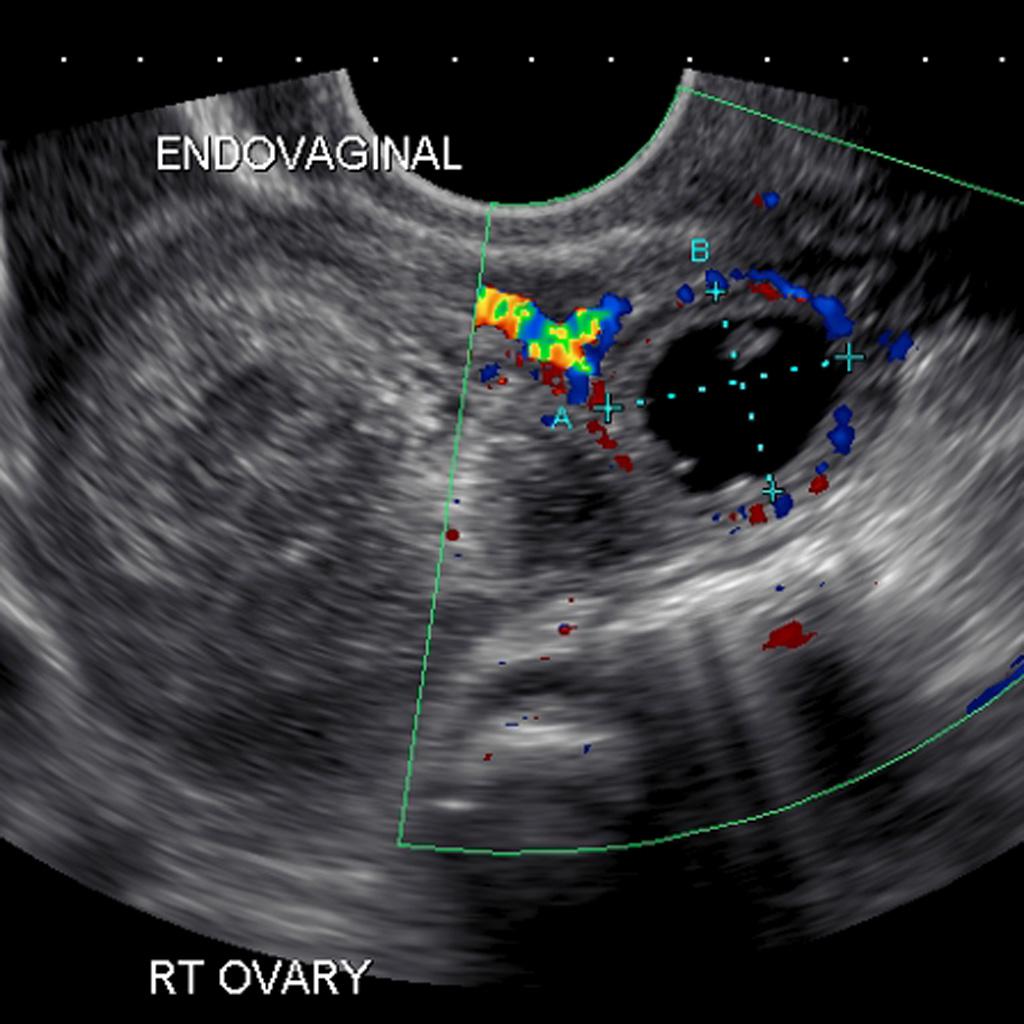
Ectopic Pregnancy on US (Case courtesy of A.Prof Frank Gaillard, Radiopaedia.org. From the case rID: 8161)
Definition: Embryo implantation outside of the endometrial cavity
Background: (Alkatout 2013)
- Ectopic pregnancy occurs in up to 2% of pregnancies.
- It is the leading cause of 1st trimester death and causes 0.5 deaths/100,000 live births.
- Ectopic Location (Arleo 2014)
- Greater than 95% of extrauterine implantations occur in the fallopian tube.
- Interstitial pregnancies: occur in to the most proximal segment of the fallopian tube within the uterine wall
- Cornual pregnancies occur in the upper and lateral portion of the uterus.
- Rare cervical pregnancies implant in the uterine endocervix. They may be confused with an aborting intrauterine pregnancy (IUP) residing in the cervix and may lead to massive hemorrhage if disturbed.
