Show Notes
Background
- In 2017, there were 219 million cases and 435,000 people deaths from malaria
- Five species: Falciparum, P. vivax, P. ovale, P. malariae, and P. knowlesi.
- Falciparum, Vivax and Knowlesi can be fatal
- History of recent travel to Africa (69% of cases in US), particularly to west-Africa should raise suspicion for malaria
Clinical Manifestations
- Average incubation period for Falciparum is 12 days
- 95% will develop symptoms within 1 month
- Clinical findings with high likelihood ratios include periodic fevers, jaundice, splenomegaly, pallor.
- Can also have vomiting, headache, chills, abdominal pain, cough, and diarrhea
- Severe malaria has a mortality of 5% to 30%, even with therapy
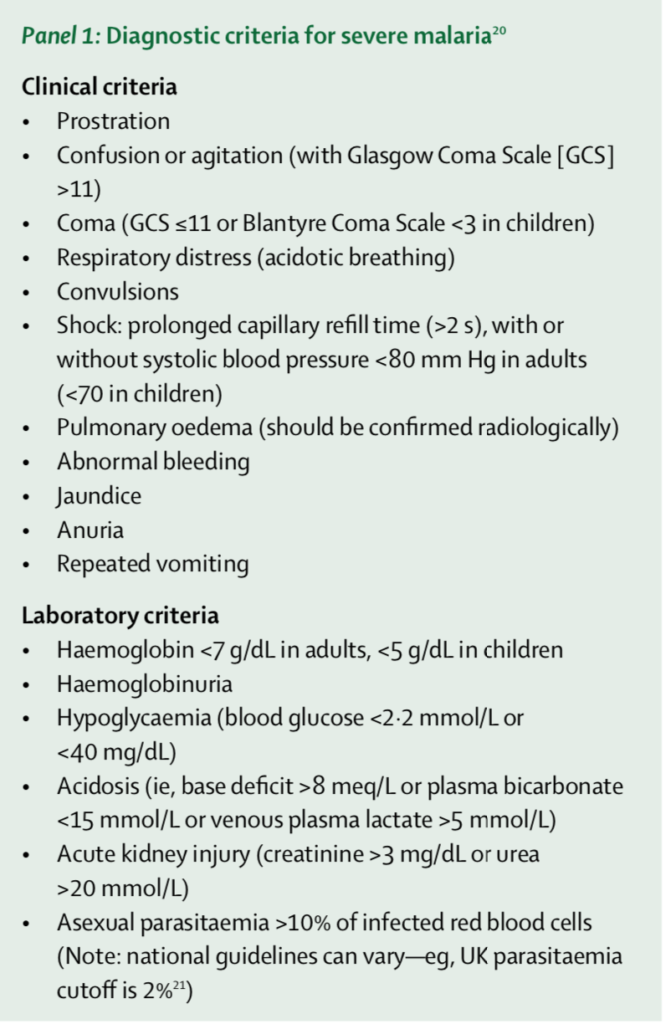
- Diagnostic criteria for severe malaria:
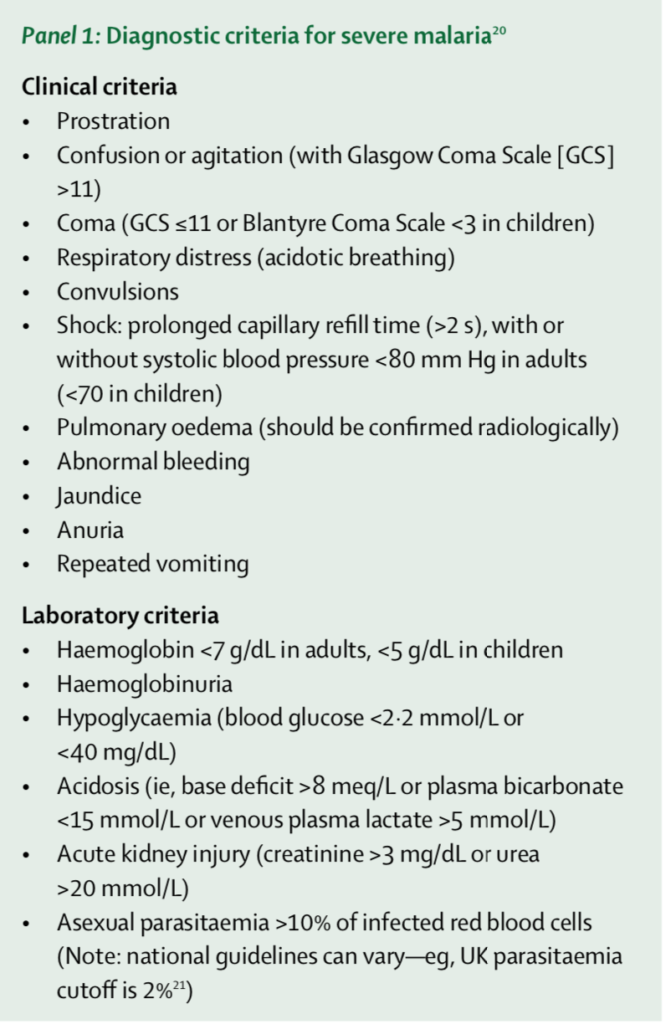
Ashley 2018
- Most common manifestations of severe malaria affect the brain, lungs, and kidneys
- Patients with cerebral malaria can present encephalopathic or comatose, some severe enough to exhibit extensor posturing, or seizures
- Can have acute lung injury with a quarter of these patients progressing to ARDS
- Can have AKI from ATN and resultant acidosis
- Labs may be unremarkable but watch for anemia and thrombocytopenia
- Hgb <5 has an OR = 4.9 for death
- Severe thrombocytopenia has an OR = 2.8
- Anemia + Thrombocytopenia has an OR = 13.8 (Lampah 2015, PMID 25170106)
- Watch for hypoglycemia
- Be mindful of co-infection with salmonella and HIV
- Obtain BCx, cover with ceftriaxone
Diagnosis
- Blood smear
- Thick smear to increase sensitivity for detecting parasites
- Thin smear for quantifying parasitemia and species
- The first smear is positive in over 90% of cases, but if suspicion is high, it has to be repeated BID for 2-3 days for proper exclusion of malaria (CDC 2019)
Management
- For uncomplicated, non-severe cases, most patients with falciparum should be admitted, especially those with no prior exposure to malaria parasites
- Malarone is one of the first line options
- Important to note that when they take this, ensure they take with milk or food containing fat to enhance absorption
- Severe Malaria
- Resuscitative efforts directed at affected organ
- Can deteriorate rapidly
- Initiate IV Artesunate if high level of suspicion
- Requires call to CDC: CDC Malaria Hotline: (770) 488-7788 or (855) 856-4713 (toll-free) Monday–Friday 9am–5pm EST – (770) 488-7100 after hours, weekends, and holidays
- Benzodiazepines for seizures
- Be judicious with fluids as this can precipitate pulmonary edema and cerebral edema
- a/w increased mortality in children at 48 hour
