Definition: 3 distinct clinical entities caused by acute hypoxia at elevation. Usually occurs at >2500 meters above sea level.
- At altitudes greater than 2440 meters, the decrease in partial pressure of ambient air and thus the alveoli will result in a decrease in the oxygen saturation in healthy people (Hacket 2011)
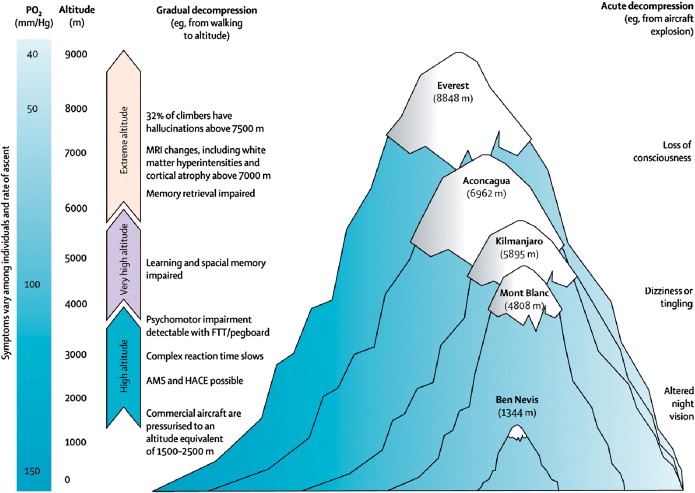
Acute Mountain Sickness Visual (sciencedirect.com)
Acute Mountain Sickness (AMS)
- Definition: Constellation of symptoms including headache with some combination of anorexia, nausea, nausea, dizziness, sleep disturbances, malaise caused by hypoxia at altitudes >2500 meters above sea level
- Epidemiology
- 10-25% of all unacclimated persons at 2500m or higher (Bartsch 2013)
- Increases 50-85% of people at 4500-5500 meters
- Can occur at lower altitudes in persons with cardiopulmonary disease
- Presentation
- Headache with some combination of anorexia, nausea, nausea, dizziness, sleep disturbances, malaise
- Onset usually 6-12 hours at >2500 meters
- Risk factors:
- Previous acute mountain sickness
- Fast ascent (>625 meters per day above 2000 meters)
- Sleeping at altitude
- Course: usually resolves in 1-2 days if person maintains elevation but can last longer
- Lake Louise Acute Mountain Sickness Questioner tool indicates disease severity
- Treatment
- Stop Ascent
- Descend immediately: altered mental status, ataxia or pulmonary edema are noted
- Descend if symptoms worsen or do not resolve in 1-2 days
- Supportive care
- Hydration
- NSAIDs for headaches
- Antiemetics for nausea/vomiting
- Medications
- Dexamethasone 4mg q6h for moderate to severe symptoms
- Consider acetazolamide 125mg BID (Luks 2014)
High-altitude cerebral edema (HACE)
