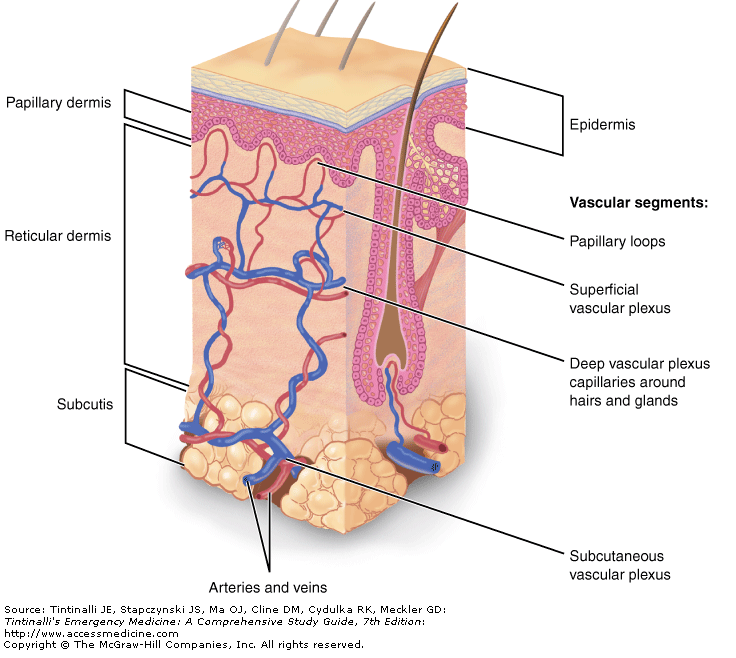
 Definition: Infection and inflammation of the deep dermis and subcutaneous tissue
Definition: Infection and inflammation of the deep dermis and subcutaneous tissue
Epidemiology:
- Overall incidence of 24.6/1000 person years, increasing incidence with age, majority receiving outpatient therapy (Simonsen 2006)
- More prevalent in males, mean age ~45 years of age (Dong 2001, Ginsberg 1981)
- Lower extremity most commonly affected site
- Most common bacteria include: B-hemolytic streptococci (Streptococcus pyogenes), Staphylococcus aureus and, less commonly, gram-negative bacilli
- Rising incidence, especially in urban settings, of community acquired methicillin resistant Staph aureus (CA-MRSA) as causative bacteria (Moran 2006)
- Immunocompromised patients are at risk for broader range of pathogens including Pseudomonas aeruginosa, clostridium species, pneumococcus, meningococcus
- Special At-risk populations (Swartz 2004):
- Patients who have undergone mastectomy with partial or full axillary lymph node dissection and breast irradiation can develop associated lymphedema leading to recurrent cellulitis of ipsilateral arm or breast
- Patient who have undergone coronary artery bypass with harvesting of saphenous vein causing lymphatic disruption and edema
- Cellulitis following exposure to saltwater, consider Vibrio vulnificus as causative organism
- In setting of animal or human bite, consider Pasteurella multocida and Capnocytophaga canimorsus
Pathophysiology:
- Develops when bacteria enter through a break in the skin barrier such as cuts, insect bites, IV drug injection site (patients may have no memory of any such inciting event)
- Bacteria then cause local inflammation by infiltration of Langerhan’s cells and keratinocytes, and release of cytokines which leads to infiltration with lymphocytes and macrophages (Kelly 2011)
Presentation

Cellulitis (Tintinalli’s Emergency Medicine)
- History
- Presence off trauma
- MRSA risk factors (see below)?
- Physical Exam
- Warmth
- Swelling
- Erythema
- Pain
- Evidence of skin breakdown
- Palpate for fluctuance suggesting an abscess
- Ultrasound
- Findings consistent with cellulitis
- Tissue edema
- “Cobblestoning”
- May be helpful in differentiating cellulitis from abscess
- Findings consistent with cellulitis

