Definition:
- An abrupt, multisystem emergency caused by the precipitous release of mast cell (skin) and basophil (blood) generated chemicals into the circulation
- Functional Emergency Medicine Approach: is there a compromise to airway, breathing or circulation and a possible allergen exposure? If so, it’s likely anaphylaxis.
- Useful to consider allergy and anaphylaxis as spectrum- allergy is on the benign end, anaphylaxis is somewhere near the middle, and anaphylactic shock is at the other extreme (Davis 2011)
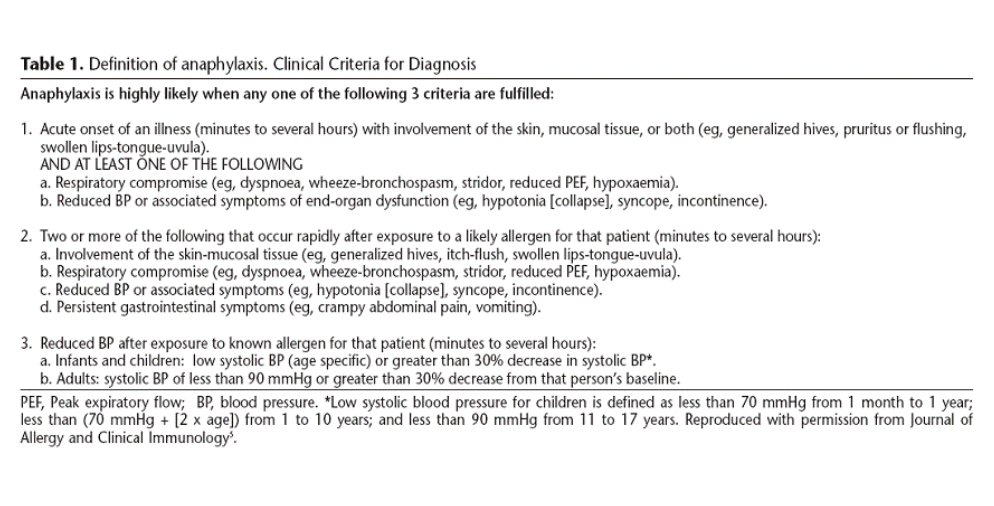
Anaphylaxis Definition (Second National Institute of Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network)
Anaphylactic (Immunologic) vs. Anaphylactoid (Non Immunologic)
- Anaphylactic (Immunologic)
- IgE Dependent (Type I Hypersensitivity) Reactions
- Requires prior sensitization to inciting agent
- Allergen cross-links two or more IgE molecules on mast cells or basophils and initiates a signal cascade leading to degranulation
- Generation of mediators (histamine, heparin, leukotriene, tryptase, and prostaglandin D2)
- Increases vascular permeability
- Recruits cells, like eosinophils, to cause fulminant allergic reaction
- IgE Dependent (Type I Hypersensitivity) Reactions
- Anaphylactoid (Non Immunologic)
- Mast cells and basophils are activated directly by certain agents (i.e. meperidine, radiocontrast agents, vancomycin)
Epidemiology:
- Lifetime prevalence anaphylaxis 0.05% to 2% (Simons 2010)
- Increasing in children and adolescents
- 1% ED visits allergy-related (Grunau 2015)
Presentation (Davis 2011):
|
Signs and Symptoms |
Frequency (%) |
|
Urticaria and angioedema |
85-90 |
|
Dyspnea and wheeze |
45-50 |
|
Upper airway angioedema |
50-60 |
|
Rhinitis |
15-20 |
|
Dizziness, syncope, hypotension |
30-35 |
|
Nausea, vomiting, diarrhea, cramping |
25-30 |
|
Headache |
5-8 |
|
Seizure |
1-2 |
- When patients die from anaphylaxis, they typically die from upper and lower airway obstruction or cardiovascular collapse
Differential (Simons 2010):
- Angioedema
- Carcinoid syndrome
- Acute asthma
- Shock
- Red Man Syndrome
- Pheochromocytoma
- Scrombroidosis
- Vocal cord dysfunction
Which patients do poorly with anaphylaxis? (Simons 2010)
- Pulmonary pathology (i.e. asthma, COPD, pulmonary fibrosis)
- Cardiovascular disease
- Mast cells are implicated in clot formation in coronary arteries, anaphylaxis may propagate clot burden (Kounis Syndrome)
- Providers may be reluctant to administer life-saving medications in anaphylaxis (i.e. epinephrine) for fear of causing cardiac ischemia
- Use of Beta Blockers, ACE inhibitors (ACEi), Alpha Blockers
- Interfere with patient’s ability to compensate for the massive physiological derangements
- Interfere with patient’s ability to respond to targeted treatments
- Beta blockers reduce bronchodilator and cardiovascular responses to beta-adrenergic stimulation by epinephrine
- Alpha blockers may reduce epinephrine’s effect at the alpha receptors
- ACEi block effect of angiotensin and the degradation of kinins which help alleviate the symptoms and signs of anaphylaxis
Management:
- Rapid recognition and treatment is key
