Background
Thanks to Salim Rezaie (@srrezaie) for peer-reviewing this post.
Acute headache is a common emergency department presentation that accounts for 1-2% of all encounters (Goldstein 2006) The differential includes many life-threatening diagnoses, one of which is aneurysmal subarachnoid hemorrhage (SAH). With an estimated overall prevalence of 2% and a 1-month mortality of 40-45%, SAH is a high-risk disease that no emergency physician wants to miss (Linn 1996). 30% of those patients that survive will have severe disabilities (Hop 1997). Rebleeding following initial presentation is the largest cause of death. There is a 1.5% risk of rebleeding per day and a 15-20% risk in the first two weeks (Kassell 1983, Samandouras 2010). Early diagnosis and aneurysm repair using endovascular or surgical treatment before rebleeding occurs improves outcomes. However, about 5% of SAH are misdiagnosed on the first Emergency Department (ED) assessment because up to 50% of SAH patients present with no neurological deficits, providers fail to correctly interpret test results, or providers fail to appreciate the wide spectrum of symptoms that a SAH can present with (Vermeulen 2007, Weir 1994).
The current guidelines put forth by the American Heart / Stroke Association in 2012 state that the acute diagnostic workup for suspected SAH should include a noncontrast head CT (NCHCT), which, if nondiagnostic, should be followed by a lumbar puncture (LP). (Class I; Level B evidence) (Connolly 2012). However, recent studies using modern CT scanners have demonstrated a near 100% sensitivity for detecting SAH if the CT is performed within 6 hours and interpreted by qualified radiologists. This data questions the role of LP after a negative NCHCT when performed within this time window.
Clinical Question
What is the sensitivity of brain CT using modern scanners when performed within 6 hours of headache onset to exclude SAH in neurologically intact patients.
Design
Systematic review and meta-analysis
Literature Search
The electronic search included Ovid MEDLINE, Ovid EMBASE, Web of Science, and Scopus from inception (Ovid MEDLINE and Scopus 1966, Ovid EMBASE 1988 and Web of Science 1975) until April 2015.
Outcomes
Sensitivity of NCHCT performed within 6 hours for excluding the diagnosis of SAH
Inclusion
Original research studies of adults with a history concerning for SAH who received a NCHCT within 6 hours of onset of headache
Excluded
Studies involving patients < 15 years of age, older CT scanners (< 16-slice) and those in which patients did not receive their CT scan within 6 hours.
Primary Results
Primary Results
- 5 trials included with 8907 patients
- Performed three analyses:
- “Worst case scenario”: Included patients found to have vascular abnormalities on angiography but unclear if had thunderclap presentation
- “Intermediate case scenario”: Excluded those with vascular abnormalities but unclear presentations (as above)
- Three study analysis: Only included articles with direct information in 2 by 2 tables
Critical Findings:
- “Worst Case Scenario”
- 13 missed SAH (incidence 1.46/1000) on brain CT within 6 hours
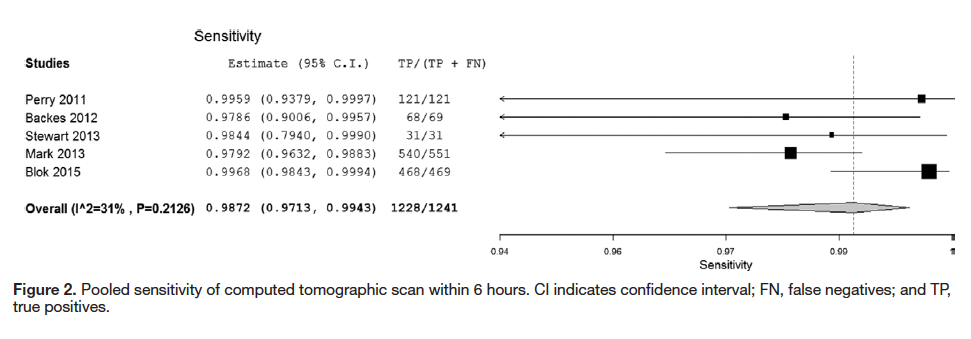
- Sensitivity: 0.987 (95% CI 0.971 – 0.994)
- Specificity 0.999 (95% CI 0.993 – 1.0)
- (+) LR: 921.9 (95% CI 139 – 6103)
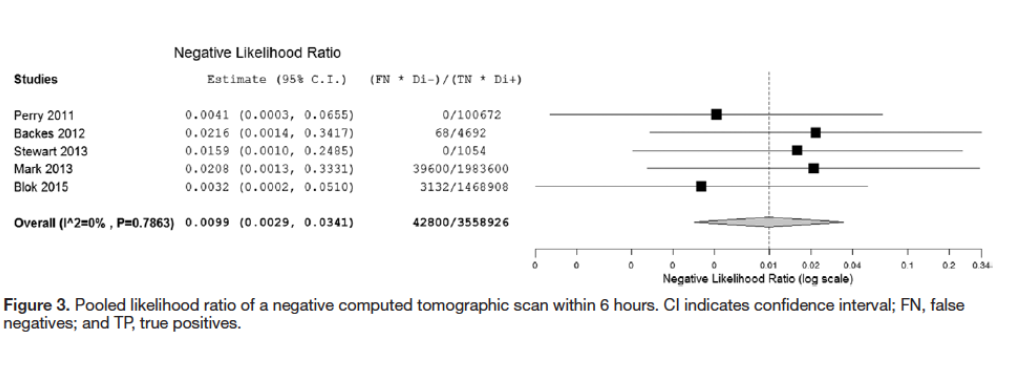
- (-) LR :0.010 (95% CI 0.003 – 0.034)
- “Intermediate Case Scenario”
- 9 missed SAH on brain CT within 6 hours
- Sensitivity 0.989 (95% CI 0.980 – 0.994)
- Specificity 1.0 (95% CI 0.993 – 1.0)
- Excluding 2 Studies Without Direct Information
- incidence of SAH was 19.1%
- 1/1155 missed SAH (incidence 0.87/1000) on brain CT within 6 hours
- Sensitivity: 0.986 (95% CI 0.951 – 0.996)
- Specificity 0.996 (95% CI 0.974 – 0.999)
Strengths
- Extensive literature search performed and a medical librarian was consulted to ensure all relevant articles considered
- Interobserver agreement for article inclusion was high (87.5%)
- Study quality was assessed using the QUADAS-2 tool
- Calculated heterogeneity was low allowing for a composite sensitivity and negative likelihood ratio calculation
- Primary outcomes based on a “worst-case scenario.”
