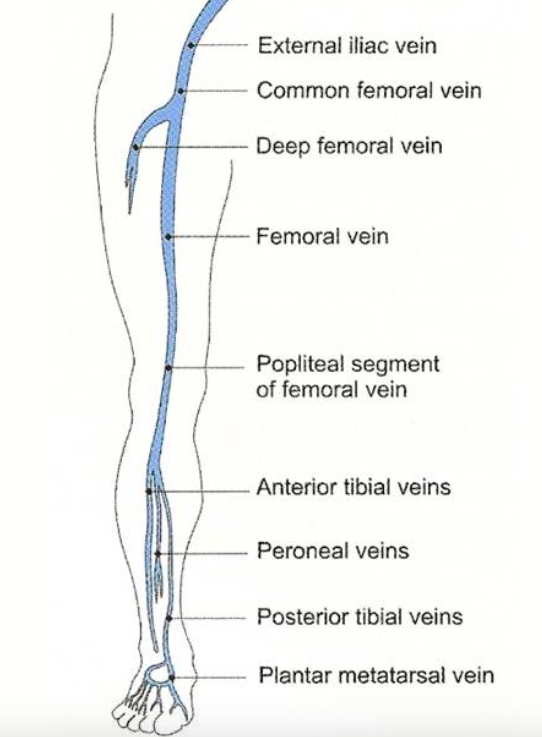
Lower Extremity Venous System (http://venacure-evlt.com/)
Pathophysiology
- Excess fibrin production and deposition within deep veins
- Virchow’s Triad describes the inciting mechanisms for VTE
- Venous injury
- Venous stasis (slow blood flow)
- Hypercoagulability (including exogenous hormone use)
Anatomy
- Lower extremity venous anatomy
- The lower extremity contains deep and superficial venous systems
- Superficial veins: Greater and short saphenous veins
- Deep veins: Anterior/Posterior Tibial veins, peroneal veins, popliteal vein, superficial femoral vein, deep femoral vein, common femoral vein
- Proximal DVT: clot forming in the popliteal vein or higher within the venous system
- Distal DVT: isolated clot in the calf veins (anterior/posterior tibial and peroneal veins)
- Upper Extremity DVT: Thrombosis within the axillary vein
- DVTs occur more frequently in the left leg secondary to the crossing of the left iliac artery over the left iliac vein increasing the chance of external compression

Unilateral Leg Swelling
Presentation
- Symptoms
- Early symptoms are nonspecific and include cramping or calf fullness
- Classic symptoms: unilateral leg swelling, edema, redness and pain
- Upper extremity: arm swelling, finger swelling (may be evidenced by ill-fitting rings)
- Physical Exam
- Unilateral leg swelling
- Erythema and warmth
- Tenderness to palpation along the deep venous system
- Palpable venous “cord”
- Dilation of superficial veins
- Homan’s sign: pain in the calf with dorsiflexion at the ankle is neither sensitive nor specific
Differential Diagnosis
- Cellulitis
- Peripheral vascular disease
- Trauma or Musculoskeletal Injury
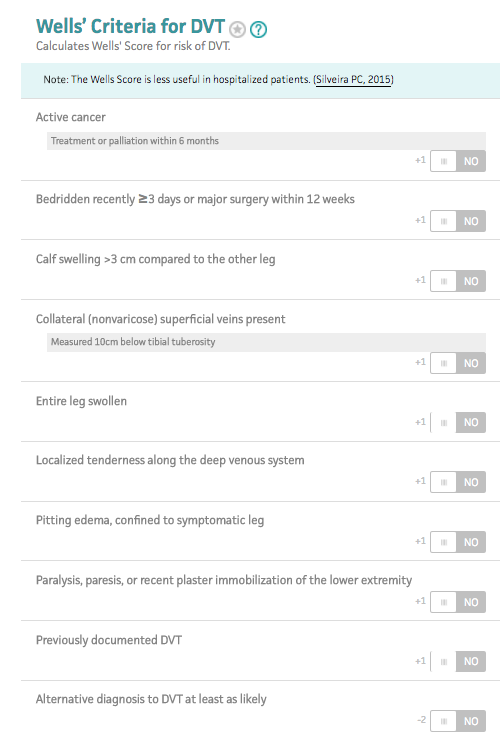
Wells’ Criteria (MDCalc.com)
Diagnostics
- Start with pretest probability
- May be done with unstructured clinical gestalt in experienced providers
- Wells’ Criteria Decision Instrument (INSERT MDCalc IMAGE) (Wells 2003)
- Score = 0
- DVT unlikely < 5%
- Perform high or moderate-sensitivity D-dimer testing (see below)
- Score = 1-2
- DVT moderate risk ~ 17%
- Perform high-sensitivity d-dimer or proceed directly to US if high-sensitivity D-dimer not available
- Score > 3
- DVT high risk 17-53%
- Obtain D-dimer and US imaging for diagnosis + risk stratification
- Score = 0
- Laboratory Evaluation
- Renal function: guides choice of anticoagulation strategy
- D-dimer
- Protein generated by the breakdown of cross-linked fibrin. An elevated plasma level indicates the presence of clot formation
- Conditions that elevate D-dimer (even in the absence of VTE)
- Active malignancy
- Infection
- Inflammation
- Advanced age
- Recent surgery
- Prolonged immobilization or bed rest
- Myocardial infarction
- New indwelling catheter
- Stroke
- Quantitative D-dimer Testing
- Common methods are via ELISA and Immunoturbidimetric technique
- Cutoffs for “negative” test vary based on assay used (typically < 500 ng/ml). Check you local institution parameters
- Test performance characteristics depend on sensitivity of assay being used
- High Sensitivity D-dimer Assay Test Characteristics (Wells 2006)