- In a series of 164 fatalities from anaphylaxis, median time interval between onset of symptoms and respiratory or cardiovascular collapse was 5 minutes in iatrogenic anaphylaxis, 15 minutes with stinging insect venom, and 30 minutes for food allergies (Pumphrey 2000)
- Basics- ABCs, IV, O2, Cardiac Monitor, Epinephrine
- Potentially anatomically challenging airway
- Airway edema can rapidly obscure visualization of the cords and necessitate a surgical airway. Intubate early if airway compromise is present
- Edema of the anterior tongue, base of the tongue, or larynx significantly increases the likelihood of intubation or surgical airway management.
- Consider fiberoptic laryngoscopy in stable patients with isolated anterior tongue edema time permitting (McCormick 2011)
- Avoid unnecessary airway manipulation (can exacerbate edema)
- Epinephrine (Adrenaline) (Campbell 2016, Sheikh 2009)
- Early administration of epinephrine (adrenaline) is the most important intervention in anaphylaxis. It is life-saving and intubation-sparing.
- 300 to 500 mcg epinephrine to outer thigh, repeat every 5 to 15 minutes as clinically necessary
- Repeat dose IM epinephrine necessary in 12-36% of cases (Davis 2011)
- Repeat epinephrine doses more commonly needed in those with a prior episode of anaphylaxis or who present with flushing, diaphoresis, or shortness of breath
- Mechanism
- Beta-1 adrenergic agonist: augments inotropy and chronotropy
- Beta-2 adrenergic agonist: triggers bronchodilation and decreases mediator release
- Alpha-1 adrenergic agonist: increases vasoconstriction, peripheral vascular resistance, reduces mucosal edema
- Avoid subcutaneous administration: local vasoconstrictor activity leads to slow and erratic absorption if given subcutaneously
- Intravenous Epinephrine
- Dose
- Bolus: 5-20 mcg over 1 min
- Drip: 1-5 mcg/min and titrate
- Use IV epinephrine with caution as dosing errors commonly occur
- Dose
- Incorrect dosing can cause myocardial ischemia/infarction and ventricular arrhythmias
- Side Effects
- Restlessness, anxiety, dizziness, palpitations, tremor
- Anaphylaxis Refractory to Epinephrine
- Hypotensive patient may not perfuse muscles
- Start IV epinephrine
- See dosing above
- Quick epinephrine drip
- Add 1 mg epinephrine (crash cart “amp”) to 1 L normal saline
- Yield is a 1 mcg/1 ml epinephrine solution
- Methylene blue
- Inhibits nitric oxide synthase and guanylate cyclase to increase systemic vascular resistance
- 1 to 2 mg/kg over 20 to 60 minutes
- Start IV epinephrine
- Special Considerations
- Beta blockers
- Anaphylaxis resistant to epinephrine
- Give glucagon 1 to 5 mg IV in adults over 5 minutes
- Elevates cyclic AMP levels and bypasses the beta receptor
- May cause nausea and vomiting
- MAOis (inhibit epinephrine metabolism) and/or tricyclics (extend duration of action)
- Beta blockers
- Hypotensive patient may not perfuse muscles
- Adjunctive Medications (non-lifesaving) (Campbell 2016)
- H1 antihistamines: 2nd generation Cetirizine (oral) or Diphenhydramine (IV) to relieve itch and urticarial 25 to 50 mg IV, max 400 mg/24 hours
- H2 antihistamines: Ranitidine 50 mg IV
- Inhaled B2 agonist (albuterol)
- Will not prevent or relieve upper airway mucosal edema
- Corticosteroids
