Definition: Refractory Ventricular Arrhythmias
-
Persistent ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT) despite ≥3 shocks, appropriate CPR, vasopressors, and anti-arrhythmics.
Epidemiology
-
Refractory VF occurs in roughly 10–25% of out-of-hospital cardiac arrest (OHCA) cases.
-
Linked with extremely poor outcomes: survival to discharge ~2–12%.
-
Increasing use of mechanical CPR and ECMO has driven interest in novel defibrillation strategies.
Background: Standard Defibrillation (Based on ACLS Guidelines)
-
Indication:
-
Primary intervention for pulseless VT/VF, the most common initial rhythm in witnessed cardiac arrest.
-
-
Pad Placement:
-
Standard pad positioning is anterior-lateral (AL):
-
One pad below the right clavicle (sternal region)
-
One pad lateral to the left nipple (apical position)
-
-
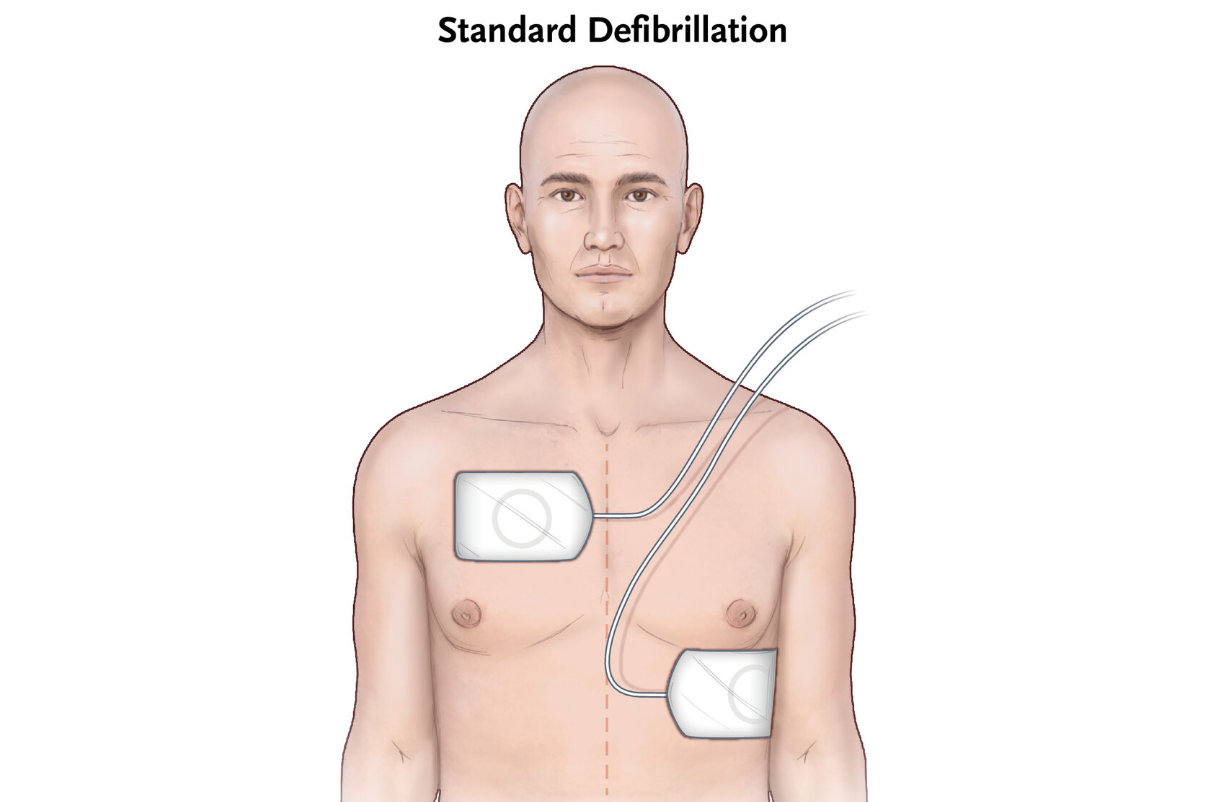
Figure 1: Cheskes S, Verbeek PR, Drennan IR, et al. Defibrillation strategies for refractory ventricular fibrillation. N Engl J Med. 2022;387(21):1947–1956. doi:10.1056/NEJMoa2207304
-
Shock Type:
-
Unsynchronized for pulseless VF/VT
-
Synchronized for unstable monomorphic VT with a pulse
-
-
Energy Recommendations:
-
Biphasic: 120–200 J (varies by device manufacturer)
-
Monophasic: Fixed at 360 J
-
-
Shock Protocol:
-
Deliver shock immediately after rhythm analysis confirms VF/VT.
-
Resume high-quality CPR immediately post-shock.
-
Administer epinephrine every 3–5 minutes.
