Definition:
- An inherited disorder that predisposes patients to sudden cardiac death by ventricular arrhythmia that is characterized by the following EKG pattern:
- ST segment elevation with Type 1 Brugada morphology ≥ 2mm in ≥ 1 of the right precordial leads (V1 or V2), spontaneously or after provocative test with intravenous class I anti-arrhythmic medication
- Type 1 Brugada morphology defined as cove-shaped ST segment elevation ≥ 2mm followed by inverted T wave
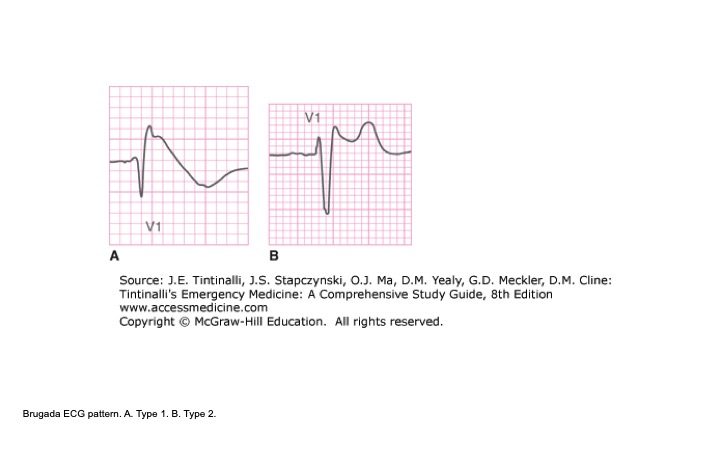
Figure 1: Brugada Pattern (Tintinalli 2016)
- Diagnosis of Brugada syndrome requires characteristic EKG findings and appropriate clinical scenario
- Originally described in 1992 by Pedro and Josep Brugada in their paper entitled “Right Bundle Branch Block, Persistent ST Segment Elevation and Sudden Cardiac Death: A Distinct Clinical and Electrocardiographic Syndrome.” In the paper, they described 8 patients with episodes of aborted sudden death with common clinical and ECG findings, without evidence of electrolyte disturbance, ischemia, or structural heart disease.
Epidemiology: (Sieira J 2016)
- Estimated to be reported in 5-40% of sudden deaths in patients without structural heart disease
- Global prevalence between 5-20 cases per 10,000
- Increased prevalence in Asian countries
Pathophysiology:
- Pathophysiology not completely understood
- Many different genes have been implicated in Brugada syndrome, involving mutations in the sodium channels as well as the calcium and potassium channels.
- 3 different hypotheses exist for mechanism of Brugada syndrome: (Sieira J et al.)
-
- Repolarization: an outward shift in balance of current in right ventricular epicardium results in repolarization abnormalities, leading to closely coupled premature beats which can lead to ventricular arrhythmia.
- Depolarization: conduction delay in the right ventricular outflow tract (RVOT) creates abnormal current leading to ventricular arrhythmia.
- Neural crest: the RVOT has different embryologic origin than rest of the heart, and abnormal expression of these cells could lead to both a depolarization delay and abnormal repolarization in the RVOT
ECG Criteria:
- As above, only Type 1 EKG pattern is diagnostic of Brugada syndrome.
- Type 2 Brugada pattern is characterized by “saddleback” pattern of ST elevation with positive or biphasic T wave. Type 2 is not diagnostic of Brugada Syndrome, but may raise suspicion for Brugada syndrome, and should lead to further testing.
- Type 3 Brugada pattern is characterized by coved or saddle back with ST elevation between 1-2mm. This pattern was initially thought to be suggestive of Brugada syndrome, but is no longer considered suggestive of Brugada syndrome, but is now thought to be a normal variant.