- A negative test is adequate to rule out DVT in low or moderate probability patients
- A negative test may still require additional testing in high probability patients
| Pretest Probability | Sensitivity | Specificity | (+) LR | (-) LR |
| Low | 95% (82-99) | 58% (45-71) | 2.4 | 0.10 |
| Moderate | 98% (91-100) | 41% (31-52) | 1.7 | 0.05 |
| High | 97% (94-99) | 36% (29-43) | 1.5 | 0.07 |
- Moderate Sensitivity D-dimer Assay Test Characteristics
- A negative test is adequate to rule out DVT in low probability patients
- A negative test may still require additional testing in moderate or high probability patients
| Pretest Probability | Sensitivity | Specificity | (+) LR | (-) LR |
| Low | 86% (79-92) | 78% (71-83) | 4.0 | 0.20 |
| Moderate | 85% (73-93) | 66% (58-73) | 2.4 | 0.23 |
| High | 90% (80-95) | 49% (40-58) | 1.7 | 0.20 |
- Age-Adjusted D-dimer
- Normal D-dimer levels become elevated with advancing age
- Multiple studies look at using a relative D-dimer cutoff based on age instead of a uniform cutoff
- Age-adjusted Cutoff
- 10 X age (apply to age > 50)
- D-dimer cutoff for 75 year old = 750
- D-dimer cutoff for 35 year old = 500
- Age-adjusted D-dimer increases specificity in older patients with minimal loss of sensitivity (Adams 2014)
- Reasonable to apply in low to moderate risk patients as a rule out test
- In all studies, D-dimer assay standard cutoffs were 500 ng/ml
- Qualitative D-dimer Testing
- Lower sensitivity than quantitative testing (78-93%)
- Adequate to rule out DVT in low risk patients only
-
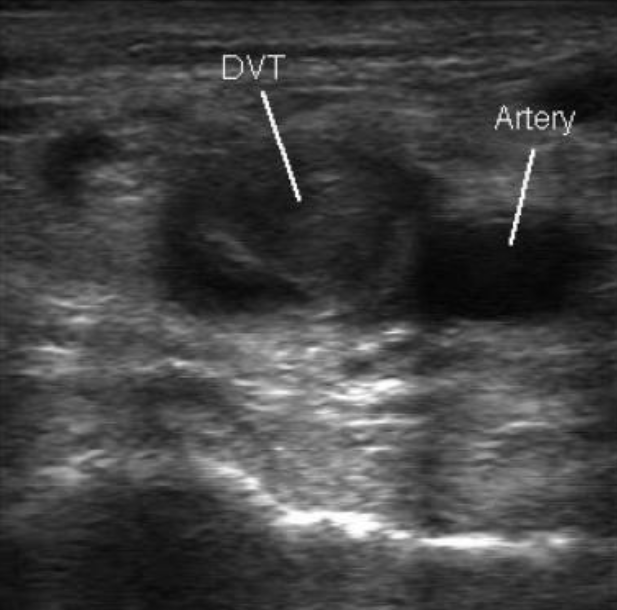
DVT on US (Medscape)
Radiographic Evaluation
- Venous duplex ultrasound (US)
- Diagnostic modality of choice as it is non-invasive and can be performed rapidly
- Multiple US techniques may be employed including 3-point (common and superficial femoral veins and popliteal veins) and whole leg
- Technique: Graded compression along the path of the vein in question. If the vein compresses, there is no DVT present
- Test Performance Characteristics
- Sensitivity ~ 95%
- Specificity ~ 95%
- Characteristics of test when performed by certified US technician and interpreted by board-certified radiologist
- Low pretest probability
- A negative 3-point US effectively rules out DVT
- A negative whole leg US effectively rules out DVT
- Moderate to High pretest probability
- A single, negative 3-point US is inadequate to rule out DVT
- Can add a D-dimer and if negative, rules out DVT
- Can repeat the 3-point US at 2-7 days
- A single, negative whole leg US is adequate to rule out DVT
- A single, negative 3-point US is inadequate to rule out DVT
- “Free-Floating” DVT
- Thrombi where proximal end is not attached to the wall of the vein at time of diagnosis
- Limited evidence does not suggest a higher rate of embolization (Baldridge 1990, Pacouret 1997)
- Emergency Physician POCUS
- Data on the performance of POCUS for DVT are based on 2-point and 3-point US (not whole leg)
- Studies of POCUS show varying test characteristics
- Crisp 2010
- Sensitivity 100% (CI 92-100%)
- Specificity 99% (CI 96-100%)
- Kim 2016