- Clinical progression of acute mountain sickness
- Includes cerebral hypoxia causing increased cerebral blood flow leading to potentially life-threatening cerebral vasogenic edema with microhemorrhages
- Presentation
- Commonly occurs 2-4 days after arriving to altitudes >2500 meters
- Headache, nausea and vomiting are common but not obligatory
- Continuum from truncal ataxia, altered mental status, low-grade fever, coma, herniation to death
- Treatment
- Priority #1: Immediate Descent
- Supplemental O2 as needed
- Medications
- Dexamethasone 8mg once, then 4mg q6h until resolution of symptoms
- Consider acetazolamide 125mg BID (Luks 2014)
- Always consider alternative diagnosis, i.e. infections, strokes, subarachnoid hemorrhage
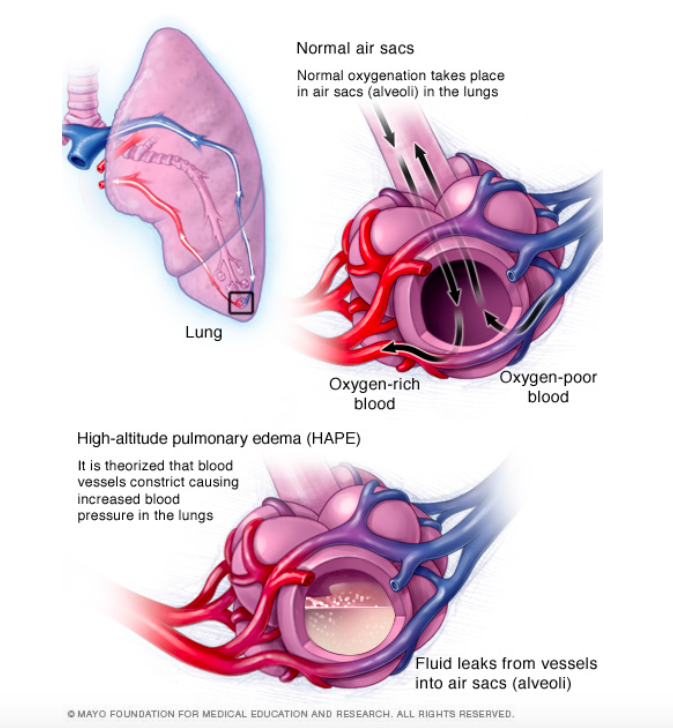
HAPE (Mayo Clinic)
High-altitude pulmonary edema (HAPE)
- Non-cardiogenic, hydrostatic pulmonary edema cause by hypoxic-induced vasoconstriction leading to high microvascular pressures (i.e. altitude-dependent pulmonary hypertension)]
- 50% fatal if untreated
- Presentation
- Initial symptoms: dry cough, decreased exercise tolerance, dyspnea on exertion and increased recovery time
- KEY TO DIAGNOSIS IS SUSPECTING IT
- Progresses to tachycardia, tachypnea, dyspnea at rest, weakness, productive cough, cyanosis, generalized rales; late findings include hypoxia, altered mental status, coma, death
- Low resting O2 saturation for given altitude and marked drop with exertion
- Usually presents 2-4 days at altitude >2500 meters
- Can occur independently of other symptoms of AMS or HACE
- In mild HAPE, 30% of patients will not have rales at rest but can be induced with exercise
- Diagnostics
- EKG may show right-axis deviation
