Background
The diagnosis of a pulmonary embolism (PE) in the Emergency Department (ED) is complicated. Many different decision rules have been developed to help risk stratify patients coming into the ED with some level of suspicion for PE. The Pulmonary Embolism Rule-Out Criteria (PERC) are a set of decision rules created to reduce testing in patients who have a low probability of PE. For low-risk patients in whom the diagnosis of PE is being considered, a negative PERC criteria (for all features) results in a patient who is risk stratified to a low enough level (< 2%) that further testing is unlikely to yield benefit to the patient. While multiple observational studies have looked at the validity of the PERC criteria, before now, no prospective randomized clinical trials have existed.
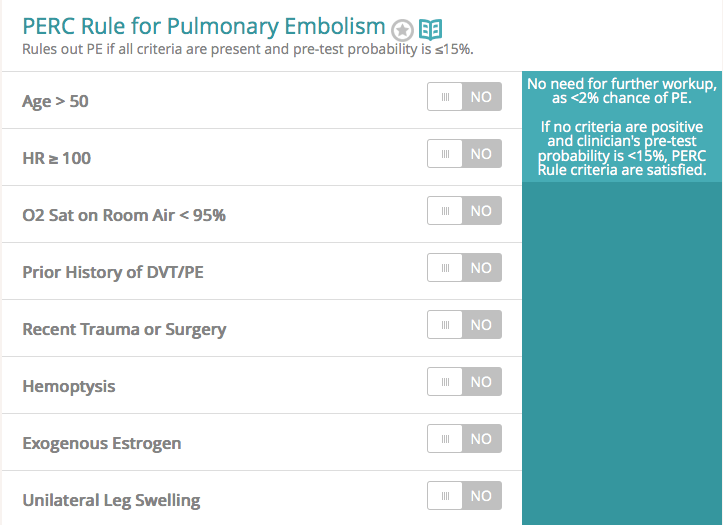
PERC Criteria – MDCalc
Clinical Question
Is using PERC in patients with a “low risk” of PE non-inferior to conventional care and testing in diagnosing clinically significant PE?
Population
Patients with suspicion of pulmonary embolism but who were determined to be low-risk (<15%) by physician gestalt in 14 emergency departments in France from August 2015 to September 2016
Intervention
PERC = 0, no further testing; PERC > 0, age adjusted D-dimer and if positive CT pulmonary angiography
Control
Age adjusted D-dimer, and if positive, CT pulmonary angiography
Outcomes
Primary: Occurrence of a thromboembolic event during the 3-month follow-up period that was not diagnosed at initial visit
Secondary:
Rate of CT pulmonary angiography
Rate of CTPA-related adverse events requiring intervention within 24 hours
Median length of stay
Rate of hospital admission
Onset of anticoagulation therapy
Severe hemorrhage in patients on anticoagulation therapy
All cause mortality at 3 months
Design
Prospective, crossover cluster-randomized clinical noninferiority trial
Excluded
Obvious cause of symptoms other than PE (ex: PTX), critical presentation (hypotension, hypoxia < 90%), contraindication to CTPA, pregnancy, inability to be followed up, already on anticoagulant
Primary Results
- 1916 patients initially included
- 962 patients in PERC group
- 954 patients in control group
- 1749 patients completed trial
Critical Findings (95% CI)
- 1 patient was diagnosed with VTE in follow-up in the PERC group (0.1%) compared with 0 in the control
- Primary Outcome: PERC was non-inferior to standard care for the occurrence of VTE at 3-month follow up
- 10% decrease in patients undergoing CT in PERC cohort
- 36 minute mean reduction in ED stay
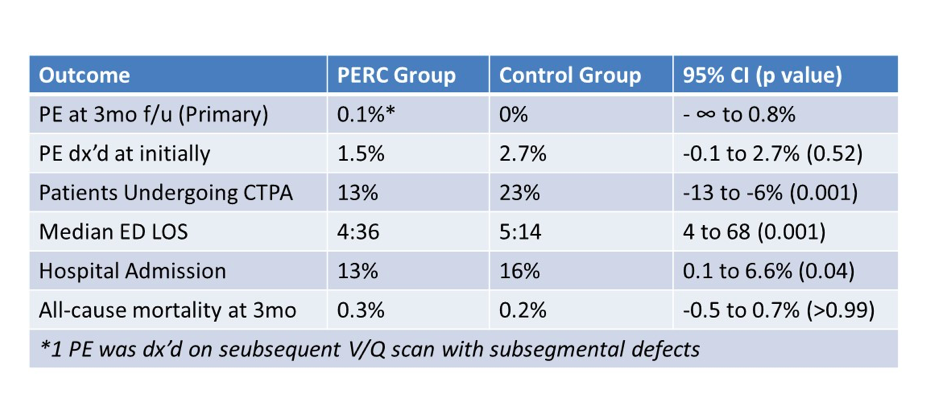
PERC RCT Outcomes (Freund 2018)
Strengths
- Multicenter, randomized, prospective clinical trial
- Robust follow up methods
- Patients instructed to return to same ED if they experienced new/worsening symptoms
- GPs contacted if unable to contact patient
- Confirmation of PE and death due to PE was performed by blinded experts
Limitations
- Prevalence of PE still extremely low (2.3% upon initial visit)
- 54 patients lost to follow up
- Per-protocol analysis and not intention to treat
- Mean age young compared with other trials (44 years)
- Subsegmental PE’s still considered positive although these may not be clinically important
Other Issues
- Study incidentally showed the overestimation of PE risk by provider
- Category of control group should have included only patients with PE prevalence below 15%
- Prevalence of PE in control group only 2.7%
- Significant percent of patients with positive dimer never received definitive imaging
- 62% of patients PERC group
- 54% of pts in control group
Author's Conclusions
“Among very low risk patients with suspected PE, randomization to a PERC strategy vs conventional strategy did not result in an inferior rate of thromboembolic events over 3 months. These findings support the safety of PERC for very-low risk patients presenting to the emergency department.”
Our Conclusions
We agree with the authors. A PERC-based algorithm is safe to use in the ED in very low risk patients. This strategy will reduce imaging in comparison to standard practice.
Potential Impact To Current Practice
Based on this study, PERC can be continued to be used safely in the ED in low risk patients with suspicion for PE
Bottom Line
A PERC-based strategy is non-inferior to usual care in the ED. PERC should ONLY be applied in very low risk patients. Using PERC may lead to a decrease in imaging and LOS
Read More
MD Calc: PERC Criteria
REBEL EM: Is It PROPER to PERC It Up?
EM Lit of Note: Using PERC & Sending Home Pulmonary Emboli For Fun and Profit