- Sensitivity 86% (CI 73-94%)
- Specificity 93% (CI 89-96%)
- Crisp 2010
- Based on current literature, Emergency Physician performed POCUS cannot be used to rule-out DVT
- CT Venogram (CTV)
- May be added on to a CT pulmonary angiography (CTPA) being performed for PE
- Identifies DVT in the absence of PE on CTPA in up to 2% of patients
- Interobserver agreement on CTV is less than that seen with CTPA (likely due to suboptimal image acquisition)
- CTV should not be routinely added to CTPA
- MRI
- Limited utility due to availability, cost and lack of data demonstrating superior performance to US
- Useful for evaluation of pelvic veins and vena cava
- Venous duplex ultrasound (US)
Isolated Distal DVT (i.e. Calf Clots)
- The significance of isolated distal DVTs is unknown. Many of the US examinations currently done (i.e. 3 point US) do not look for isolated distal DVTs
- It is unclear whether systemic anticoagulation is beneficial to the patient with these clots
- The danger with an isolated distal DVT is that it will propagate and become a proximal DVT with the associated risks
- Risk factors for extension (Kearon 2016)
- D-dimer is positive (particularly with larger elevations)
- Extensive thrombosis (> 5 cm in length, multiple veins, > 7 mm diameter)
- Proximity to proximal veins
- No reversible provoking factor for the DVT
- Active cancer
- History of VTE
- Admitted to the hospital
Management (Kearon 2016)
- Proximal DVT without history of cancer
- Oral anticoagulant alone (dabigatran, rivaroxaban, apixaban or edoxaban (NOAC)) preferred over a vitamin K antagonist (VKA) (Grade 2B recommendation)
- VKA preferred to low-molecular weight heparin (LMWH) (Grade 2C recommendation)
- Duration of treatment: 3 months for 1st clot (Grade 1B recommendation)
- Proximal DVT with cancer (“cancer-associated thrombosis)
- LMWH preferred to VKA therapy, dabigatran, rivaroxaban, apixaban or edoxaban (Grade 2C recommendation)
- Duration of treatment: 3 months for 1st clot (Grade 1B recommendation)
- Distal DVT (isolated)
- Up to 25% will propagate proximally in admitted patients but no robust evidenced in ambulatory patients discharged home
- Absence of severe symptoms and no risk factors for extension
- Serial imaging over 2 weeks preferred to anticoagulation (Grade 2C recommendation)
- No established role for providing antiplatelet therapy (i.e. aspirin) alone in these cases but a reasonable intervention (Kline 2014)
- Presence of severe symptoms or risk factors for extension
- Anticoagulation preferred to serial imaging (Grade 2C recommendation)
- Anticoagulation choices same as for proximal DVT (Grade 1B recommendation)
- Superficial Thrombophlebitis
- Saphenous vein clots above the knee can spread into deep venous system via the saphenous-femoral junction (Decousus 2010)
- Initial treatment with NSAIDs, warm compresses and compression stockings
- Repeat US in 2-5 days and start anticoagulation if clot extending
- Catheter-Directed Thrombolysis (CDT)
- Does not show substantial benefits in most patients with proximal DVT and likely increases risk of major bleeding (Bashir 2014)