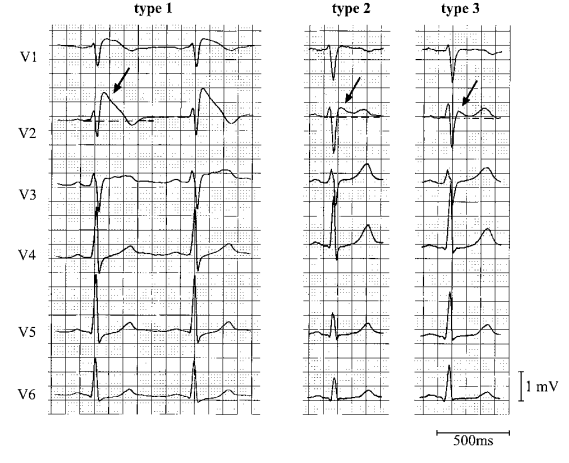
Figure 2: Brugada Types (Wilde 2002)
- Patient’s with Brugada syndrome will not always manifest characteristic EKG at all times
Differential:
- Must consider Brugada Syndrome in all patients presenting with syncope or unexplained cardiac arrest
- Right bundle branch block (RBBB): different in that normal RBBB does not have ST segment elevation
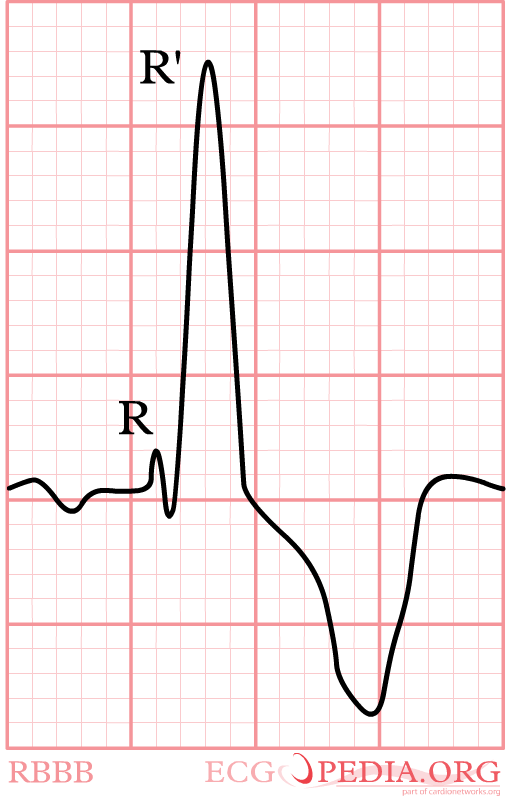
Figure 3: RBBB
- Arrhythmogenic right ventricular cardiomyopathy (ARVC): structural heart disease characterized by fatty replacement and fibrosis of the right ventricle, can also lead to ventricular arrhythmias. EKG shows characteristic Epsilon wave, a small positive deflection buried in the end of the QRS complex.
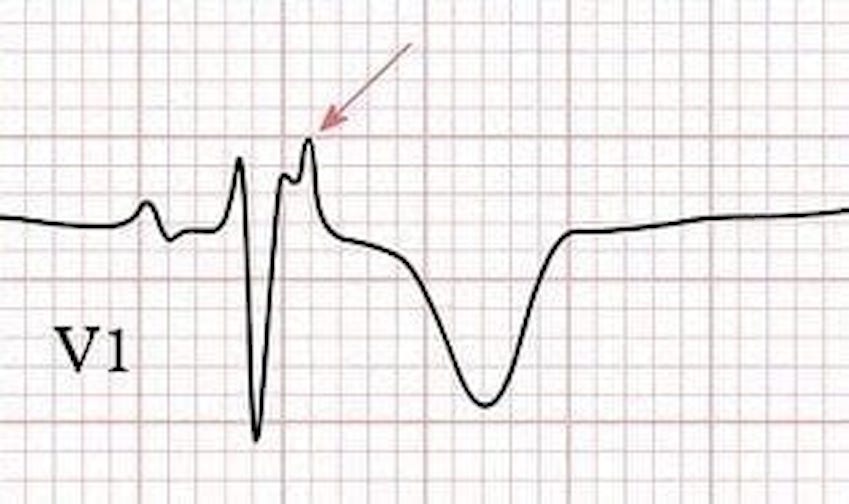
Figure 4: Epsilon wave (LIFTL)
Presentation and Management
- Presentation can vary from incidentally found Brugada pattern on screening EKG, to found in workup of syncope or cardiac arrest
- Implantable cardioverter-defibrillator (ICD) is definitive treatment for patients deemed high risk for ventricular arrhythmia
- Quinidine, a class I antiarrhythmic, has also been used in conjunction with ICD or if unable to place ICD.