- Heterotopic pregnancy: An ectopic pregnancy in conjunction with an IUP
- Natural conception rate: 1/30,000
- Assisted reproduction rate: 1/100
- Ectopic pregnancy rupture is often associated with profound hemorrhage, which may be fatal if rapid surgical intervention isn’t undertaken
- The vast majority of deaths occur prior to hospitalization or just after to arrival to the emergency department. (Anderson 2004)
Clinical Presentation:
- Classic Triad
- Abdominal pain
- Vaginal bleeding
- Missed menstrual period
- Patient’s typically present 6-8 weeks after the last normal menstrual period
- Signs and symptoms suggestive of rupture
- Vital sign abnormalities
- Hypotension
- Tachycardia
- Shock
- Lightheadedness/syncope
- Cool, pale skin
- Nausea + emesis
- Severe abdominal pain
- Vital sign abnormalities
- Referred pain
- Diaphragmatic irritation from free blood in the peritoneal space may present as shoulder pain
- Referred neck or rectal pain are reported
- Vagal stimulation from intra-peritoneal blood can present as hypotension and bradycardia
Selected Differential Considerations:
- OB/GYN conditions: Spontaneous abortion (of normal IUP), septic abortion, early normal IUP, ovarian cyst, ovarian/fallopian torsion, necrotic myoma, PID/TOA
- Others: Appendicitis, cystitis, obstructed viscus, perforated viscus, pyelonephritis, vascular hemorrhage/ischemia.
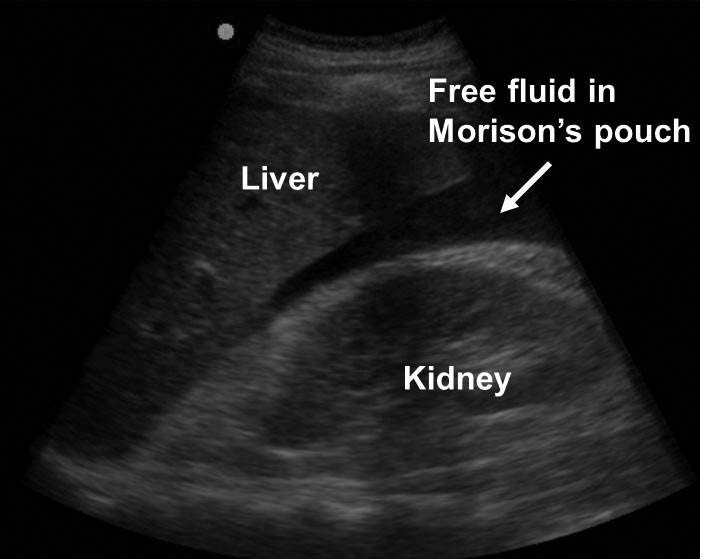
Free Fluid in Morrison’s Pouch (AHC Media)
Evaluation of Unstable Patients
- Rapid identification is paramount
- Ruptured ectopic should be considered in any hemodynamically unstable woman of child bearing age
- Presence of free fluid in absence of trauma in this group should be considered ectopic pregnancy until proven otherwise
- Basic Management
- ABCs, Large bore (> 18 gauge) IV X 2, Supplemental O2 if necessary
- Approach similar to exsanguinating trauma patient
- Key actions:
- Perform a FAST exam
- Positive result requires immediate OB/Gyn or surgical consultation for surgical exploration
- Can improve sensitivity by placing patient in Trendelenburg position
- Hemodynamic instability should trigger massive transfusion protocol
- Start resuscitation with O negative blood (start with crystalloid resuscitation if blood not immediately available)
- Perform a FAST exam
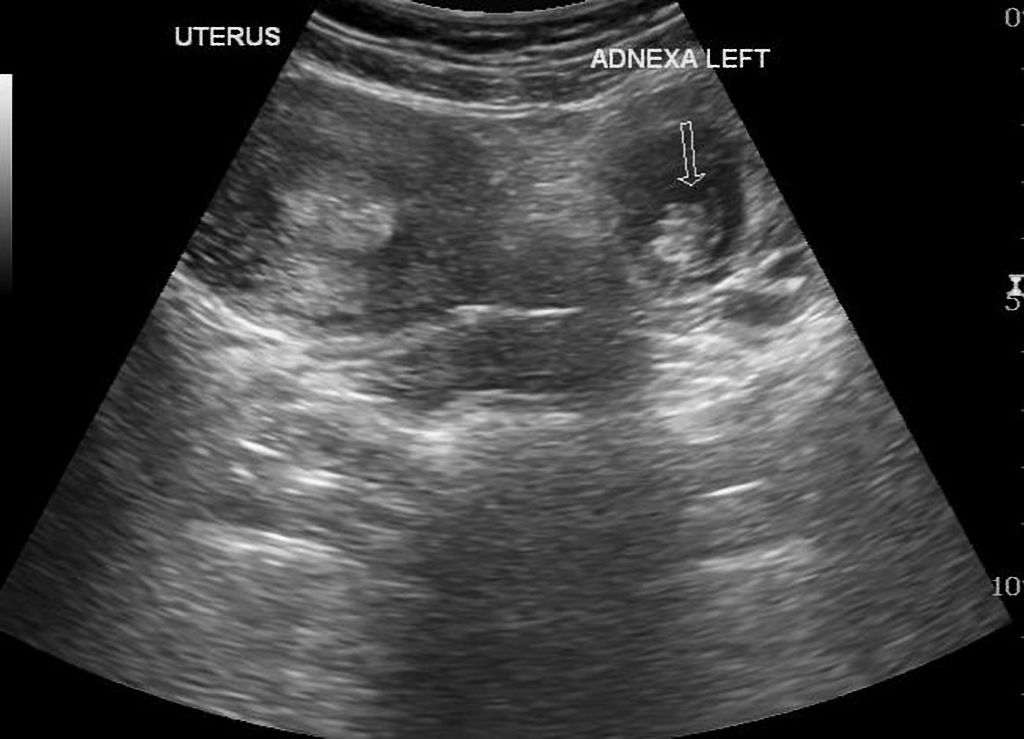
Ectopic Pregnancy US (Case courtesy of Dr Maulik S Patel, Radiopaedia.org. From the case rID: 46956)
Evaluation of Stable Patients
- Rapid, unexpected decompensation can occur
