Definitions:
- Hypertension (HTN) was previously classified by JNC7 as elevated blood pressure (BP) divided into the following categories (Figure 1)
- Normal: Systolic BP <120, Diastolic BP <80 (mmHg)
- Prehypertension: Systolic BP 120-130, Diastolic BP 80-89
- Stage 1: Systolic BP 140-159, Diastolic BP 90-99
- Stage 2: Systolic BP ≥ 160, Diastolic BP ≥ 100
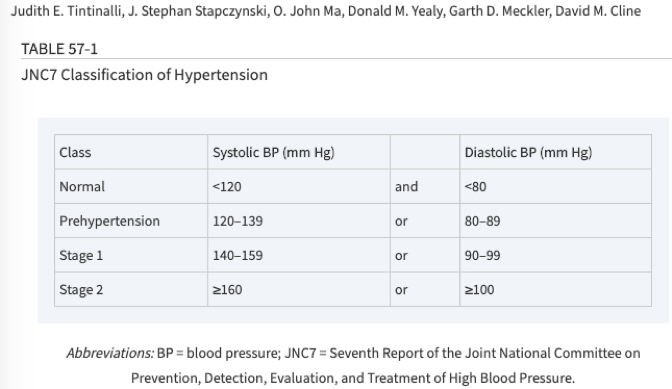
Tintinalli 2016
- Approximately 33% of US adults ≥20 yo have hypertension (Go AS et al. 2014)
- Updated JNC8 guidelines recommend initiation of treatment based on the following scenarios
- Adults ≥60 yo: ≥150/90mmHg
- Adults <60 yo: ≥ 140/90mmHg
- Patients with diabetes: 140/90mmHg, regardless of age
- Important to note, these guidelines are for initiation of medication in outpatient setting, not necessarily in the ED
- Asymptomatic HTN is defined as elevated BP without symptoms/signs indicative of end-organ damage
- HTN in pregnancy is not discussed here, see Core EM: Preeclampsia and Eclampsia
Presentation:
- These patients often present referred from primary care doctors for elevated BP, or may come without referral based on home BP reading.
- Patients may also present for completely unrelated chief complaint, and be found incidentally to have elevated BP
History and Physical Exam:
- History should be focused on searching for evidence of end-organ damage
- Exam should include complete neurologic exam, cardiovascular exam, and pulmonary exam, in addition to routine ED exam
- Symptoms of end-organ damage include:
- Chest pain concerning for acute myocardial ischemia or acute aortic dissection
- Respiratory distress, hypoxia, volume overload
- Focal neurologic deficit
- Vision loss
- Altered mental status
- Seizure
- Severe headache concerning for subarachnoid hemorrhage
- Oliguria
- Patients with asymptomatic hypertension may have mild symptoms such as mild headache or lightheadedness, but this does not necessarily indicate need to search for end-organ damage
Differential Diagnosis:
- Hypertensive emergency: this is what you need to rule out with good history and physical exam!
- Acute pulmonary edema
- Acute myocardial infarction
- Aortic dissection
- Hypertensive encephalopathy
- Hemorrhagic stroke
- Ischemic stroke
- Acute kidney Injury
Diagnostics:
- If symptoms/signs are suggestive of acute end-organ damage, diagnostics can be performed to further evaluate—this is not asymptomatic hypertension! (For example Chest X-Ray to evaluate for pulmonary edema, EKG and troponin to evaluate for myocardial infarction, Head CT to evaluate for hemorrhagic stroke).
- In absence of signs/symptoms of acute end-organ damage (true asymptomatic hypertension), no routine screening is necessary per ACEP clinical policy (see below).
- A prospective observational study of 109 patients with asymptomatic hypertension ≥180/90mmHg, showed only 5% of patients had a meaningful unanticipated abnormality on screening tests, and no patients had findings indicative of hypertensive emergency. (Karras DJ 2008)
- Retrospective propensity matched cohort study of 58,535 clinic patients with asymptomatic HTN ≥180/110mmHg, emergency department referral showed no significant difference in major adverse cardiac events at 7 days, 8-30 days, or 6 months. Only 5.5% of tests ordered on patients sent to the ED were abnormal, and only 2.1% had evidence of target organ injury. None (0/60) of the Head CT or Chest CTs that were ordered were abnormal. (Patel KK 2016)
Management:
- In the absence of symptoms/signs of end-organ damage or hypertensive emergency, management goal should be to reduce BP gradually on outpatient basis
- Emergent rapid lowering of blood pressure in the absence of symptoms/signs of end-organ damage is discouraged due to the concern for decreased cerebral perfusion
- Acute BP reduction does not appear to provide any benefit (Levy PD 2015)
- Depending on patient-specific factors and ease of accessibility to follow-up, it may be reasonable to initiate oral anti-hypertensives in the emergency department
- Initial therapy recommendations for non-Black individuals are a thiazide diuretic, an ACE-inhibitor or a calcium channel blocker.
- Initial therapy recommendations for Black individuals are a thiazide diuretic and/or calcium channel blocker.