- Methylprednisolone: 1-2 mg/kg IV
- Prednisone: 1 mg/kg PO
Biphasic Reactions
- Older studies had suggested a biphasic reaction rate between 1 and 20% (Campbell 2016). This included patients with minor biphasic reactions (i.e. hives)
- Recent literature suggests that clinical significant biphasic reactions are rare (0.18%) (Grunau 2014)
Disposition
- There is no “safe” observation period as biphasic reactions can occur up to days after the initial presentation
- If symptoms resolve after single dose epinephrine, observation may not be useful
- Discharge home
- Give prescriptions for epinephrine auto-injectors (EpiPen®) (2-3) and a course of corticosteroids
- Instruct individuals on how to use epinephrine auto-injectors
- Consider prolonged observation (4-8 hours) of patients requiring multiple doses of epinephrine
- Consider admission
- Patients with anaphylactic shock on presentation (regardless of response to epinephrine)
- Patients with continued symptoms after epinephrine administration (beyond skin findings)
Take Home Points:
- Rapid recognition is critical. If the patient has compromise to airway, breathing or circulation in the setting of an allergen exposure, anaphylaxis is extremely likely.
- The most important step in management of anaphylaxis is early administration of epinephrine. Epinephrine is life-saving.
- Airway edema can occur rapidly making intubation difficult and a surgical airway necessary. Intubate early if you suspect considerable airway compromise
- Prior to discharge, ensure that patients have access to epinephrine auto- injectors and know how to use them
Read More
General Management
The Crashing Patient: Allergy, Hypersensitivity, Anaphylaxis
First 10 EM: Management of Severe Anaphylaxis in the Emergency Department
Core EM: Episode 52.0 – Anaphylaxis
Biphasic Anaphylaxis
SGEM#57: Should I Stay Or Should I Go (Biphasic Anaphylactic Response)
REBEL Cast Episode 1: Clinically Important Biphasic Anaphylaxis
Core EM: Biphasic Reactions in Emergency Department Patients with Allergic Reactions or Anaphylaxis
References
Grunau BE et al. Incidence of clinically important biphasic reactions in emergency department patients with allergic reactions or anaphylaxis. Ann Emerg Med 2014; 63: 736-44. PMID 24239340
Campbell RL et al. Evaluation of national institute of allergy and infectious diseases/food allergy and anaphylaxis network criteria for the diagnosis of anaphylaxis in emergency department patients. J Allergy Clin Immunol. 2012; 129(3): 748-52. PMID 22051698
Campbell et al. Anaphylaxis: Emergency Treatment. In: UptoDate, Feldwed AM (ed.) 2016, UptoDate, Waltham, MA. Link
Davis JE, Norris RL. Chapter 19: The Crashing Anaphylaxis Patient. Emergency Department Resuscitation of the Critically Ill. 2011, ACEP, Dallas, TX. 177-185.
McCormick M et al. Site involvement as a predictor of airway intervention in angioedema. Laryngoscope. 2011;121:262–266. PMID 21271571
Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy. 2000;30(8):1144. PMID 10931122
Sheikh A et al. Adrenaline for the treatment of anaphylaxis: Cochrane systematic review. Allergy 2009; 64(4):204-12. PMID 19178399
Simons FE. Anaphylaxis. J Allergy Clin Immunol 2010; 125: S161-81. PMID 20176258