Shoulder Dislocation Classifications (www.backandbodyclinic.co.uk)
Definition: Separation of the humerus from the scapula at the glenohumeral joint
Epidemiology:
- Most commonly dislocated joint in the body (17/100,000 people/year)
- Young males most commonly injured
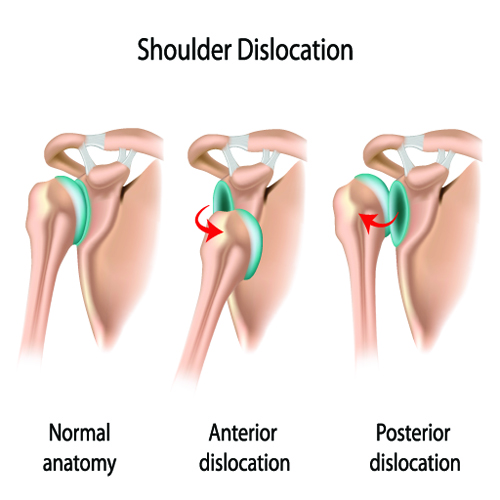
Classification:
- Anterior: 97% (Rowe 1956)
- Posterior: < 3%
- Inferior: < 1% (Also known as: Luxatio Erecta Humeri)
- IMAGE: www.newhealthadvisor.com
Mechanism:
- Anatomy
- Inherently unstable joint, relies on soft tissues for stabilization
- Only 25-30% of humeral head articulates with glenoid at any one time
- Axillary nerve wraps around surgical neck of humerus, most commonly injured nerve in dislocations of any direction
- Motor: Deltoid muscle
- Sensory: Anterolateral shoulder
- Anterior:
- Fall onto outstretched hand
- Force/blow to abducted and externally rotated +/- extended arm (ie. Blocking basketball shot)
- Posterior:
- ~50% secondary to trauma (Matsen 2007)
- 34% associated with seizures (Rouleau 2012)
- Strongest shoulder muscles (latissimus dorsi, pectoralis major, subscapularis) overpower others and pull shoulder internally, posteriorly
- Most common dislocation during seizures is anterior due to associated fall
- Inferior:
 Physical Examination:
Physical Examination:
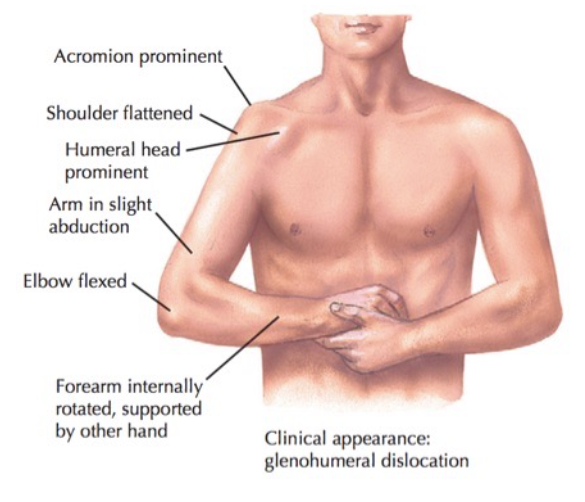
- Anterior