- Pertinent History/Risk Factors: prior genital tract infection(s), prior ectopic pregnancy, prior dilatation and curettage or tubal ligation, current IUD, assisted reproduction, age >35, tobacco use, progestin-only contraception
- Assessment
- Vital signs: may be normal early in the course of significant bleeding, particularly in young patients due to compensatory mechanisms
- Physical examination: lower abdominal tenderness or diffuse tenderness with or without rebound or guarding, depending on extent of hemorrhage
- FAST exam (for free fluid)
- Laboratory evaluation
- Quantitative pregnancy test
- CBC (to aid in assessment of blood loss)
- Basic metabolic panel (renal function important consideration in medical management)
- Type and screen (with Rh factor status)
- PT/PTT and fibrinogen in unstable patients (assessment for DIC)
- Imaging
- Transabdominal US can rapidly identify IUP but can miss early pregnancy
- Transvaginal US (TVUS) is more sensitive for diagnosing an IUP and for finding an ectopic
-
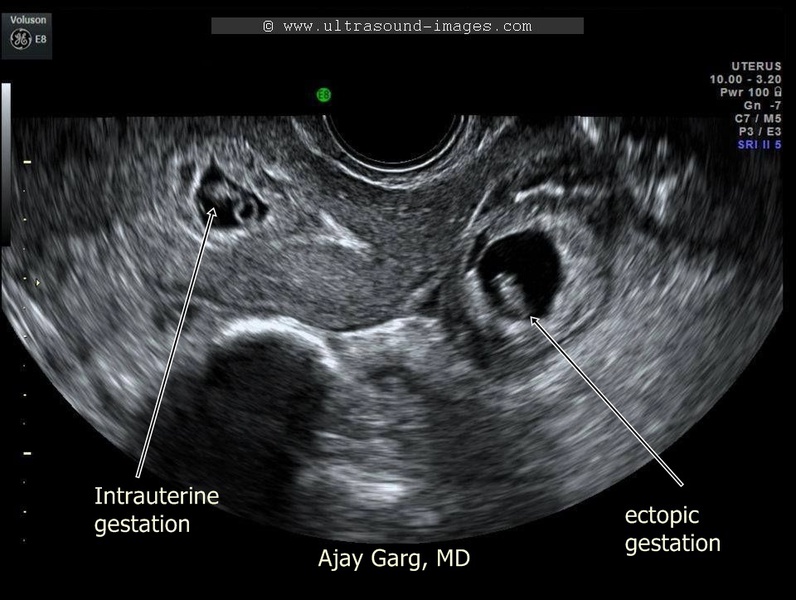
Heterotopic Pregnancy (Ultrasound Image Gallery)
Management based on imaging
- Ultrasound with (+) IUP
- Ectopic highly unlikely (possible in heterotopic)
- Manage as threatened Ab
- Consider hetertopic pregnancy in patients with assisted reproduction
- Ultrasound with (+) ectopic
- OB/Gyn consultation for further management
- Ultrasound with no IUP or ectopic (indeterminate US) AND no free fluid
- β-hCG level < 1500 (Condous 2005)
- May be early IUP
- Typically will get repeat β-hCG in 48 hours to look for appropriate rise and repeat US
- β-hCG level > 1500
- Risk of ectopic rises as TVUS usually locates IUP above this level
- Management will be based on shared decision making with patient and OB/Gyn
- Medical abortion (methotrexate)
- Expectant management (repeat US and β-hCG)
- β-hCG level < 1500 (Condous 2005)
- Ultrasound with (+) IUP
- Medical management with methotrexate
- Eligible Patients:
- Hemodynamically Stable,
- Hcg <5000,
- Need to comply with treatment and follow up,
- No fetal cardiac activity
- Contraindications:
- Renal insufficiency
- Immunodeficiency
- Active Pulmonary Disease
- Peptic Ulcer Disease
- Hypersenstivity to MTX
- Heterotopic Pregnancy with viable IUP
- Breastfeeding
- Dosing
- IM Therapy is most common choice (Linscomb 2007)
- Dose 50mg/m2 of body surface area (Stovall 1993)
- Disposition
- Patients with ectopic pregnancy may be discharged after administration of methotrexate
- Indeterminate US
- Hemodynamically stable patients may be discharged
- Close follow up is mandatory
- Eligible Patients:
Take Home Points
- Ecoptic pregnancy is the leading cause of 1st trimester maternal death
