The Case
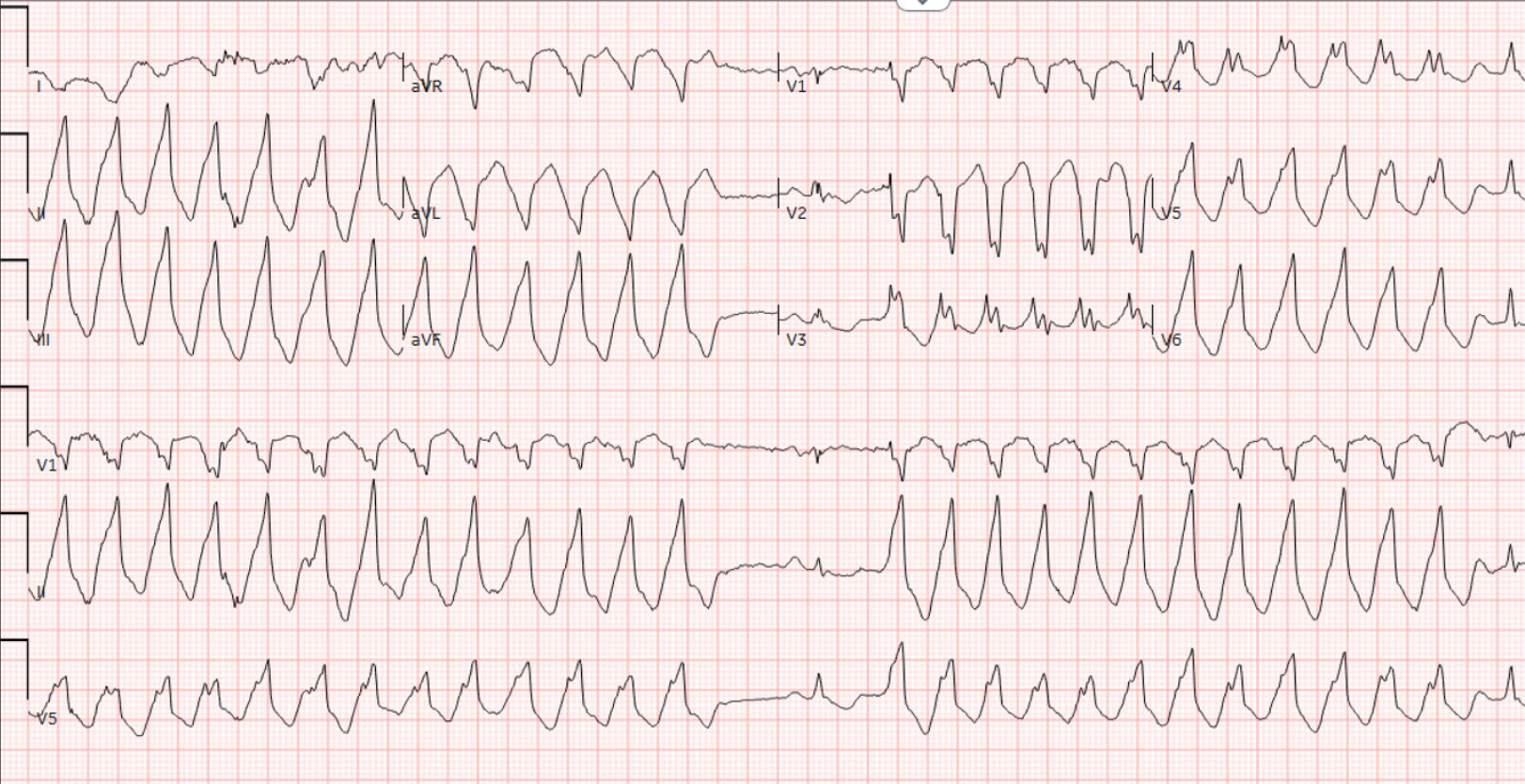
A 33 year old male with a PMH of AICD presents with palpitations and shortness of breath that began abruptly 30 minutes prior to arrival while working out at the gym. The patient was found to be in a wide complex tachycardia suspected to be ventricular tachycardia. Following lack of response to anti-arrhythmic medication, the patient was successfully electrically cardioverted with 200J. The following ECG was obtained:
Show Details
EKG Characteristics
-
Rate
60
-
Rhythm
Normal Sinus Rhythm
-
Intervals
Normal PR, QRS, QT intervals
-
Axis
Normal
-
ST Segments
T-wave inversion in lateral leads (aVL, V3, V4, V5, V6)
-
Additional Features
Epsilon Wave V1, V2, V3
Diagnosis
Arrhythmogenic Right Ventricular Cardiomyopathy
Questions
-
What underlying cardiac conditions may be a cause of ventricular arrhythmias in young patients without cardiovascular risk factors?
1. Brugada Syndrome 2. Hypertrophic Cardiomyopathy 3. Long QT Syndrome 4. Arrythmogenic Right Ventricular Cardiomyopathy 5. Congenital Heart Disease 6. Myocarditis 7. Anomalous Coronary Artery
Discussion
The patient reports he was in his usual state of health until 30 minutes before arrival, when he developed sudden onset symptoms of palpitations and shortness of breath while working out at the gym. Initial vitals BP 127/106, HR 150, Resp 15, temp 97.4 F, O2 100% (RA).