- Arm is held in internally rotated and abducted position
- Shoulder silhouette flattened with a prominent acromion
Netter’s Concise Orthopaedic Anatomy, Second Edition
- Posterior
- Arm is fixed, internally rotated, and adducted
- Posterior shoulder prominence
- Inferior
- Fixed, abducted position
- Arm held above the head
X-Ray Imaging (All Images in Gallery Below):
- For any suspected dislocation, obtain 3 views: AP, Scapula Y, and Axillary (see Approach to Traumatic Shoulder Pain for normal X-ray anatomy)
- Anterior Dislocation
- AP View: Humeral head dislocated anteriorly and rests under the coracoid process
- Scapula Y View: Scapula Y view: humeral head displaced medially (to the right) of the scapula
- Axillary view: Humeral head displaced anteriorly in front of the coracoid process
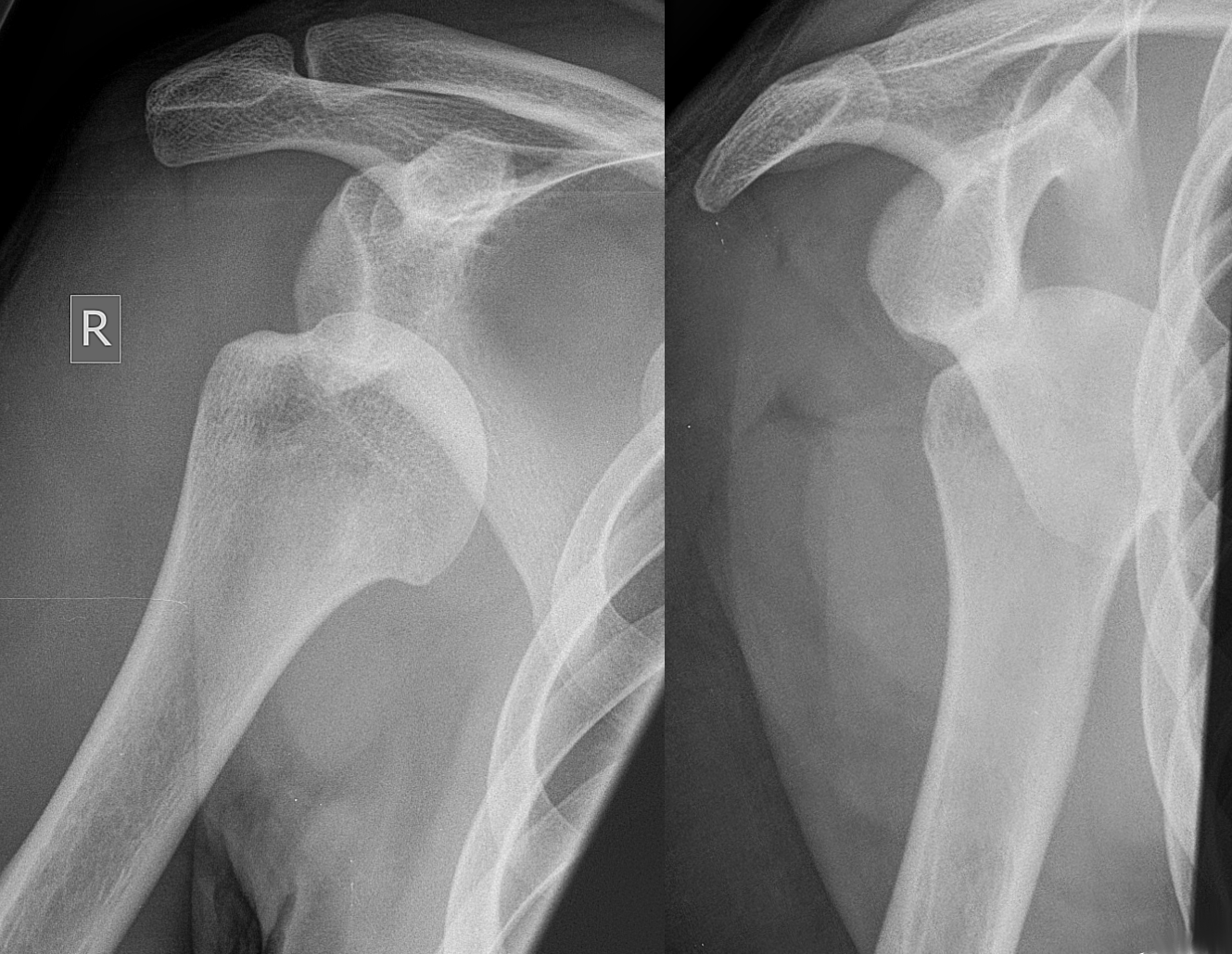
- Posterior Dislocation
- AP: “Light bulb on a stick” – often the only sign of a posterior dislocation. The humeral head does not appear displaced from the glenoid BUT it is internally rotated and thus the contour of the humeral head appears rounded – like a light bulb
- Scapula Y: Humeral head displaced laterally (to the left) of the scapula
- Axillary: Humeral head displaced posteriorly behind the coracoid process
- Inferior Dislocation
- Luxatio Erecta: Humeral head displaced inferior to glenoid and arm/humerus fixed above head/superiorly
Shoulder Dislocation X-Rays