-
Introduce antiarrhythmic drugs (e.g., amiodarone, lidocaine) after the third shock.
-
Alternative Defibrillation Strategies
-
Vector Change (VC) Defibrillation:
-
A single defibrillator is used.
-
Pads repositioned from AL to AP to change the shock vector.
-
Theoretically re-engages different myocardial fibers or improves current delivery.
-
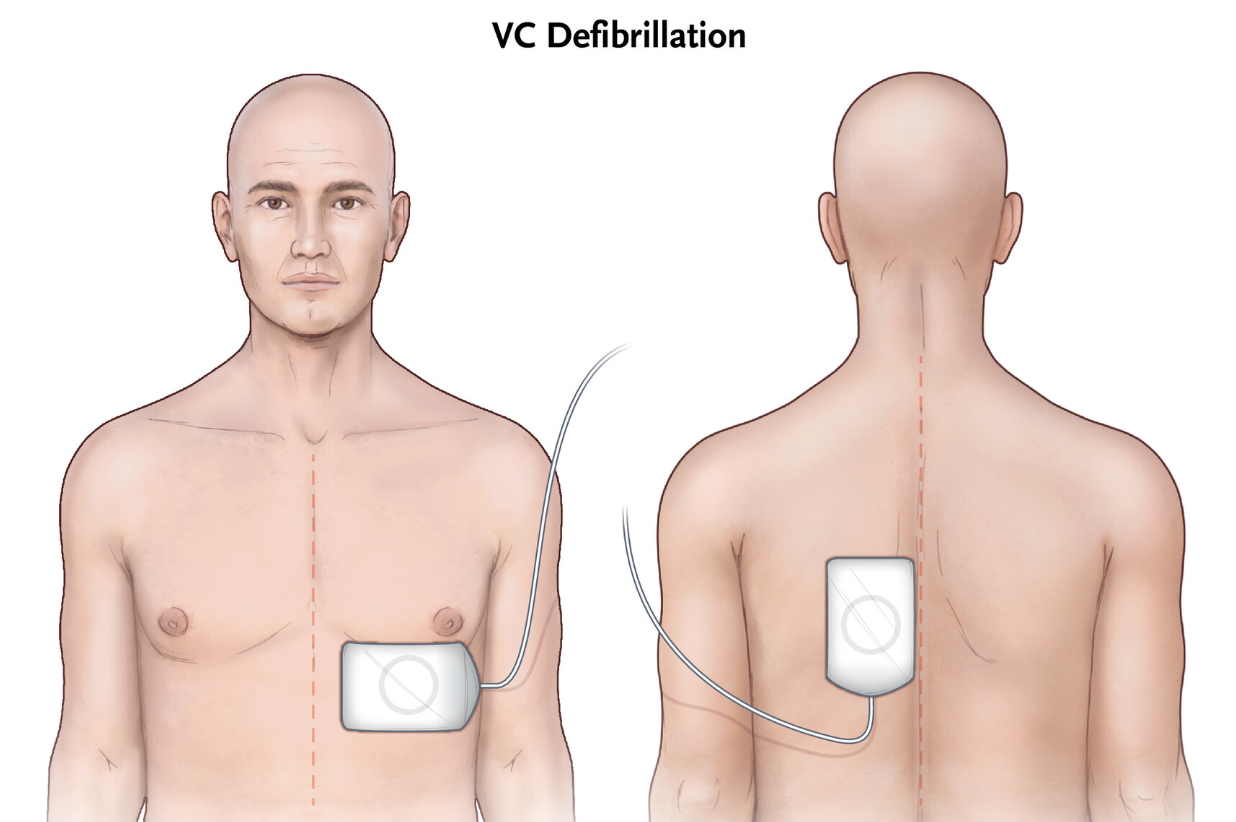
Figure 1: Cheskes S, Verbeek PR, Drennan IR, et al. Defibrillation strategies for refractory ventricular fibrillation. N Engl J Med. 2022;387(21):1947–1956. doi:10.1056/NEJMoa2207304
-
Dual Sequential External Defibrillation (DSED):
-
Uses two defibrillators delivering sequential high-energy shocks.
-
Pads placed in both AL and anterior-posterior (AP) positions.
-
Goal: Engage multiple vectors and potentially overcome high defibrillation thresholds.
-
-
Dual Dose Defibrillation:
-
Two defibrillators deliver simultaneous shocks.
-
Controversial due to concerns of myocardial injury; less commonly practiced.
-
History of Dual Sequential Defibrillation
-
DSED emerged in case reports from the 1990s; gained popularity through anecdotal success and observational data.
-
First large-scale RCT (DOSE-VF) published in NEJM 2022.
Pathophysiology: How DSED Might Work
-
Power Hypothesis:
-
Two sequential shocks may summate energy, reaching thresholds unreached by single shocks.
