ACNES Anatomy (www.aerzteblatt.de)
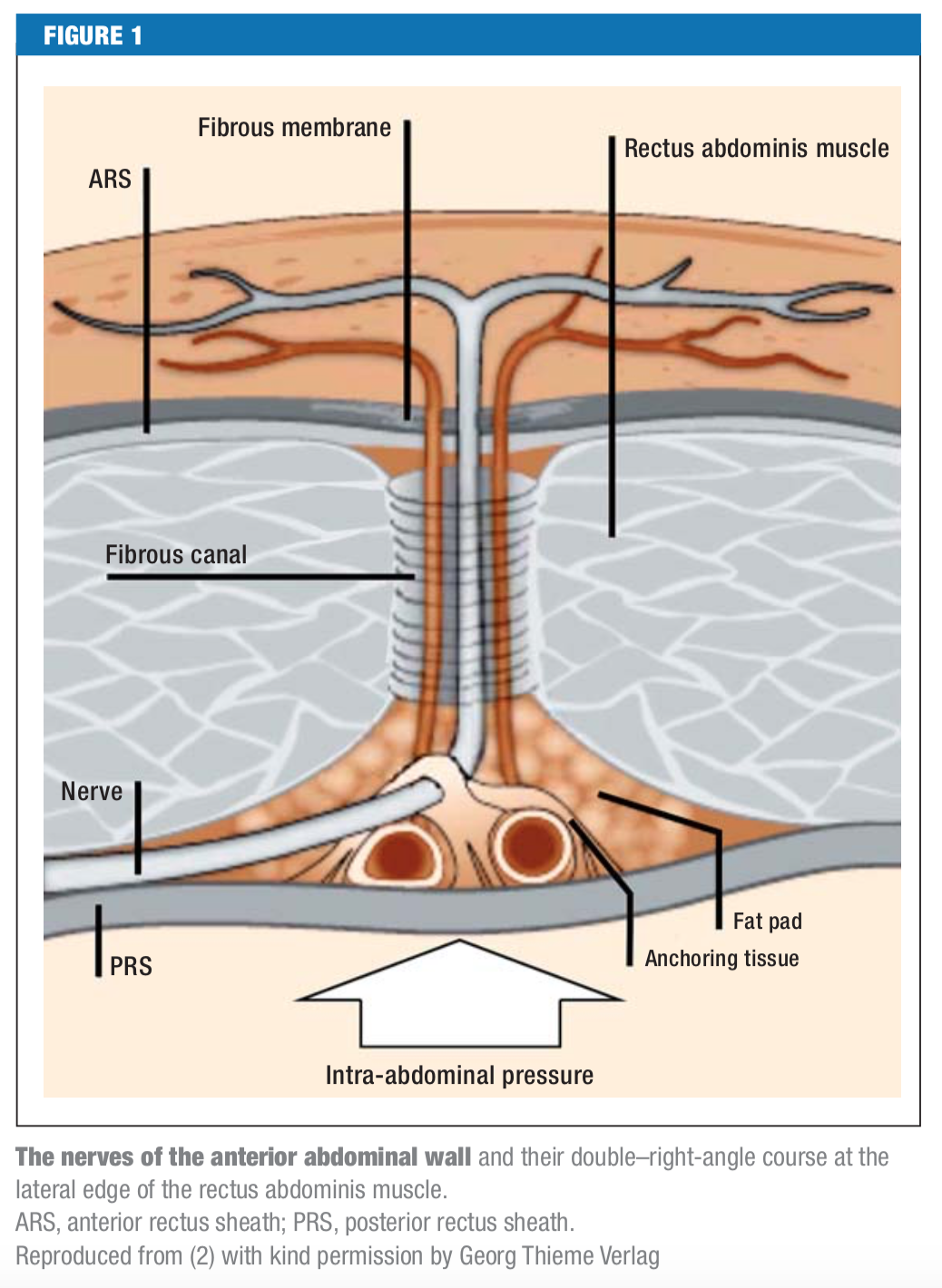
Definition: Abdominal cutaneous nerve entrapment syndrome (ACNES) is an under recognized cause of chronic abdominal pain. It results when the cutaneous branches of the lower intercostal nerves become entrapped in the lateral border of the rectus muscle.