Disposition:
- Disposition is controversial and depends on clinical scenario that led to finding of Brugada pattern or diagnosis of Brugada syndrome
- All patients who are symptomatic should be admitted for further workup, electrophysiology studies, and likely ICD placement
- Asymptomatic patients with Type 1 EKG pattern, or patients with Type 2 EKG pattern can be considered for discharge with close cardiology and Electrophysiology follow-up
Special Considerations:
- Fever has been thought to precipitate arrhythmic events in patients with Brugada syndrome, sometimes referred to as “Fever-induced Brugada”
- Recommend that these patient’s have their hyperthermia aggressively treated to avoid inducing potential ventricular arrhythmia
- First EKG below is patient presenting to ED with febrile illness. Second EKG is same patient next day after fever resolved
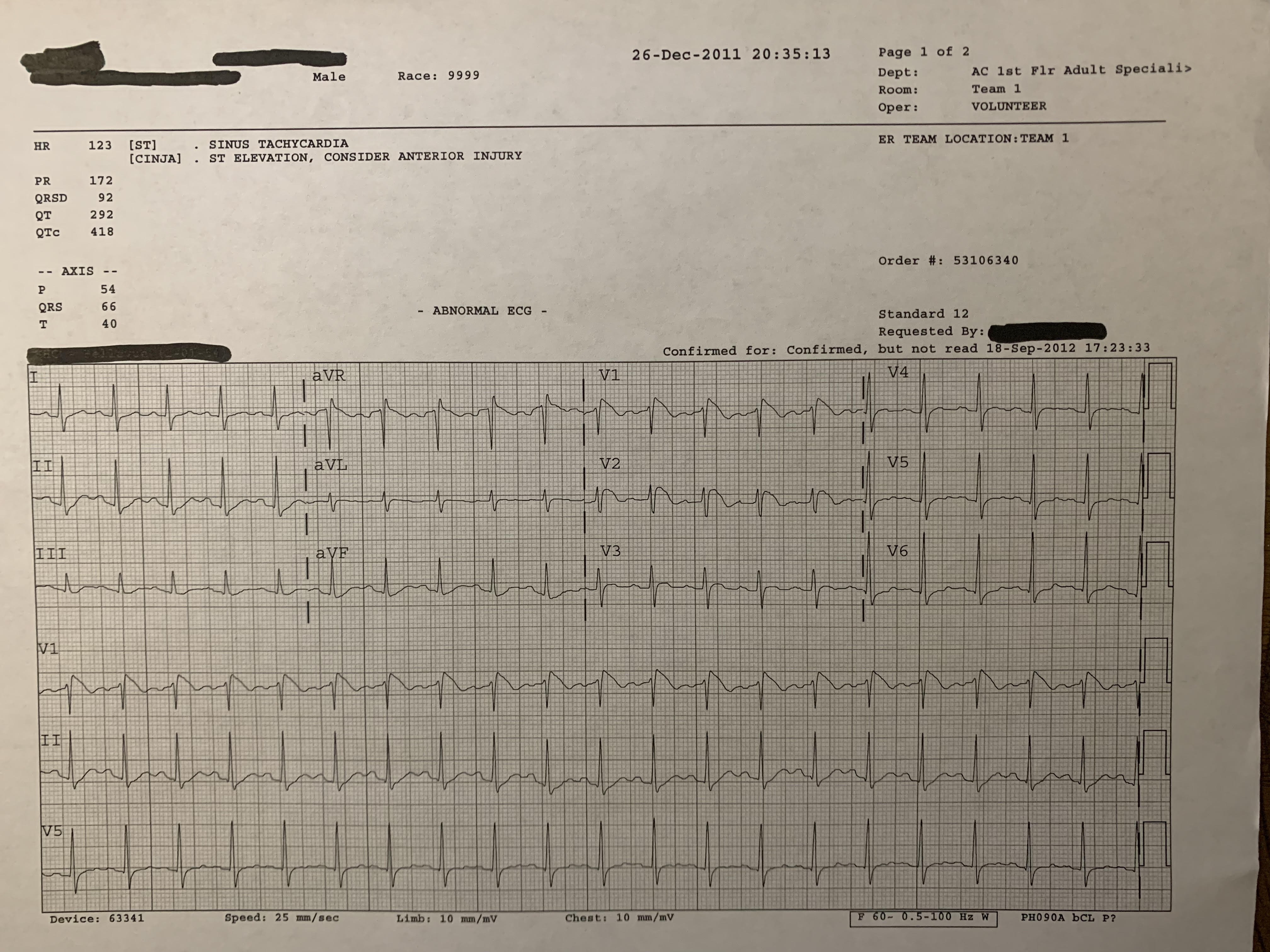
Figure 5: Brugada Febrile
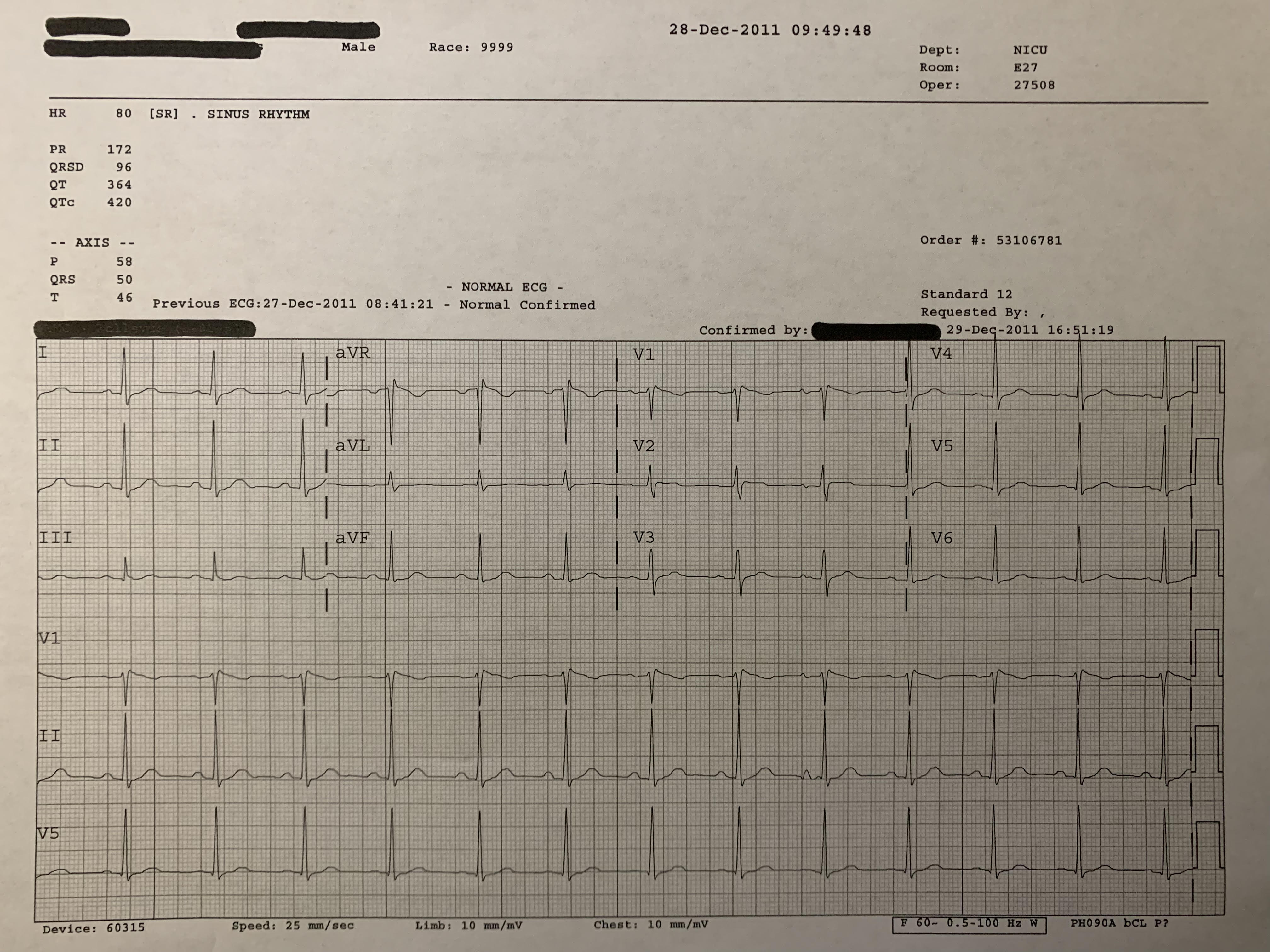
Figure 6: Brugada Afebrile
