
Background
- Around 6 million people in the U.S. are on oral anticoagulants (Ref 1)
- Common causes for oral anticoagulation uses include:
- Atrial fibrillation
- Venous thromboembolism
- Stroke
- Heart valve replacement
- The number of patients on direct oral anticoagulants is steadily increasing, and about 3% experience life-threatening bleeding annually (Ref 2)
- Anticoagulation status leads to increased mortality despite the availability of reversal agents in patients with severe bleeding (ref 2)
Indications for Anticoagulation Reversal
- Life-threatening bleeding as defined (Ref 1, 5) by a:
- Hemoglobin drop of 5 g/dL or more compared to baseline and requiring blood transfusion
- Bleeding that requires intervention (surgery, endoscopy, IR)
- Vital sign instability requiring vasoactive medications (i.e., pressors) or ongoing volume resuscitation
- Bleeding at critical site (brain, eye, spine, airway, pericardium, aorta, or closed space with potential for compartment syndrome)
- Emergent surgery
Procedures in the Emergency Room
- The majority of procedures done in the ED do not require screening with coagulation laboratory tests or reversal due to low bleeding risk (ref 9); these include:
- Dialysis access, lumbar puncture, non-tunneled chest tube placement, paracentesis, peripheral nerve blocks, thoracentesis, tunneled venous catheter removal/placement (ref 9)
Laboratory Evaluation:
- Obtain CBC, BMP, LFTs, PT/INR, aPTT, anti-FXa activity, fibrinogen, type and screen
- INR will be elevated in patients taking warfarin
- PT might be elevated in patients taking rivaroxaban, sensitive but not specific (ref 7, 12)
- PT and aPTT prolonged by rivaroxaban (Ref 12)
- Anti-FXa activity will reflect factor Xa inhibitors activity (ref 7)
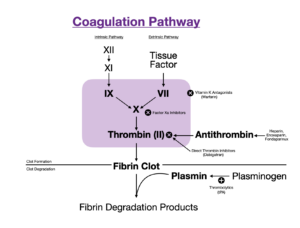
Pathophysiology of Common Anticoagulants
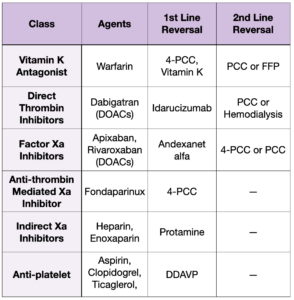
Common Reversible Agents
- Vitamin K
- Used for warfarin reversal
- Necessary for hepatic synthesis of factors II, VII, IX, and X
- PO and subcutaneous Vitamin K require 12 and 24 hours to work (ref 12); IV is preferred in the emergent/urgent setting
- IV Vitamin K is associated with non-dose-dependent anaphylaxis and overcorrection of Vitamin K antagonists; as such, its use should be restricted to life-threatening bleeding
- 4-Factor – PCC
- Also known as Kcentra
- Replaces deficient factors (II, VII, IX, X, protein C, protein S, heparin, albumin)
- The first line and only therapy that is FDA-approved for warfarin reversal (ref 5)
- 3-Factor-PCC
- Contains factors II, IX, and X
- Commonly used for Hemophilia B
- Fresh Frozen Plasma – FFP
- Plasma proteins, including albumin, all coagulation factors and fibrinogen
- 250-300 cc
- Used if PCC is not available
- Compared to PCCs, larger volume, longer infusion time, increased pathogen transmission risk (ref 11)
- FFP may take up to 3- 6 hours for reversal (Ref 12)
- Cryoprecipitate
- Contains a concentrated version of FFP including Factor VIII, vWF, fibrinogen
- Requires thawing and cannot be administered as fast as FFP
- 10-15 cc of volume per 1 unit
- Recombinant XIIa
- Contains Factor VIIa
- Used for Hemophilia patients
- Idarucizumab
- Reversal for direct thrombin inhibitor (Dabigatran)
- Irreversibly binds and inactivates direct thrombin inhibitor
- Andexanet alfa (ref 10,11)
- Reversal for factor Xa inhibitors
- Reversibly binds and inactivates the Xa inhibitors
- Considerations:
- Expensive
- It may not be available in all hospitals
- Results in an increased thrombotic state
- Protamine
- Reversal for heparin
- Binds heparin and makes it inactive
- Short half-life and might require re-dosing
- Tranexamic acid
- Inhibits the breakdown of fibrin
- Thought to be beneficial in hemorrhage control (CRASH-2, WOMAN trials)
- Desmopressin (DDAVP)
- A synthetic analog of vasopressin that acts on endothelial calls via an increase of cAMP to increase circulating vWF and Factor VIII (Ref 13)