Limitations
- There was significant variation in the incidence of SAH among the studies
- The “gold standard” test for SAH was unevenly applied across all studies
- The studies by Blok and Mark et al, only included patients with negative CTs, so estimations of their true positives and negatives had to be made using the Perry et al study numbers for incidence of 12.7% and the proportion of SAH patients who presented within 6 hours, which was 30%
- All NCHCTs were read by board certified radiologists.
- The Perry study, which contributed the largest number of patients, did not perform LP in all patients. This could lead to missed cases and an overestimation of sensitivity
- Included studies had incidences of SAH that seem higher than what is typically seen in clinical practice
Other Issues
- Headache has a broad differential diagnosis and other dangerous etiologies may not be ruled out simply be performing a NCHCT (i.e. meningitis)
Author's Conclusions
“In patients presenting with thunderclap headache and normal neurological examination, normal brain CT within 6 hours of headache is extremely sensitive in ruling out aneurysmal SAH.”
Our Conclusions
A negative NCHCT performed within 6 hours of onset of headache in a neurologically intact patient with symptoms concerning for SAH has a robust negative likelihood ratio allowing to post-test risk stratify patients to a low enough level where the LP is unlikely to add to the clinical workup. Recent studies (Sayer 2015) looking at the yield of LP should be considered alongside this systematic review and meta-analysis.
Potential Impact To Current Practice
Clinicians can use this information to discuss harms and benefits of additional testing after a negative NCHCT in patients with suspected SAH presenting within 6 hours of symptom onset.
Bottom Line
An LP may not be necessary in patients presenting with suspected SAH who have a negative NCHCT within 6 hours of headache onset.
Read More
EMLitofNote: Is the 6-Hr CT for SAH Debate Over?
ERCast: The Subarachnoid Enigma
St. Emlyn’s Blog: Lets Talk About Subarachnoid Hemorrhage
The SGEM: SGEM #48 – Thunderstruck (Subarachnoid Hemorrhage)
The SGEM: SGEM #134 – Listen, to What the British Doctors Say About LPs Post CT for SAH
REBEL EM:
References
- Goldstein JN et al. Headache in United States emergency departments: demographics, work-up and frequency of pathological diagnoses. Cephalalgia 2006;26:684–90. PMID: 16686907
- Linn FH, Rinkel GJ, Algra A, van Gijn J. Incidence of subarachnoid hemorrhage: role of region, year, and rate of computed tomography: a meta-analysis. Stroke 1996;27:625–9. PMID: 8614919
- Hop JW, Rinkel GJ, Algra A, van Gijn J. Case-fatal- ity rates and functional outcome after subarachnoid hemorrhage: a systematic review. Stroke 1997;28: 660–4. PMID: 11765839
- Kassell NF, Drake CG. Review of the management of saccular aneurysms. Neurol Clin 1983;1:73–86. PMID: 6680167
- Samandouras G. The Neurosurgeon’s Handbook. Oxford: Oxford University Press, 2010.
- Vermeuleun, M, Schull, MJ. Missed Diagnosis of Subarachnoid Hemorrhage in the Emergency Department. Stroke. 2007; 38:1216-1221. PMID: 17322078
- Weir, B. Headaches from Aneurysms. Cephalalgia. 1994; 14:2:279-287. PMID: 8062361
- Connolly, ES et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2012 Jun;43(6)1711-37. PMID: 22556195
- Perry, JJ. et al. Sensitivity of computed tomography performed within six hours of onset of headache for diagnosis of subarachnoid haemorrhage: prospective cohort study. BMJ. 2011; 343:d4277. PMID: 21768192
- Sidman, R. et al. Subarachnoid hemorrhage diagnosis: lumbar puncture is still needed when the computed tomography scan is normal. Acad Emerg Med. 1996 Sep;3(9):827-31. PMID: 8870753
- Van der Wee N, et al. Detection of subarachnoid haemorrhage on early CT: is lumbar puncture still needed after a negative scan? J Neurol Neurosurg Psychiatry. 1995;58:357-9. PMID: 7897421
- Chu, K. et al. Spectrophotometry or Visual Inspection to Most Reliably Detect Xanthochromia in Subarachnoid Hemorrhage: Systematic Review. Ann Emerg Med. 2014;64:256-264. PMID: 24635988
- Sayer, D et al. An Observational Study of 2,248 Patients Presenting With Headache, Suggestive of Subarachnoid Hemorrhage, Who Received Lumbar Punctures Following Normal Computed Tomography of the Head. Journal of Academic Emergency Medicine. 2015 Nov; 22(11):1267-73. PubMed ID: 26480290