Epidemiology
- Estimated incidence: 1 in 1800 (van Assen 2015)
- Reported in 2% of patients presenting to ED with abdominal pain (van Assen 2015)
- Up to 30% incidence in patients with chronic abdominal pain and negative prior work up (Koop 2016)
- Peak incidence between ages 30-50, but reported in 1 in 8 pediatric outpatients with chronic abdominal pain (Siawash 2016)
Pathogenesis
- Cutaneous branches of sensory nerves from T7 to T12 supply abdominal wall
- Branches make 90 degree angle as they traverse the abdominal wall at side of rectus sheath
- Nerves are vulnerable to compression at this site
- Entrapment can be caused by increased abdominal pressure, ischemia, herniation of fat, or scarring in the area
- Obesity, pregnancy, and oral contraceptive use identified as risk factors (Mishriki 2009, Peleg 1997, 1999)
Presentation
- Patients often complain of chronic abdominal pain localized to a small (<2cm) area
- Pain is usually located along the lateral edge of the rectus abdominis muscles and is often right sided, but can be in multiple locations and more diffuse with radiation in the area of the affected dermatome
- May be sharp, dull, or burning
- Exacerbated by tensing of the abdominal musculature (straining, sneezing, etc.) and is usually positional
Diagnosis
- Carnett’s Test
- Once pain is localized to specific area, the examiner presses on the point of maximal pain
- Patient is asked to tense the abdominal wall either by performing a sit-up or raising the legs
- Test is positive if pain increases or remains the same
- If pain decreases, suspect a visceral origin of pain
- Test characteristics (Srinivasan 2002)
- 78% sensitive
- 88% specific
- (+) Likelihood ratio: 6.5
- (-) Likelihood ratio: 0.25
- Proposed diagnostic criteria
- Test characteristics (Srinivasan 2002)
- 85% sensitive
- 97% specific
- (+) Likelihood ratio: 28.3
- (-) Likelihood ratio: 0.15
- Test characteristics (Srinivasan 2002)
| Very localized pain
(Can be covered by fingertip) |
AND | Superficial tenderness
(depth of rectus abdominis) |
| OR | ||
| OR | Point tenderness ≤2.5 cm in diameter | |
| Fixed location of tenderness | OR | |
| Positive Carnett test |
- >50% pain relief with injection of local anesthetic considered diagnostic and has been shown to be effective when compared to placebo injection (Boelens 2013)
Treatment
- Systemic analgesia with NSAIDs, opioids, and neuropathic pain agents (gabapentin, etc) have unclear efficacy (Chrona 2017)
- Combination injection with local anesthetic and corticosteroid is generally first line therapy (Koop 2016)
- Immediate relief of symptoms in 83-91% of patients with injection of anesthetic alone, though prolonged relief only in 20%