- Patients with iliofemoral DVT and a low risk of bleeding may benefit from CDT in terms of decreased rates of post-thrombotic syndrome
Complications
- Pulmonary embolism
- Venous insufficiency
- Results from damage to venous valves
- Spectrum of manifestations ranging from varicose veins to postphlebetic syndrome
- Postphlebetic syndrome
- Chronic pain and swelling
- Ulcerations (can be non-healing)
- Increased susceptibility to infection
Disposition
- Most patients with DVTs can be discharged home on either oral anticoagulation with a NOAC or with a LMWH bridge to warfarin
- Consider admission for patients with more extensive clot
- Refer patients with moderate to high suspicion for DVT with a negative 3-point ultrasound or in patient with isolated calf clots in 3-5 days
Take Home Points
- A negative high sensitivity D-dimer effectively rules out the diagnosis of DVT in patients with low to moderate risk of DVT. In those with high-risk, an US should be considered regardless of the D-dimer results
- Consider using an age-adjusted D-dimer to rule out DVT in low to moderate risk patients with advanced age as it increases specificity with only a small effect on sensitivity
- Venous duplex ultrasound is the test of choice in patients who are high-risk and/or have a positive D-dimer. POCUS DVT study has not been consistently shown to have comparable sensitivity to radiology technician, radiologist read US
References:
Wells PS et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003; 349(13):1227-35. PMID: 14507948
Wells PS et al. Does this patient have deep vein thrombosis? JAMA. 2006; 295(2):199-207. PMID: 16403932
Adams D et al. Clinical utility of an age-adjusted D-dimer in the diagnosis of venous thromboembolism. Ann Emerg Med 2014. PMID: 24439717
Baldridge ED et al. Clinical significance of free-floating venous thrombi. J Vasc Surg 1990; 11: 62-9. PMID: 2404143
Pacouret G et al. Free-floating thrombus and embolic risk in patients with angiographically confirmed proximal deep venous thrombosis: a prospective study. Arch Intern Med 1997; 157: 305-8. PMID: 9040297
Crisp JG et al. Compression ultrasonography of the lower extremity with portable vascular ultrasonography can accurately detect deep venous thrombosis in the emergency department. Ann Emerg Med 2010; 56 (6): 601-10. PMID: 20864215
Kim DJ et al. Test characteristics of emergency physician-performed limited compression ultrasound for lower-extremity deep vein thrombosis. J Emerg Med 2016. PMID: 27637139
Kearon C et al. Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 2016; 149(2): 315-52. PMID: 26867832
Kline JA: Pulmonary Embolism and Deep Vein Thrombosis in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 88: p 1157-71. PMID: 26867832
Decousus H et al. Fondaparinux for the treatment of superficial-vein thrombosis in the legs. N Engl J Med 2010; 363:1222-1232. PMID: 20860504
Bashir R et al. Comparative outcomes of catheter-directed thrombolysis plus anticoagulation vs anticoagulation alone to treat lower-extremity proximal deep vein thrombosis. JAMA Intern Med. 2014;174(9):1494-1501. PMID: 25047081