Ultrasound of Cellulitis Showing Edema + Cobblestoning
Differential
- Necrotizing fasciitis: rapidly developing infection of deep fascia, severe pain out of proportion to exam, swelling, bullae and necrosis, +/- crepitus
- Septic Arthritis: suspect when cellulitis overlies a joint
- Gout: joint pain, repeated attacks, elevated serum uric acid level
- Deep vein thrombosis: venous cord, can check Homan’s sign (discomfort behind the knee on forced dorsiflexion of foot), can be difficult to distinguish from cellulitis and may necessitate duplex to rule out thrombus
- Vasculitis: non-blanching erythema due to extravasated erythrocytes in dermis
- Stasis dermatitis: presence of telangiectasia, varicose veins, hyperpigmentation, edema subsides with recumbency
Management
- Mark extent of cellulitis: allows monitoring for progression or improvement of infection
- Infectious Disease Society of America (IDSA) empiric antibiotic recommendations in nonpurulent cellulitis (Stevens 2014)
- Use antibiotics that cover beta-hemolytic streptococci (most frequent causative organism)
- Cephalexin 500 mg PO Q6 hours X 5-7 days
- Doxycycline 100 mg PO BID X 5-7 days
- Empiric addition of trimethoprim-sulfamethoxazole (TMP-SMX) to cover MRSA in nonpurulent cellulitis has not shown benefit (Pallin 2013)
- Use antibiotics that cover beta-hemolytic streptococci (most frequent causative organism)
- Consider risk of methicillin resistant S. aureus (MRSA)
- Empiric MRSA coverage:
- Purulent cellulitis
- Recurrent cellulitis
- Lack of response to initial therapy
- Signs of systemic illness (fever, tachycardia, hypotension)
- Recent hospitalization]
- Residence in long term care facility
- Recent antibiotic therapy
- Previous episode of MRSA infection
- Medical Comorbidities: HIV, IVDU, hemodialysis, diabetes,
- Patient from community with high rate of CA-MRSA (> 30%)
- Antibiotics that will add MRSA coverage (Moran 2006)
- Check your local antibiogram for resistance patterns
- Oral Administration
- Clindamycin: 450 mg Q6 hours X -7 days
- TMP-SMX: DS 1-2 tabs BID X 5-7 days
- Doxycycline: 100 mg BID X 5-7 days
- Linezolid 600 mg TID X 5-7 days
- Intravenous
-
-
- Vancomycin: 15-20 mg/kg IV BID
- Linezolid: 600 mg IV TID
-
- Empiric MRSA coverage:

Disposition:
- Most patients are suitable for outpatient management with oral antibiotics
- Indications for admission:
- Significant systemic illness (fever, hypotension)
- Immunosuppressed state (HIV, diabetes, on chemotherapy)
- Rapidly progressing cellulitis
- Predictors of outpatient treatment failure (Peterson 2014)
- Presence of fever
- Chronic leg ulcers
- Chronic edema or lyphedema
- Prior cellulitis at the same site
- Cellulitis at wound site
Take Home Points:
- Most cellulitis patients can be treated as outpatients with oral antibiotics. Consider the dangerous differential diagnoses in all patients with cellulitis
- Evaluate all patients for risk of MRSA as it will change antibiotic choice
- Consult your local antibiogram to determine appropriate antibiotics for your patient
Dong SL et al. ED Management of cellulitis: a review of five urban centers. Am J Emerg Med 2001; 19(7):535-40. PMID: 11698996
Ginsberg MB. Cellulitis: Analysis of 101 cases and review of the literature. South Med J 1981;74:530-533. PMID: 6972617
Kelly EW, Magilner D. Chapter 152. Soft Tissue Infections. In: Tintinalli JE, Stapczynski J, Ma O, Cline DM, Cydulka RK, Meckler GD, T. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e. New York, NY: McGraw-Hill; 2011 (Acess Emergency Medicine)
Liu C et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis 2011;52 (3):285-92. PMID: 21217178
Moran GJ et al. Methicillin-Resistant S. aureus Infections among Patients in the Emergency Department. NJEM 2006; 355(7):666-74. PMID: 16914702
Pallin DJ et al. Clinical trial: comparative effectiveness of cephalexin plus trimethoprim-sulfamethoxazole versus cephalexin alone for treatment of uncomplicated cellulitis: a randomized controlled trial. Clin Infect Dis 2013; 56(12):1754-62. PMID:23457080
Peterson D et al. Predictors of empiric outpatient antibiotic therapy in emergency department patients with uncomplicated cellulitis. Acad Emerg Meds. 2014;21(5):526-31. PMID:24842503
Simonsen SME et al. Cellulitis incidence in a defined population. Epidemiol Infect 2006;134(2):293-9. PMID:16490133
Stevens DL et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the infectious disease society of America. Clin Infect Dis 2014; 59(2):e10-52. PMID: 24973422
Swartz MN. Cellulitis. NEJM 2004; 350(9): 904-12. PMID: 14985488