- Multiple injections lead to prolonged relief in 40-50% of patients and the addition of corticosteroids up to 80%
- Injection of 1-3mL of 1% lidocaine or 0.25-0.5% bupivacaine with 40mg of long acting steroid (like triamcinolone) at the point of maximal tenderness is typical therapy
- Although injections were historically performed with anatomical landmarks, ultrasound is becoming standard for identification localization of injection site and affected nerve
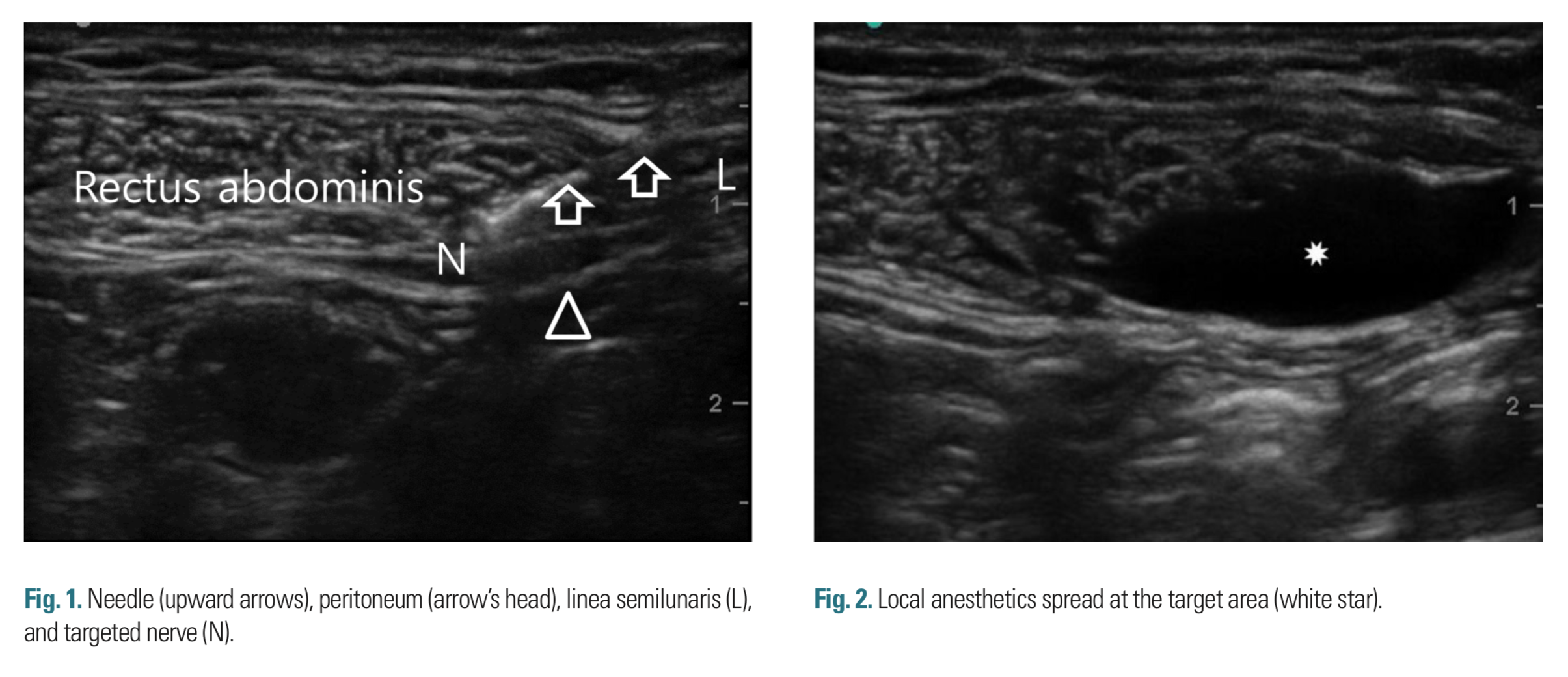
Ultrasound Guided Nerve Block (Lee 2016)
Take Home Points
- ACNES is an under recognized cause of chronic abdominal pain in patients presenting to the ED
- Consider in patients with localized, positional pain without symptoms suggestive of an intra-abdominal pathology
- Diagnosis is based on characteristic history and physical exam findings including positive Carnett’s test
- Trigger point injection with anesthetic and steroid can both confirm the diagnosis and provide symptomatic relief
References
Van assen T et al. Incidence of abdominal pain due to the anterior cutaneous nerve entrapment syndrome in an emergency department. Scand J Trauma Resusc Emerg Med. 2015;23:19. PMID: 25887961
Koop H et al. Chronic Abdominal Wall Pain. Dtsch Arztebl Int. 2016;113(4):51-7. PMID: 26883414
Siawash M et al. Prevalence of Anterior Cutaneous Nerve Entrapment Syndrome in a Pediatric Population With Chronic Abdominal Pain. J Pediatr Gastroenterol Nutr. 2016;62(3):399-402. PMID: 26327211
Mishriki YY. Abdominal wall pain in obese women: frequently missed and easily treated. BMJ Case Rep. 2009. PMID: 21686788
Peleg R et al. Abdominal wall pain in pregnant women caused by thoracic lateral cutaneous nerve entrapment. Eur J Obstet Gynecol Reprod Biol. 1997;74(2):169-71. PMID: 9306112
Peleg R. Abdominal wall pain caused by cutaneous nerve entrapment in an adolescent girl taking oral contraceptive pills. J Adolesc Health. 1999;24(1):45-7. PMID: 9890364
Srinivasan R, Greenbaum DS. Chronic abdominal wall pain: a frequently overlooked problem. Practical approach to diagnosis and management. Am J Gastroenterol. 2002;97(4):824-30. PMID: 12003414
Boelens OB et al. Randomized clinical trial of trigger point infiltration with lidocaine to diagnose anterior cutaneous nerve entrapment syndrome. Br J Surg. 2013;100(2):217-21. PMID: 23180371
Chrona E et al. Anterior cutaneous nerve entrapment syndrome: management challenges. J Pain Res. 2017;10:145-156. PMID: 28144159
Lee M, et al. Diagnosis and Treatment of Abdominal Cutaneous Nerve Entrapment Syndrome Using Ultrasonography. Soonchunhyang Medical Science. 2016;22(2):147-150. doi:10.15746/sms/16/034
