Thank you to Salim Rezaie for providing additional peer review for this post.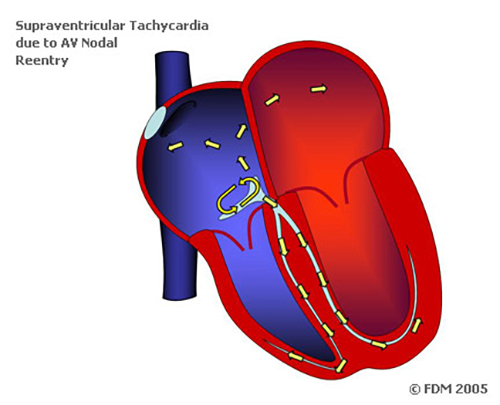
Definition: A regular, narrow-complex rhythm with a ventricular rate that is typically > 160 bpm. Atrioventricular nodal reentrant tachycardia (AVNRT) results from the presence of a reentry circuit in the AV node. This circuit conducts down the bundle of His (resulting in a narrow QRS) and generates retrograde conduction into the atria (inverted P waves buried within the QRS).
AVNRT is also referred to as paroxysmal supraventricular tachycardia (PSVT) or simply supraventricular tachycardia (SVT). However, it is important to understand that SVT is an umbrella term that refers to all tachydysrhythmias that originate above the ventricles including atrial fibrillation and atrial flutter, for example. When describing a supraventricular tachycardia that is due to a re-entrant circuit in the AV node specifically, it is better to use the term AVNRT as opposed to SVT in order to avoid confusion.
Differential to Consider (for Regular, Narrow Complex Tachydysrhythmias)
- Sinus Tachycardia
- AVNRT
- Orthodromic Atrioventricular Reentrant Tachycardia (AVRT)
- Atrial Flutter with 2:1 block
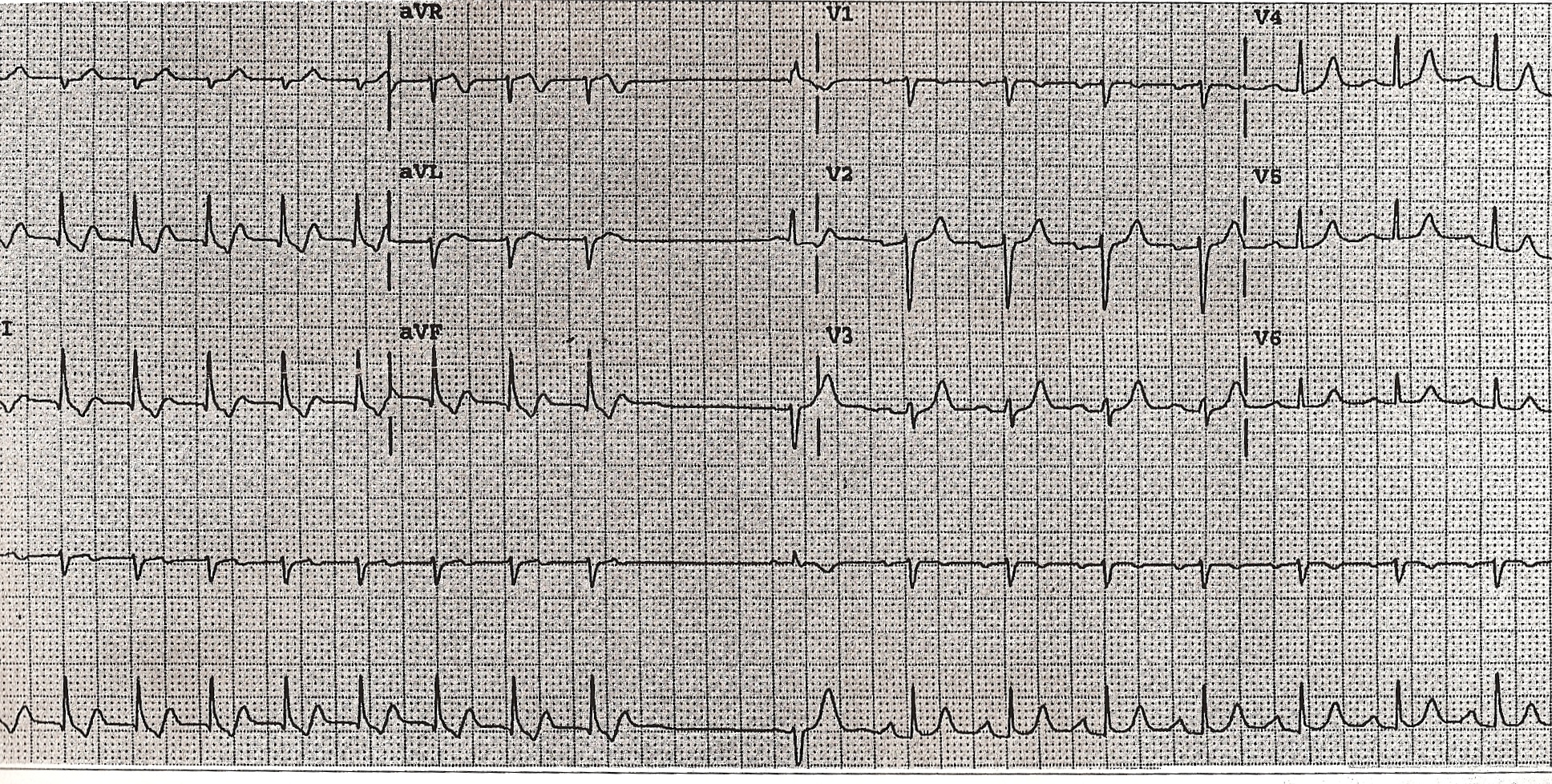
Common EKG Findings
- Narrow-complex, regular rhythm with a rate that often exceeds the theoretical maximal heart rate (220 – age) for that patient.
- Rhythm strip (or monitor): The rhythm is exquisitely regular. Sinus tachycardia and atrial flutter will have some minor variation in rate while AVNRT will not.
- ST depressions are commonly seen in AVNRT and can be diffuse (see EKG 1). These depressions are often rate related and of unknown significance.
AVNRT with Aberrancy
- Although AVNRT typically has a narrow-complex, some patients may demonstrate a wide-complex if the patient has aberrant conduction (baseline right or left bundle branch block or rate related bundle branch block).
- It can be difficult to differentiate AVNRT with aberrancy from ventricular tachycardia (VT). A number of algorithms have been constructed for this purpose, including the Brugada criteria, but none are perfect. Amal Mattu’s ECG Blog has an excellent review of AVNRT vs. VT and REBEL EM reviews the sensitivity and specificity of various algorithms.
- When in doubt, regular, wide-complex tachydysrhythmias should be treated as VT as this is the safest approach.