- (Maitland 2011, PMID: 21615299; Hanson 2013, PMID: 23324951)
Take Home Points
- This is going to be a diagnosis that is mainly made through a thorough history, and pay particular attention to those with recent travel to West-Africa
- The incubation period for falciparum is 12 days, but there is a range of weeks and we should consider Malaria when consistent symptoms develop within 1 month of travel to an endemic area
- Typical signs and symptoms for uncomplicated malaria are periodic fevers, jaundice, pallor
- Be mindful of end organ involvement, such as cerebral edema, ATN, and pulmonary edema; these cases are considered to be severe and treated differently than uncomplicated malaria
- Uncomplicated cases should get Malarone or Coartem
- Severe cases require IV Artesunate
- Be judicious with your fluid resuscitation as this can harm our patients
References
Centers for Disease Control and Prevention. CDC Parasites – Malaria. 2019 https://www.cdc.gov/parasites/malaria/index.html (7 July 2019, date last accessed)
Ashley EA, Pyae Phyo A, Woodrow CJ. Malaria. Lancet. 2018;391(10130):1608-21.
Hanson JP, Lam SW, Mohanty S, Alam S, Pattnaik R, Mahanta KC, et al. Fluid resuscitation of adults with severe falciparum malaria: effects on Acid-base status, renal function, and extravascular lung water. Crit Care Med. 2013;41(4):972-81.
Lampah DA, Yeo TW, Malloy M, Kenangalem E, Douglas NM, Ronaldo D, et al. Severe malarial thrombocytopenia: a risk factor for mortality in Papua, Indonesia. J Infect Dis. 2015;211(4):623-34.
Lokken KL, Stull-Lane AR, Poels K, Tsolis RM. Malaria Parasite-Mediated Alteration of Macrophage Function and Increased Iron Availability Predispose to Disseminated Nontyphoidal Salmonella Infection. Infect Immun. 2018;86(9).
Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot-Olupot P, Akech SO, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med. 2011;364(26):2483-95.
Park SE, Pak GD, Aaby P, Adu-Sarkodie Y, Ali M, Aseffa A, et al. The Relationship Between Invasive Nontyphoidal Salmonella Disease, Other Bacterial Bloodstream Infections, and Malaria in Sub-Saharan Africa. Clin Infect Dis. 2016;62 Suppl 1:S23-31.
Tintanelli, Judith E., et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. Eighth edition. New York: McGraw-Hill Education, 2016: p.1070-1077
World Health Organization. Guidelines for the treatment of malaria. Third edition
April 2015. WHO. 2015 https://www.who.int/malaria/publications/atoz/9789241549127/en/ (7 July 2019, date last accessed)
A special thanks to our editor:
Angelica Cifuentes Kottkamp, MD
Infectious Diseases & Immunology
NYU School of Medicine