- Always consider the diagnosis of an ectopic pregnancy in any woman of child bearing age presenting with abdominal pain, vaginal bleeding, and missed period
- Hemodynamically unstable patients need rapid diagnosis and stabilizing treatment
- Involve consulting services early on in management course
Read More:
LITFL: Ectopic Pregnancy
EM Updates: Rule Out Ectopic in the Emergency Department
EM: RAP: Episode 79 – Ectopic Pregnancy
EM: RAP: C3- Frist Trimester Vaginal Bleeding
References:
ACEP Clinical Policies Subcommittee (Writing Committee) on Early Pregnancy et al. Clinical Policy: Critical Issues in the Initial Evaluation and Management of Patients Presenting to the Emergency Department in Early Pregnancy. Ann Emerg Med. 2017;69:241-250.e20. PMID: 22921048
Alkatout I et al. Clinical diagnosis and treatment of ectopic pregnancy. Obstet Gynecol Surv 2013;68:571. PMID: 23921671
American Institute of Ultrasound in Medicine, ACEP. AIUM practice guideline for the performance of the focused assessment with sonography for trauma (FAST) examination. J Ultrasound Med 2014;33:2047. PMID: 18204028
Anderson FW et al. Sudden death: ectopic pregnancy mortality. Obstet Gynecol 2004;103:1218. PMID: 15172855
Arleo EK, DeFilippis EM. Cornual, Interstitial, and Angular Pregnancies: Clarifying the Terms and a Review of the Literature. Clin Imaging. 2014;38:763-70. PMID: 25156020
Barnhart KT. Clinical practice. Ectopic pregnancy. N Engl J Med. 2009;361:379-387. PMID: 19625718
Condous G, Kirk E, Lu C, et al. Diagnostic accuracy of varying discriminatory zones for the prediction of ectopic pregnancy in women with a pregnancy of unknown location. Ultrasound Obstet Gynecol 2005; 26:770. PMID: 16308901
Doubilet PM et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013;369:1443-1451. PMID: 24106937
Ley EJ et al. Emergency department crystalloid resuscitation of 1.5 L or more is associated with increased mortality in elderly and nonelderly trauma patients. J Trauma 2011;70:398. PMID: 21307740
Lipscomb GH. Medical therapy for ectopic pregnancy. Semin Reprod Med 2007; 25:93. PMID: 17377896
Parks JK et al. Systemic hypotension is a late marker of shock after trauma: a validation study of ATLS principles in a large national sample. Am J Surg 2006; 192:727. PMID: 17161083
Rana P et al. Ectopic pregnancy: a review. Arch Gynecol Obstet. 2013;288:747-57. PMID: 23793551
Samal SK, Rathod S. Cervical ectopic pregnancy. J Nat Sci Biol Med. 2015;6:257-60.PMID: 25810679
Stovall TG, Ling FW. Single-dose methotrexate: an expanded clinical trial. Am J Obstet Gynecol 1993; 168:1759. PMID: 8317518