- Sodium channel blocking drugs should be avoided in these patients for fear of potentiating life threatening ventricular arrhythmias
- BrugadaDrugs.org is a reference that lists medications that should be absolutely or relatively avoided
Take Home Points:
- Must think about Brugada syndrome in any patient presenting with syncope or ventricular arrhythmia
- Only Type 1 Brugada pattern is diagnostic of Brugada syndrome, and only in appropriate clinical context
- Symptomatic patients with Brugada type 1 should be admitted for further workup
- ICD placement is definitive therapy
Read More:
- Life in the Fast Lane: What is Brugada Syndrome?
References:
- Wilde AA et al. Proposed diagnostic criteria for the Brugada syndrome: a consensus report. Circulation. 2002 Nov 5;106(19):2514-9. PMID 12417552
- Tintinalli, Judith E., et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Eighth edition. New York: McGraw-Hill Education, 2016: 133-134
- Sieira J and Brugada P. The definition of the Brugada Syndrome. Eur Heart J. 2017 Oct 21;38(40); 3029-3034. PMID 292020354
- Brugada P and Brugada J. Right Bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992 Nov 15;20(6):1391-6. PMID 1309182
- Brugada P. Brugada syndrome: More than 20 years of scientific excitement. J Cardiol. 2016 Mar’67(3)215-20. PMID 26627541
- Sieira J et al. Pathogenesis and management of Brugada syndrome. Nat Rev Cardiol. 2016 Dec;13(12):744-756. PMID 27629507
- Adler A et al. Fever-induced Brugada pattern: how common is it and what does it mean? Heart Rhythm. 2013 Sep;10(9): 1375-82. PMID 23872691
Figures:
- Figure 1: J.E. Tintinalli, JS Stapczynski, O.J. Ma, D.M Yealy, G.D. Meckler, D.M. Cline: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8th www.accessmedicine.com
- Figure 2: Wilde AA et al. Proposed diagnostic criteria for the Brugada syndrome: a consensus report. Circulation. 2002 Nov 5;106(19):2514-9. PMID 12417552
- Figure 3: https://nl.ecgpedia.org/images/d/d6/RBBB.png
- Figure 4: https://litfl.com/wp-content/uploads/2018/08/Epsilon-Waves.jpg