- CXR findings vary from interstitial to localized alveolar to diffuse alveolar infiltrates depending on disease severity
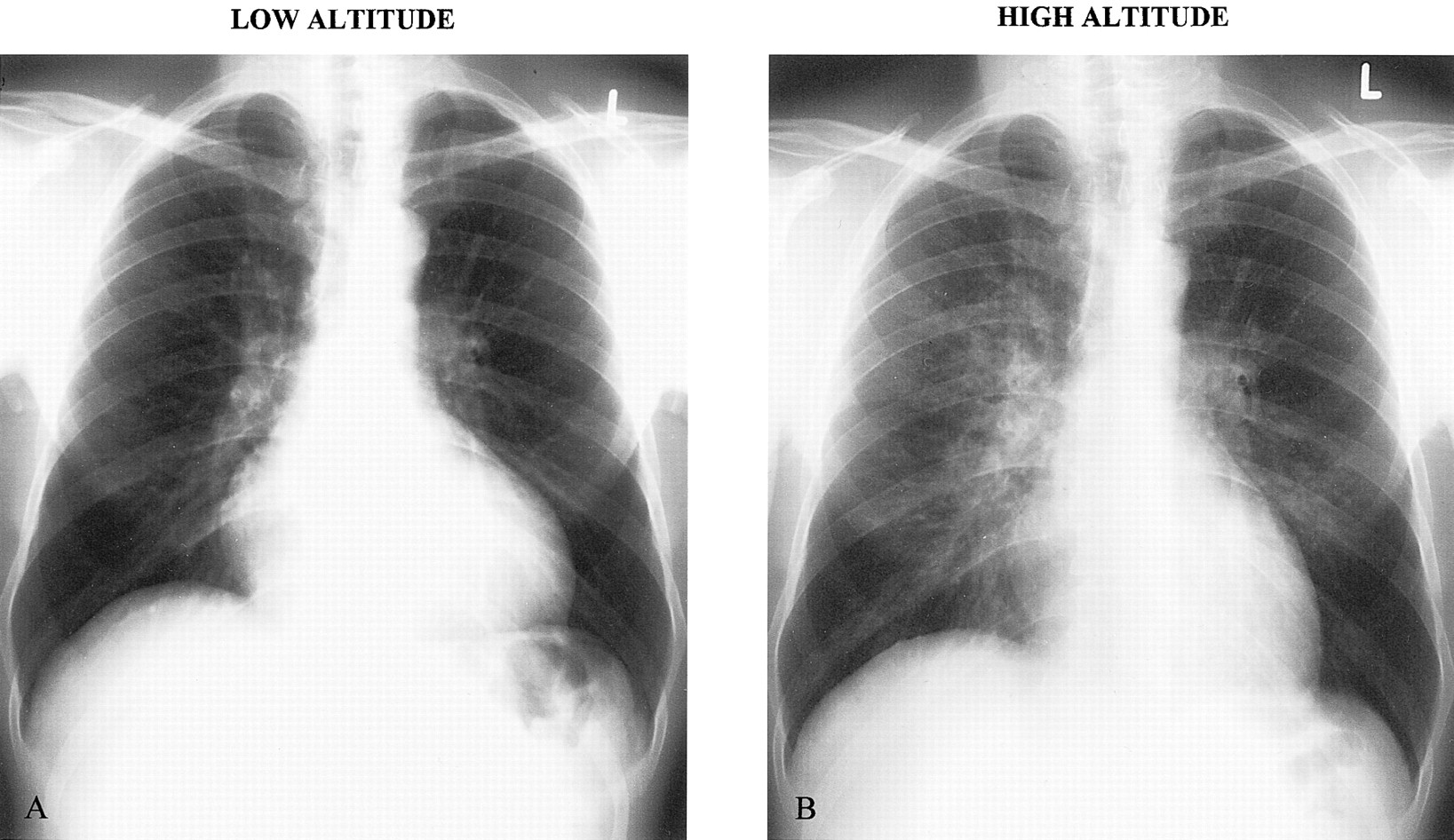
HAPE (Circulation)
- Treatment
- Immediate descent while minimizing exertion.
- Consider hyperbaric tents if unable to descend
- O2 supplementation to SpO2 >90% to decrease hypoxia-induces pulmonary artery vasoconstriction
- Keep warm as hypothermia exacerbates pulmonary arterial pressures
- Medications
- Nifedipinee 30mg extended-release BID reduces pulmonary artery pressures
- Phosphodiesterase-5 inhibitors used for prophylaxis and possible treatments as shown to blunt hypoxic pulmonary vasoconstriction (Bartsch 2013)
- Inhaled salmeterol can be used for prophylaxis
- No known utility for steroids or diuretics
Take Home Points
- Headache at altitude is concerning for AMS and can progress to HACE
- Suspecting HAPE is the key to diagnosing HAPE. Look for inappropriate dyspnea at rest or with exertions, lower resting oxygen saturations compared with peers
- Descent is the most important treatment for AMS, HACE, and HAPE
Read More:
Life in the Fast Lane: High Altitude Illness
References
Bartsch P, Swenson E. Acute High-Altitude Illnesses. NEJM 2013;368 (24): 2294-2302. PMID: 23758234
Hacket P, Hargrove J. High-Altitude Medical Problems in Tintinalli JE, Stapczynski JS, Ma OJ, Cline DM, Cydulka RK, Meckler GD, et al (eds): Tintinalli’s Emergency Medicine: A Comprehensive Guide, ed 7. McGraw Hill Companies, Inc., 2011, (Ch) 216: p 1403-1410.
Luks A et. al. Wilderness Medical Society practice guidelines for the prevention and treatment of acute altitude illness: 2014 update. Wilderness and Environ Med 2014; 25:S4-S14. PMID: 25498261.