-
-
Priming Theory:
-
First shock may lower myocardial resistance, allowing the second to more effectively depolarize myocardium.
-
-
Multi-Vector Theory:
-
Dual pad positions apply energy through different planes, increasing the chance of disrupting reentrant circuits in VF.
-
-
Improved Myocardial Engagement:
-
Engages more myocardial mass and potentially overcomes anisotropy (directional resistance) in damaged cardiac tissue.
-
Methodology: How to Perform Dual Sequential Defibrillation
-
Team Coordination Is Key:
-
Two defibrillators, two sets of pads, and a coordinated team approach are required.
-
-
Pad Placement:
-
Defibrillator A (Standard): AL position
-
Defibrillator B (Alternate): AP position (posterior pad placed beneath scapula)
-
- It is essential that pads are not touching otherwise you risk damaging both defibrillators.
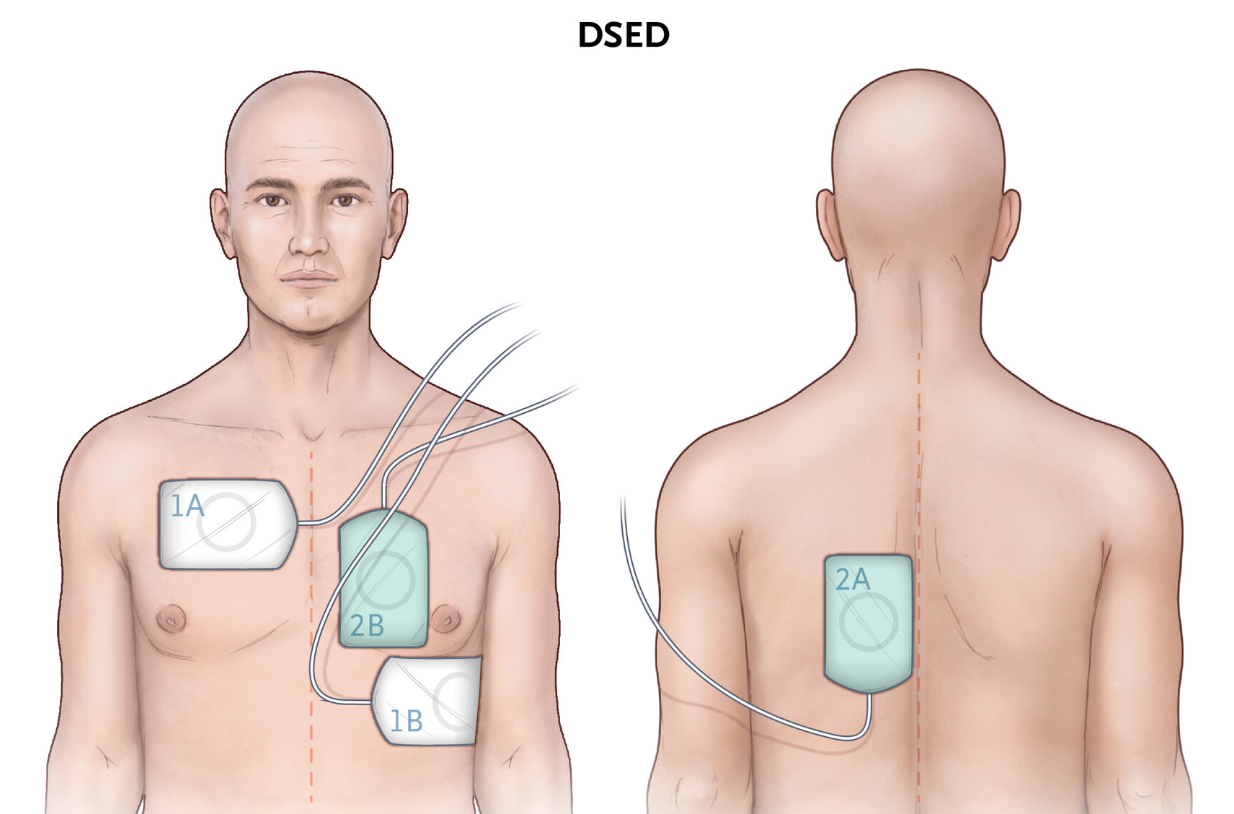
Figure 1: Cheskes S, Verbeek PR, Drennan IR, et al. Defibrillation strategies for refractory ventricular fibrillation. N Engl J Med. 2022;387(21):1947–1956. doi:10.1056/NEJMoa2207304
-
Charging & Delivery:
-
Both defibrillators charged to max energy (e.g., 200 J biphasic).
-
Shocks delivered in rapid succession — ideally <1 second apart (simultaneous not required, and may be less effective).
-
-
Safety Protocols:
-
Clear communication — designate a leader to call “Clear!”