The following EKG was obtained:
The patient was alert with reassuring signs of perfusion. An Amiodarone bolus with drip was trialed without improvement in the arrhythmia. At the advice of cardiology, a lidocaine bolus was trialed, but also failed to terminate the arrhythmia.
The patient was ultimately cardioverted with 200J synchronized cardioversion using 8 mg of etomidate as a sedative.
Arrhythmogenic Right Ventricular Cardiomyopathy
Epidemiology:
Thought to be somewhere between 1/2000 and 1/5000 in Central European demographics. While uncommon is thought to be a leading cause of sudden cardiac death in young people (3).
Pathophysiology:
Genetically inherited condition which primarily affects the intercalated disks in cardiac tissue, leading to a loss of structural integrity of cardiomyocytes. As the disease progresses there will be a combined loss of myocytes in the right ventricle with fibrofatty replacement. The replacement often starts in the subepicardium to midmyocardium and then progresses to transmural fibrosis with advanced ARVC. Endurance sports and frequent strenuous exercise promotes the development and progression of ARVC by increasing the ventricular load and mechanical stress on the heart.
Diagnosis:
ARVC is typically diagnosed between 20 and 40 years. It is exceedingly rare to be diagnosed in patients under 10. The most common symptoms are palpitations or syncope during exercise. Patients can also be asymptomatic and be identified after a family member is diagnosed. In addition, sudden cardiac death can be the first sign of ARVC, and up to 20% of patients diagnosed with ARVC first present with cardiac arrest.
The diagnosis of ARVC utilizes major and minor criteria, involving many different categories. While confirmation of this cardiomyopathy in the ED is not typically possible, the following ECG findings (based on the 2020 International Criteria for Diagnosis of Arrhythmogenic Right Ventricular Cardiomyopathy) can provide clues for identification:
Repolarization Abnormalities:
Major
-
Inverted T waves in right precordial leads (V1,V2, and V3) or beyond in individuals with complete pubertal development (in the absence of complete arrhythmogenic right ventricular cardiomyopathy, RBBB)
Minor
-
Inverted T waves in leads V1 and V2 in individuals with completed pubertal development (in the absence of complete RBBB)
-
Inverted T waves in V1, V2, V3 and V4 in individuals with completed pubertal development in the presence of complete RBBB
Depolarization and Conduction Abnormalities:
-
Epsilon wave (reproducible low-amplitude signals between end of QRS complex to onset of the T wave) in the right precordial leads (V1 to V3)
-
Terminal activation duration of QRS ≥55 ms measured from the nadir of the S wave to the end of the QRS, including R’, in V1, V2, or V3 (in the absence of complete RBBB)

Management:
- Clinical management primarily involves restricting physical activity, as exercise can trigger arrhythmias and accelerate disease progression. This measure aims to reduce the risk of sudden death and heart failure. The recommendation is that individuals (including those who are genotypically positive but phenotypically negative) limit their exercise to less than 650 MET hours per year. This corresponds to about 30 minutes of brisk walking per day. This restriction helps delay the manifestation of the disease’s symptoms in phenotype-negative individuals.
- Pharmacological treatment for ARVC involves suppressing arrhythmia, preventing thrombus formation in patients with atrial fibrillation, and managing heart failure.
- Beta blockers prevent arrythmias and reduce RV wall stress
- Class III and Ic antiarrhythmics are used in patients with persistent ventricular arrythmias.
- Patients with refractory Ventricular tachycardia may benefit from ablations, however recurrence is as high as 50-75% in just 3 years due to disease progression.
- ICDs prevent sudden cardiac death.
Pearls
- Consider arrhythmogenic right ventricular cardiomyopathy as an etiology of ventricular arrhythmias and cardiac arrest in patients, especially between the ages of 20 and 40.
- Typical ECG findings of ARVC include T wave inversions in the precordial leads (V1-V4) and Epsilon waves (found in 50% of ARVC cases) which appear as small amplitude areas of depolarization that tend to occur at the end of QRS complexes and during the beginning of ST segment.
- Key management of ARVC involves avoidance of excessive exercise, AICD placement, and anti-arrhythmic medications.
Sources
References:
- Lüker J, Sultan A, Plenge T, et al. Electrical cardioversion of patients with implanted pacemaker or cardioverter-defibrillator: results of a survey of german centers and systematic review of the literature. Clin Res Cardiol. 2018;107(3):249-258. doi:10.1007/s00392-017-1178-y
- Elgaard AF, Dinesen PT, Riahi S, et al. External cardioversion of atrial fibrillation and flutter in patients with cardiac implantable electrical devices. Pacing Clin Electrophysiol. 2023;46(2):108-113. doi:10.1111/pace.14616
- Shah SN, Umapathi KK, Rout P, et al. Arrhythmogenic Right Ventricular Cardiomyopathy. [Updated 2024 Mar 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470378/