Immediate Management: The primary goal is to convert the patient back to sinus rhythm.
Basics: ABCs, IV, O2 and Cardiac Monitor
Directed Management
- Establish patient stability
- Unstable: Evidence of end-organ (brain, heart) malperfusion or hypotension. This may manifest as altered mental status, severe lightheadedness, severe shortness of breath or chest pain.
- If the patient is unstable, proceed directly to electrical cardioversion
- If the patient is stable, you may pursue non-pharmacological therapy with vagal maneuvers, electrical cardioversion or chemical cardioversion
- Vagal Maneuvers
- Definition: maneuvers that increase stimulation of the vagal nerve resulting in increased vagal tone breaking the reentrant circuit
- Examples
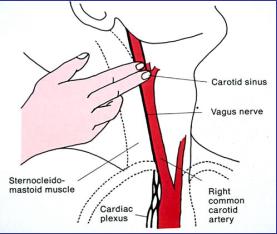
- Carotid massage
- Massage of the carotid sinus at the angle of the mandible
- Caution
- Do not perform bilateral carotid massage as this can markedly decrease blood flow to the brain
- This maneuver is relatively contraindicated in elderly patients or those in whom you hear a bruit over the carotid as there is a theoretical risk of breaking off a carotid artery plaque and causing a stroke.
- Valsalva maneuvers
- Have patient bear down as if they are having a bowel movement
- Have patient blow as hard as they can into a straw
- Syringe technique
- Postural Modification
- Success rate: 43% vs. 17% (standard Valsalva) (Appleboam 2015)
- Details of technique found at the St. Emlyn’s blog
- Have patient bear down as if they are having a bowel movement
- Carotid massage
- Electrical Cardioversion
- Synchronized cardioversion is indicated for unstable patients with AVNRT
- Synchronized cardioversion can also be strongly considered in stable patients with AVNRT
- Dose: 100-200 J
- Perform procedural sedation and analgesia if the patient’s hemodynamics allow
- Chemical Cardioversion
- Adenosine
- A naturally occurring purine nucleoside
- Causes abrupt slowing of all AV conduction (anterograde and retrograde)
- Dose: 6 mg fast IV push. If unsuccessful, dose can be doubled to 12 mg
- Onset of action: 5-20 seconds
- Duration of effect: 30 – 40 seconds
- Key Point: because of adenosine’s short half-life, it must be given through a proximal peripheral IV (antecubital or closer) and as a rapid IV push. An alternate administration approach can be found on ALiEM.
