Background
- Abdominal aortic aneurysms are typically asymptomatic and will progressively expand until they rupture. Ruptured aortic aneurysms have a mortality rate of 85-90% (Kent 2014).
- Prevalence rates are estimated to be 1.3-8.9% in men and 1.0-2.2% in women with main risk factors of smoking, age, family history, and hypertension (Sakalihasan 2005).
Indications
- In the primary care setting, the US Preventive Services Task Force recommends screening for abdominal aortic aneurysms (AAA) in men 65-75 years old who have ever smoked (grade B).
- In the ED, AAA should be on the differential in the setting of pain, hypotension and a pulsatile mass. AAA should also be considered in at-risk patients who present with syncope or signs of retroperitoneal hemorrhage.
- Emergency ultrasound of the abdominal aorta by emergency medicine physicians has been shown to be sensitive and specific. One prospective study in 2008 found bedside ultrasound to be 100% sensitive and 98% specific in detecting a AAA (Tayal 2008).
Technique
- The low-frequency, 3.5 MHz curvilinear probe is typically used for imaging of the aorta (Dean 2008).
- Beginning in the epigastric area, with the probe in the transverse plane, identify the vertebral body. The aorta should be visualized above the vertebral body on patient’s left.
- Short axis images should be obtained of the patient’s proximal abdominal aorta as well as the distal abdominal aorta, just above the site of the bifurcation into the iliac arteries.
- A long axis view should be obtained with the probe in the sagittal plane.
- A short axis view of the iliacs should be obtained distal to the bifurcation.
- Use the measurement calipers to measure the anterior-to-posterior diameter of the abdominal aorta using the outer walls.
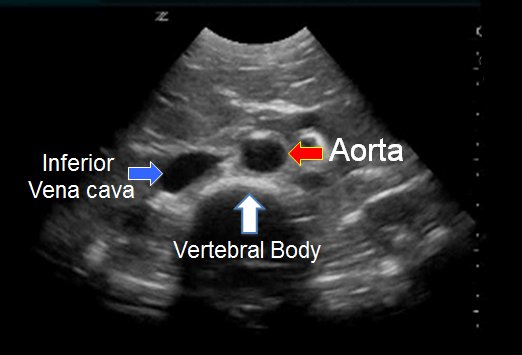
Short axis. “Ultrasound Assessment of Abdominal Aortic Aneurysms.” Medscape, reference.medscape.com/features/slideshow/ultrasound.

Long axis. “POCUS Exams – Aorta.” Ultrasound Idiots, www.ultrasoundidiots.com/aorta.
Aortic Bifurcation
Iliac Bifurcation
Evaluation
- An abdominal aortic aneurysm is diagnosed when the diameter is greater than 3.0 cm.
- The aorta should taper as the vessel is traced distally. An aorta that dilates should prompt further evaluation, even if the measurements remain within normal limits.
- Complete evaluation should trace past the bifurcation and include measurements of the common iliac vessels. These should measure <1.5 cm in women and <1.8 cm in adult men.
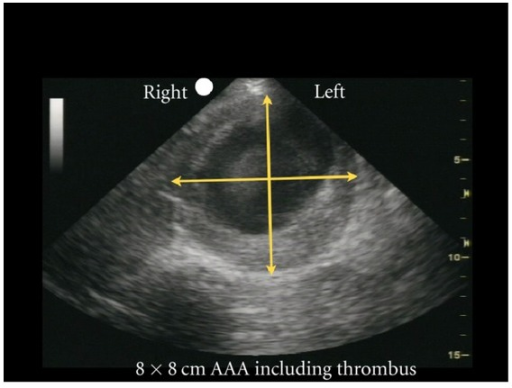
8x8cm AAA including thrombus. Bookatz, Allen, et al. “Aortic Ultrasound.” WikEM, 30 Dec. 2017, wikem.org/wiki/Aortic_ultrasound.
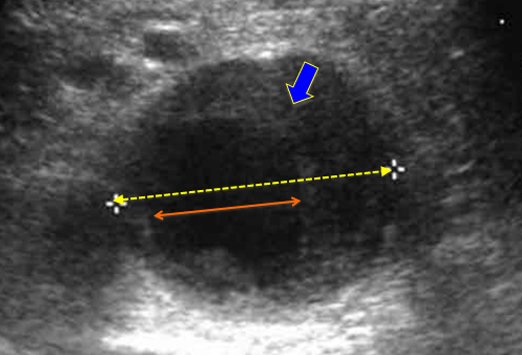
Measure from outer edge to outer edge. “Ultrasound Assessment of Abdominal Aortic Aneurysms.” Medscape, reference.medscape.com/features/slideshow/ultrasound.
Common Pitfalls
- Bowel gas will occasionally obscure the image. If this occurs, place additional pressure on the probe and gently fan up and down in an attempt to displace the bowel gas.
- Accurate measurements require measurement from the outer wall to the outer wall. Take care not to confuse the inner edge of a thrombus with the outer wall of the abdominal aorta.
- Be sure to not confuse the IVC with the abdominal aorta. The IVC is on the patient’s right and is typically non-pulsatile and compressible. Additionally, doppler mode can help to identify pulsatile waveforms consistent with aortic blood flow.
Take Home Points
- Consider AAA in setting of pain, hypotension, pulsatile mass, or syncope, especially in older men with a smoking history
- AAA is diagnosed when the outer wall to outer wall measurement exceeds 3.0 cm. Be careful not to mistake the inner rim of a thrombus for the outer wall of the abdominal aorta.
- Take the time necessary to differentiate the abdominal aorta from the IVC. If bowel gas is obscuring the image, apply increased pressure and slowly fan up and down.
References
- Abdominal aortic aneurysm. (2019, September 23). Retrieved from https://wikem.org/wiki/Abdominal_aortic_aneurysm.
- Dean, A. J., & Ku, B. S. (2008). Sonoguide: Abdominal Aortic Aneurysms. Retrieved from https://www.acep.org/sonoguide/abdominal_aortic_aneurysm.html.
- Final Update Summary: Abdominal Aortic Aneurysm: Screening – US Preventive Services Task Force. (2014, June). Retrieved from https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/abdominal-aortic-aneurysm-screening.
- Kent, K. C. (2014). Abdominal Aortic Aneurysms. New England Journal of Medicine, 371(22), 2101–2108. doi: 10.1056/nejmcp1401430
- Medscape: Abdominal aortic aneurysm ultrasound slideshow. (n.d.). Retrieved from https://reference.medscape.com/features/slideshow/ultrasound.
- Sakalihasan, N., Limet, R., & Defawe, O. (2005). Abdominal aortic aneurysm. The Lancet, 365(9470), 1577–1589. doi: 10.1016/s0140-6736(05)66459-8
- Tayal, V. S. (2003). Prospective Study of Accuracy and Outcome of Emergency Ultrasound for Abdominal Aortic Aneurysm over Two Years. Academic Emergency Medicine, 10(8), 867–871. doi: 10.1197/aemj.10.8.867
- Title Image from: https://ccc.maricopaemergencymedicine.com/abdominal-aortic-aneurism/