- Patients with chronic kidney disease should have an ACE-inhibitor or angiotensin receptor blocker started, regardless of race or diabetic status. (Tintinalli 8th Ed)
- See figure below for testing needed before initiation of different classes of antihypertensives
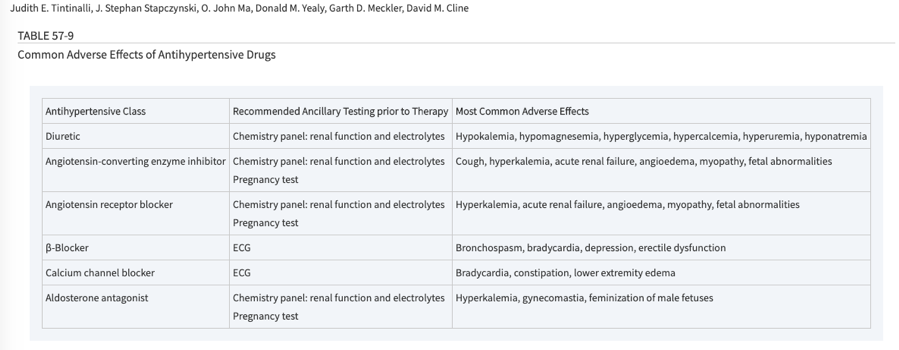
Tintinalli 2016
ACEP Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients in the Emergency Department With Asymptomatic Elevated Blood Pressure (Feb 2013)
- Level C Recommendation: (1) In ED patients with asymptomatic markedly elevated blood pressure, routine screening for acute target organ injury (eg, serum creatinine, urinalysis, ECG) is not required. (2) In select patient populations (eg, poor follow-up), screening for an elevated serum creatinine level may identify kidney injury that affects disposition (eg, hospital admission).
- Level C Recommendation: (1) In patient with asymptomatic markedly elevated blood pressure, routine ED medical intervention is not required. (2) In select patient populations (eg, poor follow-up), emergency physicians may treat markedly elevated blood pressure in the ED and/or initiate therapy for long-term control. (3) Patients with asymptomatic markedly elevated blood pressure should be referred for outpatient follow-up.
- Level C Recommendation is defined as recommendations for patient care that are based on evidence from Class of Evidence III studies, or in the absence of adequate published literature, based on expert consensus
Take Home Points:
- Hypertension is extremely common in our patient population and a common presenting chief complaint
- Important to distinguish asymptomatic hypertension from hypertensive emergency which requires admission and acute intervention
- In patients with asymptomatic hypertension without evidence of hypertensive emergency, no routine screening is required and routine ED medical intervention is not required.
- Importance of prompt primary care follow-up, with or without initiation of oral antihypertensive medication.
References:
- James PA, et al. 2014 Evidence-Based Guidline for the Management of High Blood Pressure in Adults: report from the panel members appointed to the Eigth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520. Doi:10.1001/jama.2013.284427. PMID 24352797
- Viera AJ. Hypertension Update: Hypertensive Emergency and Asymptomatic Severe Hypertension. FP Essent. 2018 Jun;469:16-19. PMID 29863318
- Go AS et al. Heart disease and stroke statistics – 2014 update: a report from the American Heart Association. Circulation. 2014 Jan 21;129(3). PMID 24352519
- Tintinalli, Judith E., et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Eighth edition. New York: McGraw-Hill Education, 2016: 399-409.
- Varon J, Elliott WJ. Management of severe asymptomatic hypertension (hypertensive urgencies) in adults. UpToDate. Feb 2019. Link
- Levy PD et al. Blood pressure treatment and outcomes in hypertensive patients without acute target organ damage: a retrospective cohort. Am J Emerg Med. 2015 Sep;33(9):1219-24. PMID 26087706
- Karras DJ et al. Utility of routine testing for patients with asymptomatic severe blood pressure elevation in the emergency department. Ann Emerg Med. 2008 Mar;51(3):231-9. PMID 17499391
- Patel KK et al. Characteristics and Outcomes of Patients Presenting with Hypertensive Urgency in the Office Setting. JAMA Intern Med. 2016 Jul 1;176(7):981-8. PMID 27294333
Figures:
- Figure 1: Baumann BM. Systemic Hypertension. In: Tintinalli, Judith E., et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Eighth edition. New York: McGraw-Hill Education, 2016. Available at https://accessemergencymedicine-mhmedical-com.ezproxy.med.nyu.edu/content.aspx?bookid=1658§ionid=109388371 Accessed May 28 2019.
- Figure 2: Baumann BM. Systemic Hypertension. In: Tintinalli, Judith E., et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Eighth edition. New York: McGraw-Hill Education, 2016. Available at https://accessemergencymedicine-mhmedical-com.ezproxy.med.nyu.edu/content.aspx?bookid=1658§ionid=109388371 Accessed June 3 2019.

I am so grateful for this update. It is my practice NOT to treat asymptomatic hypertension in the emergency department.