Definition: An injury to the eye occurring as a result of direct trauma. It may cause visual changes, eye pain/discomfort, and changes to the appearance of the eye.
Approach: Be methodical with your history and physical. If the patient describes trauma that occurred to the eye, ask about the mechanism of the injury. This will help differentiate possible pathologies. A patient will also describe their eye complaints in a way that will help lead you to a diagnosis, such as having a “foreign body sensation” or seeing “flashing lights.”
Initial exam components needed for diagnosis:
- Visual acuity
- Confrontational visual fields
- Extraocular movements
- Pupillary reactions
- Check for afferent pupillary defect
- Slit lamp exam identifying structures of eye
- +/- Ocular ultrasound (if globe rupture suspected, however, any increased pressure can worsen injury)
Several differential diagnoses to consider:
- Globe Rupture (Open Globe)
- Hyphema
- Retrobulbar hematoma
- Retinal detachment
- Corneal abrasion/ulceration
Globe Rupture
Definition: A traumatic injury involving the breakdown in the integrity of the wall of the eye, either the sclera or cornea.
Diagnosis:
- Suspect globe rupture based on mechanism (blunt trauma, projectile injury, laceration of eyelid/periorbital area, metal on metal, high-speed machinery, explosions)
- Physical Exam
- Protruding foreign body in eye
- Eccentric/teardrop pupil
- Decreased visual acuity
- Afferent pupillary defect
- Extrusion of vitreous
- External prolapse of the iris or ciliary body
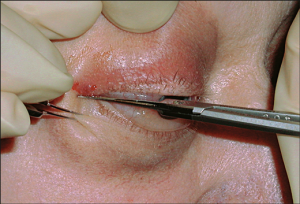
Positive Seidel Test – www.eyecalcs.com
- Tenting of the sclera or cornea at the site of globe puncture
- Volume loss of eye
- Seidel test à apply fluorescein dye to eye, which binds damaged corneal epithelium and turns green under light through a cobalt-blue filter or Wood lamp, and check for streaming of fluorescein-tinged aqueous humor; this indicates corneal laceration
- CT of orbit, sensitivity ranges from 56% to 70%, specificity 79% to 100% (Arey 2007, Hoffstetter 2010
Management:
- Prevent increased intraocular pressure (IOP)
- Head of bed at 30 degrees
- Avoid eye manipulation (do not measure eye pressure, retract lid, or perform ocular ultrasound)
- Cover with an eye shield (do not place eye patch as it exerts pressure on globe) – A paper cup can be used if an eye shield is not available
- Administer topical and systemic broad-spectrum antibiotics (Soheilian 2007)
- Update tetanus
- Give antiemetics to prevent nausea (which increases IOP)
- Give pain medicine
- Consult ophthalmology à even if CT negative, formal surgical evaluation may be needed if occult injury suspected
Hyphema
Definition: Blood in the anterior chamber of the eye occurring usually as a result of a ruptured iris root vessel, if secondary to trauma.
Diagnosis:
- Gross inspection of blood in anterior chamber
- Slit lamp exam à check anterior chamber for blood
People at risk:
- Sickle cell disease
- Bleeding diatheses
- Anticoagulant or antiplatelet medications
Management:
- Interventions aimed preventing secondary hemorrhage
- Elevate head of bed
- Dilate pupil
- Control intraocular pressure with topical beta-blockers, topical alpha-adrenergic agonists, or topical carbonic anhydrase inhibitors
- Although recommended, no solid evidence supports the use of cyclopegics, corticosteroids, bed rest, or patching to decrease secondary hemorrhage or affect visual acuity (Gharaibeh 2011)
- Limited studies supporting tranexamic acid and other antifibrinolytics to decrease secondary hemorrhage (Gharaibeh 2011)
- Consult ophthalmology
Retrobulbar Hematoma/Orbital Compartment Syndrome
Definition: Blood found behind the globe but within the orbit, mostly occurring secondary to trauma,
which can lead to optic nerve and retinal ischemia and ultimately, vision loss.
Diagnosis:
- Physical findings
- Proptosis
- Decreased visual acuity
- Afferent pupillary defect
- Decreased extraocular movements
- Increased intraocular pressure (> 40 mmHg)
- CT scan (do not delay management for CT scan if orbital compartment syndrome highly suspected)
Management:
- Consider lateral canthotomy if any of the following (Rowh 2015)
- Decreased visual acuity
- Restricted extraocular movement
- Afferent pupillary defect
- Proptosis
- Intraocular pressure > 40 mmHg
- Expeditious performance of a lateral canthotomy is vision saving. Do not delay.
- Consult ophthalmology emergently
Retinal Detachment
Definition: Retina separates from the underlying retinal pigment epithelium and choroid, either from accumulation of fluid between the two layers or vitreous traction on the retina.
Diagnosis:
- History (trauma followed by flashing lights/floaters/dark veil/curtains, or history of diabetes/sickle disease with the same complaints)
- Decreased peripheral or central visual acuity
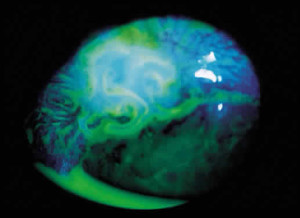
- Direct fundoscopic exam à pale billowing parachute with a large retinal detachment
- Dilated indrect ophthalmoscopic evaluation by ophthalmologist
- Ocular ultrasound à retinal detachment seen as hyperechoic membrane is posterior part of eye, sensitivity ranges from 97% to 100%, specificity 83% to 100% (Vrablik 2015)
Management:
- Consult ophthalmology for surgical repair
Take Home Points:
- Have a low threshold for suspecting globe injury especially if the mechanism is concerning.
- Retrobulbar hematoma/orbital compartment syndrome is a clinical diagnosis; perform a lateral canthotomy if any high-risk findings are present.
- Consult ophthalmology emergently for any traumatic eye injury
References:
- Arey ML et al. Computed tomography in the diagnosis of occult open-globe injuries. Ophthalmology 2007; 114(8):1448-1452. PMID: 17678689
- Hoffstetter P et al. Multidetector CT (MD-CT) in the diagnosis of uncertain open globe injuries. Rofo 2010; 182(2):151-154. PMID: 19859864
- Soheilian M et al. Prophylaxis of acute posttraumatic bacterial endophthalmitis: a multicenter, randomized clinical trial of intraocular antibiotic injection, report 2. Arch Ophthalmol 2007; 125(4):460-465. PMID: 17420365
- Gharaibeh A et al. Medical interventions for traumatic hyphema. Cochrane Database Syst Rev 2011; 19(1): CD005431. PMID: 21249670
- Rowh AD et al. Lateral canthotomy and cantholysis: emergency management of orbital compartment syndrome. J Emerg Med 2015. 48(3):325-330. PMID: 25524455
- Vrablik ME et al. The diagnostic accuracy of bedside ocular ultrasonography for the diagnosis of retinal detachment: a systematic review and meta-analysis. Ann Emerg Med 2015; 65(2):199-203. PMID: 24680547