-
Ensure nobody is touching the patient.
-
Verify pad cables are not crossing to avoid arc or equipment failure.
-
-
When to Use:
-
Consider DSED after three failed standard defibrillation attempts.
-
Most often used during refractory OHCA with ongoing CPR.
-
Prognosis: Does DSED Improve Outcomes?
Evidence from the DOSE-VF Trial (NEJM 2022)
-
Survival to Hospital Discharge:
-
DSED: 30.4%
-
VC: 21.7%
-
Standard: 13.3%
-
-
Neurologically Intact Survival:
-
DSED: 27.4%
-
VC: 16.2%
-
Standard: 11.2%
-
-
VF Termination and ROSC:
-
DSED had higher rates of ROSC (46%) and VF termination (84%) than standard approaches.
-
Findings from 2024 Resuscitation Journal Secondary Analysis
-
In shock-refractory VF:
-
Survival with DSED: 28.6%
-
Survival with VC: 9.1%
-
Standard defibrillation: 0%
-
-
In recurrent VF:
-
DSED still showed a survival advantage over VC and standard approaches.
-
Adjunctive Therapies in Refractory Ventricular Arrhythmias
Medications
-
Esmolol:
-
Ultra-short-acting beta-1 blocker.
-
Used to blunt catecholamine-driven myocardial excitability.
-
Dose: 500 mcg/kg IV bolus → 50–100 mcg/kg/min infusion.
-
Some observational studies suggest improved ROSC and survival.
-
-
Lidocaine:
-
Alternative to amiodarone.
-
May be preferred in early refractory VF, especially in cases of ischemia or torsades.
- “A retrospective ‘target trial emulation’ comparing amiodarone and lidocaine for adult out-of-hospital cardiac arrest resuscitation” (March 2025) demonstrated lidocaine administration compared to amiodarone was associated with higher odds of:
-
- prehospital return of spontaneous circulation (ROSC) (36.0% vs. 30.4%; adjusted odds ratio [aOR]: 1.29)
- fewer post-drug defibrillation attempts
- greater odds of survival to hospital discharge (35.1% vs. 25.7%; OR: 1.54)
-
-
-
Magnesium:
-
Consider in torsades de pointes or suspected hypomagnesemia.
-
Mechanical Support & Other Techniques
-
Mechanical CPR: Allows uninterrupted compressions during defibrillator coordination.
-
ECMO: For patients with persistent VF and good pre-arrest function; enables continued perfusion while managing arrhythmia.
-
PCI: Should be considered early in arrest of suspected ischemic origin.
-
Stellate Ganglion Block (experimental): May blunt sympathetic surge in refractory cases.
Take Aways
-
DSED is not yet standard of care but supported by growing clinical evidence, especially for shock-refractory VF.
-
It shows higher survival and neurologically intact outcomes compared to standard and VC strategies.
-
Implementation requires two defibrillators, team coordination, and protocol familiarity.
-
Should be combined with appropriate pharmacologic and procedural adjuncts for optimal effect.
Want to learn more? Listen to our Podcast on Electrical Storm below!
References
-
Cheskes S, Verbeek PR, Drennan IR, et al. Defibrillation strategies for refractory ventricular fibrillation. N Engl J Med. 2022;387(21):1947–1956. doi:10.1056/NEJMoa2207304
-
Cheskes S, Drennan IR, Turner L, Pandit SV, Dorian P. The impact of alternate defibrillation strategies on shock-refractory and recurrent ventricular fibrillation: A secondary analysis of the DOSE VF cluster randomized controlled trial. Resuscitation. 2024;198:110186. doi:10.1016/j.resuscitation.2024.110186
-
Renslow M, Maloney J, Snell A. Dual Sequential Defibrillation (DSD). REBEL EM. Published April 8, 2019. Accessed April 23, 2025. https://rebelem.com/dual-sequential-defibrillation-dsd
-
Advanced Cardiovascular Life Support. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK544231
-
Cheskes S, Turner L, Drennan IR, et al. Outcomes of patients with recurrent ventricular fibrillation treated with alternative defibrillation strategies: a DOSE VF sub-analysis. Resuscitation. 2025;191:109910. [ScienceDirect Access via NYU Library]
-
Panchal AR. Updates in the Management of Refractory Ventricular Tachycardia or Ventricular Fibrillation Arrest. ACEP Now. Published August 9, 2023. Accessed April 23, 2025. https://www.acepnow.com/article/updates-in-the-management-of-refractory-ventricular-tachycardia-or-ventricular-fibrillation-arrest
- Smida T, Crowe R, Price BS, et al. A retrospective ‘target trial emulation’ comparing amiodarone and lidocaine for adult out-of-hospital cardiac arrest resuscitation. Resuscitation. 2025;208:110515. doi:10.1016/j.resuscitation.2025.110515