- Adenosine
- Verapamil (Non-dihydropyridine Calcium Channel Blocker)
- Class IV antidysrhythmic agent that slow Ca2+ channels and thus, slow conduction at the AV node and suppresses the SA node.
- Multiple studies comparing verapamil to adenosine demonstrate equal efficacy of either agent with verapamil causing more hypotension (Delaney 2011, Hood 1992)
- Dose: 0.07 mg/kg (most studies gave 5 mg over 2-5 minutes). Dose can be repeated
- Should not be given to pediatric patients as there are reports of profound hypotension and circulatory collapse
- Cardiac troponin is commonly elevated in patients with AVNRT but is often not associated with coronary artery disease (Ben Yedder 2011, Carlberg 2011)
Disposition
- Most adult patients with AVNRT can be discharged after termination of the tachydysrhythmia.
- Pediatric patients should be considered for admission and further cardiology evaluation.
- Patients with frequent recurrences should be sent to a electrophysiologist for follow up.
Take Home Points
- AVNRT is a common tachydysrhythmia that results from a reentrant loop within the AV node.
- Unstable patients with AVNRT should be considered for immediate synchronized electrical cardioversion.
- Stable patients with AVNRT can have a trial of vagal maneuvers followed by chemical cardioversion with adenosine or verapamil and synchronized electrical cardioversion if that fails.
Additional Resources
AVNRT with Aberrancy vs. VT
REBEL EM: SVT with Aberrancy Versus VT
Amal Mattu’s ECG Case of the Week: August 26th, 2013
Valsalva Maneuver
ALiEM: Tricks of the Trade: Valsalva Maneuver By Using a 10cc Syringe
St. Emlyn’s: JC The REVERT Trial
Adenosine in AVNRT
Larry Mellick: Treating SVT with Adensoine
ALiEM: Trick of the Trade: Combining Adenosine with the Flush
Verapamil in AVNRT
RAGE Podcast: Rage Session Two
ERCast Podcast: How to run a code
References
Brugada P et al. A new approach to the diagnosis of regular wide complex tachycardia. Circulation 1991; 83: 1649-59. PMID: 2022022
Appleboam A et al. Postural mdodification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT): a randomised trial. Lancet 2015. PMID: 26314489
Delaney B, Loy J, Kelly AM. The relative efficacy of adenosine versus verapamil for the treatment of stable paroxysmal supraventricular tachycardia in adults: a meta-analysis. Eur J Emerg Med. 2011; 18(3): 148-52. PMID: 20926952
Hood MA, Smith WM. Adenosine versus verapamil in the treatment of supraventricular tachycardia: a randomized double-crossover trial. Am Heart J. 1992; 123(6):1543-9. PMID: 1595533
Ben Yedder N et al. Troponin elevation in supraventricular tachycardia: primary dependence on heart rate. Can J Cardiol 2011; 27(1): 105-9. PMID: 21329868
Carlberg DJ et al. Serum troponin testing in patients with paroxysmal supraventricular tachycardia: outcome after ED care. Am J Emerg Med 2011; 29(5): 545-8. PMID: 20825871
Yealy D, Kosowsky JM: Dysrhythmias, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2010, (Ch) 79: p 1034-63.



Hello again. Maybe I am confused, as I understand it, Orthodromic AVRT is simply a subtype of AVNRT along with antidromic (the 2nd subtype which can create a wide QRS). This isn’t clearly stated in the differential diagnosis. Maybe mention something about the 2 subtypes and the different ECG morphologies.
Another great post, thanks Anand.
@Shane AVNRT and AVRT are not related.
@Anand it should be noted that ECG 1 and ECG 2 shows the rather AVNRT-specific “pseudo s sign” and “pseudo r sign” which establishes the diagnosis of AVNRT and makes further examinations unnecessary. Perhaps I missed it in the text?