- May be used in life-threatening bleeding with platelet dysfunction (e.x, uremia) or in the setting of anti-platelet therapy
- Also used in patients with Hemophilia A and Von Willebrand Disease
Special Situations
- If bleeding is not improving despite reversal agents, consider alternative diagnosis such as DIC (ref 5)
- Use charcoal if ingestion of PO anticoagulant within 2-4 hours (ref 5, 11)
- Patients with renal disease: (ref 1)
- Might have platelet dysfunction due to uremia; consider desmopressin
- Might benefit from hemodialysis for dabigatran reversal
- Patients with liver disease: (ref 1)
- Will have coagulation abnormalities, especially vitamin K-dependent factors
- All PCCs carry a risk of pro-thrombotic side effects (ref 7)
- Platelet transfusion for a patient bleeding on an anti-platelet is not indicated and might negatively affect outcome (PATCH trial)
- Consider and discuss with consultants platelet transfusion if platelets <50 and an invasive procedure is planned
References:
- Tomaselli GF, Mahaffey KW, Cuker A, et al. 2017 ACC Expert Consensus Decision Pathway on Management of Bleeding in Patients on Oral Anticoagulants: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2017;70(24):3042-3067. doi:10.1016/j.jacc.2017.09.1085
- Gómez-Outes A, Alcubilla P, Calvo-Rojas G, et al. Meta-Analysis of Reversal Agents for Severe Bleeding Associated With Direct Oral Anticoagulants. J Am Coll Cardiol. 2021;77(24):2987-3001. doi:10.1016/j.jacc.2021.04.061
- Thomas S, Makris M. The reversal of anticoagulation in clinical practice . Clin Med (Lond). 2018;18(4):314-319. doi:10.7861/clinmedicine.18-4-314
- Kuramatsu JB, Sembill JA, Huttner HB. Reversal of oral anticoagulation in patients with acute intracerebral hemorrhage. Crit Care. 2019;23(1):206. Published 2019 Jun 6. doi:10.1186/s13054-019-2492-8
- Baugh CW, Levine M, Cornutt D, et al. Anticoagulant Reversal Strategies in the Emergency Department Setting: Recommendations of a Multidisciplinary Expert Panel. Ann Emerg Med. 2020;76(4):470-485. doi:10.1016/j.annemergmed.2019.09.001
- Gilbert BW, Morton L, Huffman JB, et al. Modified version of the American College of Cardiology’s recommendation for low-dose prothrombin complex concentrate is effective for warfarin reversal. Am J Emerg Med. 2020;38(4):806-809. doi:10.1016/j.ajem.2019.12.005
- Kaide CG, Gulseth MP. Current Strategies for the Management of Bleeding Associated with Direct Oral Anticoagulants and a Review of Investigational Reversal Agents. J Emerg Med. 2020;58(2):217-233. doi:10.1016/j.jemermed.2019.10.011
- Bitonti MT, Rumbarger RL, Absher RK, Curran LM. Prospective Evaluation of a Fixed-Dose 4-Factor Prothrombin Complex Concentrate Protocol for Urgent Vitamin K Antagonist Reversal. J Emerg Med. 2020;58(2):324-329. doi:10.1016/j.jemermed.2019.10.013
- Patel IJ, Rahim S, Davidson JC, et al. Society of Interventional Radiology Consensus Guidelines for the Periprocedural Management of Thrombotic and Bleeding Risk in Patients Undergoing Percutaneous Image-Guided Interventions-Part II: Recommendations: Endorsed by the Canadian Association for Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe. J Vasc Interv Radiol. 2019;30(8):1168-1184.e1. doi:10.1016/j.jvir.2019.04.017
- Connolly SJ, Milling TJ Jr, Eikelboom JW, et al. Andexanet Alfa for Acute Major Bleeding Associated with Factor Xa Inhibitors. N Engl J Med. 2016;375(12):1131-1141. doi:10.1056/NEJMoa1607887
- Milling TJ, Pollack CV. A review of guidelines on anticoagulation reversal across different clinical scenarios – Is there a general consensus?. Am J Emerg Med. 2020;38(9):1890-1903. doi:10.1016/j.ajem.2020.05.086
- Thigpen JL, Limdi NA. Reversal of oral anticoagulation. Pharmacotherapy. 2013;33(11):1199-1213. doi:10.1002/phar.1270
- McCarty TS, Patel P. Desmopressin. [Updated 2023 Jun 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554582/
