Definition
- Acute rhinosinusitis (ARS) – Symptoms for less than four weeks
- Subacute rhinosinusitis – Symptoms for 4 to 12 weeks
- Chronic rhinosinusitis – Symptoms persisting greater than 12 weeks
- Recurrent acute rhinosinusitis – Four or more episodes of ARS per year, with interim symptom resolution
Epidemiology (Anon 2004)
- 20 million cases of sinusitis annually in the US, costing $3.5 billion/year
- Source of 1 in 5 antibiotic prescriptions for adults
Acute Sinusitis (JAMA)
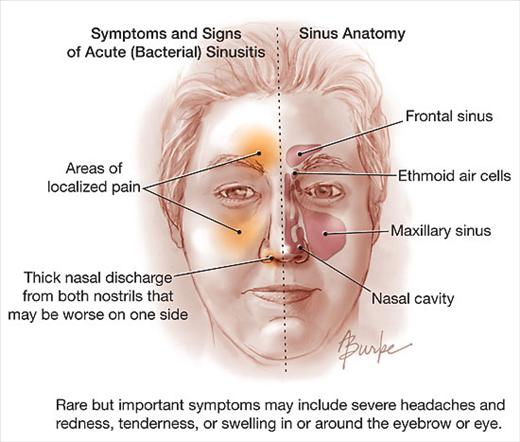
Presentation
- Sinusitis is most commonly diagnosed by clinical symptoms
- Common symptoms
- Purulent nasal discharge
- Nasal congestion
- Facial pain or pressure, especially over a sinus or unilaterally
- Anosmia
- Hyposmia
- Fever
- Cough
- Fatigue
- Maxillary pain
- Ear pressure or fullness
Classification of Sinusitis
- Acute viral rhinosinusitis (AVRS)
- ARS with viral etiology (i.e. rhinovirus, influenza, and parainfluenza)
- Most common form of ARS
- Uncomplicated acute bacterial rhinosinusitis (ABRS)
- ARS with a bacterial etiology without clinical evidence of extension outside the paranasal sinuses and nasal cavity
- Bacterial superinfection: 0.5-2% of all ARS
- Complicated acute bacterial rhinosinusitis
- ARS with bacterial etiology with clinical evidence of extension outside the paranasal sinuses and nasal cavity
Viral vs. Bacterial:
- Color change in sputum does not determine whether infection is viral or bacterial
- Viral infections
- Tend to begin resolution by 7-10 days
- Rarely have associated fevers
- If fever present, usually only in the first 48 hours.
- Guidelines for diagnosing ABRS are
- Presence of URI/cold symptoms that
- Don’t improve after 10 days
- Worsen after 5-7 days of improvement
- Severe symptoms including high fever, purulent discharge or facial pain for 3-4 days
- Presence of URI/cold symptoms that
The Data Behind Antibiotic Use
- Clinically diagnosed acute sinusitis
-
- Multiple studies show the same cure rate at 7 days, but improved cure rate at 7-14 days for those who use antibiotics (Lemiengre 2012, Berg 1986, Gwaltney 1996)
-
IDSA Recommendations for the Treatment of Acute Sinusitis
Overall Treatment Effect NNT = 18
- Overall Harm NNH = 8 (mostly GI side effects)
- Radiographically-diagnosed acute sinusitis (Ahovuo-Saloranta 2008)
- Endpoint: clinical cure at 7-15 days
- NNT = 15
- NNH = 8
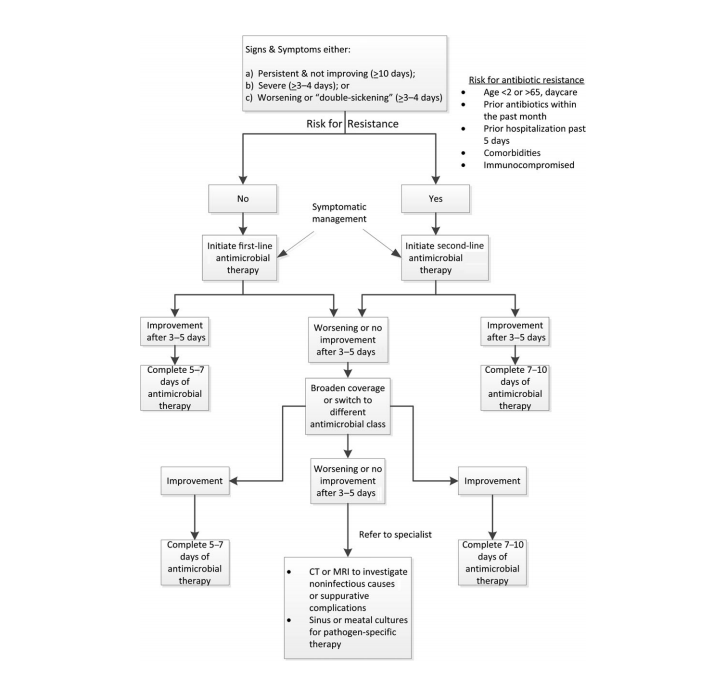
IDSA Recommendations for Antibiotic Treatment (Chow 2012)
- Patients that should be treated
- Persistent symptoms w/o improvement (> 10 days)
- Severe symptoms (> 3-4 days)
- Worsening (“double-sickening”) (> 3-4 days)
- Antimicrobials
- 1st Line
- Amoxicillin 875 mg PO BID X 5-7 days
- Doxycycline 100 mg PO BID X 5-7 days
- 2nd Line
- Amoxicillin/Calvulanate 875/125 mg PO BID X 5-7 days
- Levofloxacin 500 mg PO Q24 X 5 days
- 1st Line
Bottom Line: Given the risk for adverse events associated with antibiotic use, the growing specter of resistance and the lack of significant differences in outcomes with antibiotic use, it is better to avoid antibiotics in most patients with ARS. Antibiotics should be considered in those with severe disease and in immunocompromised patients
Take Home Points
- Acute rhinosinusitis is a clinical diagnosis
- The vast majority of acute rhinosinusitis cases are viral in nature and do not require antibiotics
- Consider the use of antibiotics in select groups with severe disease or worsening symptoms after initial improvement
References
Anon JB et al. Antimicrobial treatment guidelines for acute bacterial rhinosinusitis. Otolaryngol Head Neck Surg 2004; 130(Suppl 1): 1-45. PMID: 14726904
Lemiengre MB et al. Antibiotics for Clinically Diagnosed Acute Rhinosinusitis in Adults. Cochrane Database Syst Rev 2012. PMID: 23076918
Berg O et al. Occurence of asymptomatic sinusitis in common cold and other acute ENT-infections. Rhinology 1986; 24(3): 223-5. PMID: 3775189
Gwaltney JM. Acute community-aquired sinusitis. Clin Infect Dis 1996; 23(6): 1209-23. PMID: 8953061
Ahovuo-Saloranta A et al. Antibiotics for acute maxillary sinusitis. Cochrane Database Syst Rev 2008. PMID: 18425861
Chow AW et al. IDSA Clinical practice guideline for acute bacterial rhino sinusitis in children and adults. Clin Infect Dis 2012; 54(8): e72-e112. PMID: 22438350