Posterior Glenohumeral Dislocation: AP View (Case courtesy of Dr Henry Knipe, Radiopaedia.org. From the case rID: 35746)

Posterior Glenohumeral Dislocation: Oblique View (Case courtesy of Dr Henry Knipe, Radiopaedia.org. From the case rID: 35746)

Posterior Glenohumeral Dislocation: Axillary View (Case courtesy of Dr Sigmund Stuppner, Radiopaedia.org. From the case rID: 44745)

Inferior Glenohumeral Dislocation: Luxatio Erecta (Case courtesy of Dr Andrew Ho, Radiopaedia.org. From the case rID: 22924)
Hill Sachs Lesion (www.wikimedia.org)
Important Additional X-Ray Findings
- Hill Sachs Lesion
- Impaction fracture of humeral head against glenoid rim
- Anterior dislocations,
- Occurs against posterolateral surface
- Incidence rate 40-90%
- As high as 100% in recurrent dislocations (Provencher 2012)
- Posterior dislocations
- Occurs against anterolateral surface (“reverse Hill Sachs lesion”)
- Incidence 86%.
- May require accentuating rotational force (internal vs external) when reducing dislocation to dislodge the lesion off glenoid rim
- Bankart Lesion
- Detachment of anterior inferior labrum from glenoid
- “Soft” – Labrum only
- “Bony” – impaction fracture involving glenoid margin
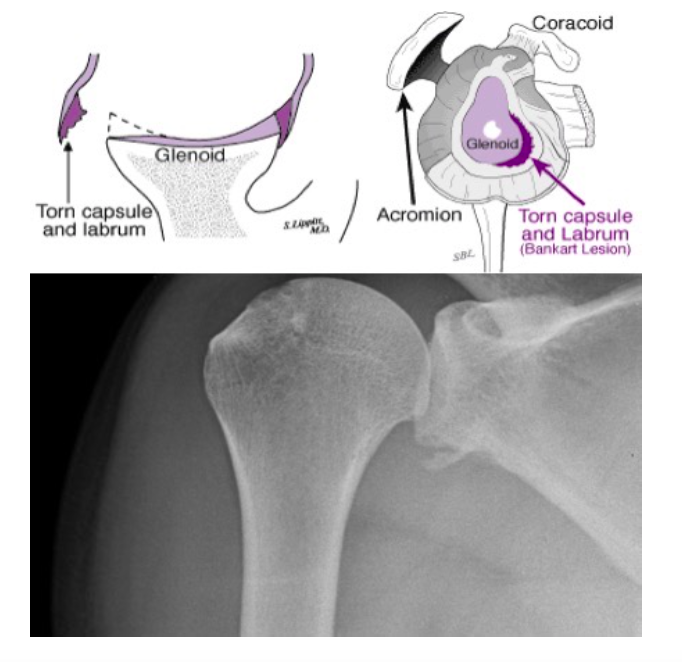
Bankart Lesion (www.orthop.washington.edu)
Management/Reduction Techniques
- Provide adequate analgesia
- The more the patient tenses his or her muscles from pain, the more difficult it will be to reduce the joint
- Consider systemic analgesia vs intraarticular local anesthetics vs both
- Procedural sedation may be required in select cases
- Complete a full neurologic and vascular assessment prior to the performance of any manipulation technique
- Anterior
- Cunningham Technique
- Physician massages the patient’s biceps muscle as the patient holds arm adducted and elbow flexed
- Patient gradually moves shoulders up and back (shoulder shrug) as tolerated
- Cunningham Technique
- Stimson Maneuver
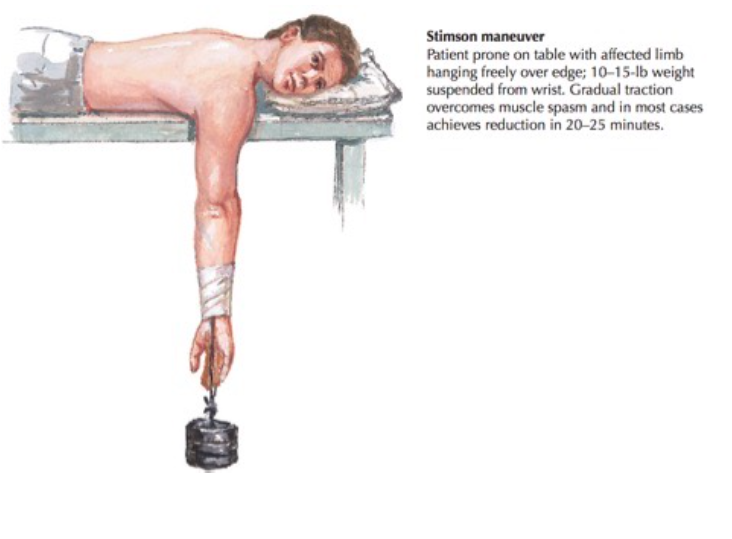
Stimson Maneuver (Netter’s Concise Orthopedic Anatomy 2nd Edition)
- Scapular Manipulation
- Stimson technique applied
- Scapula manipulated counterclockwise: stabilized superiorly, medial force applied on inferior angle

Scapular Manipulation with Stimson (aibolita.com)
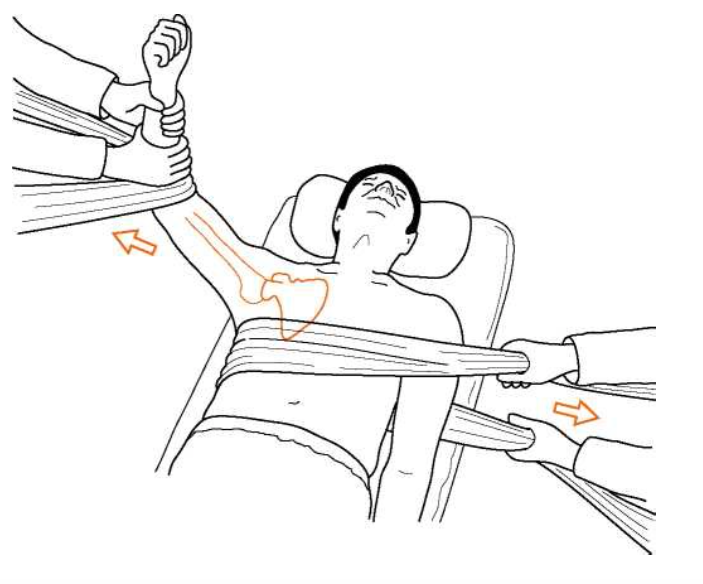
- Traction-Countertraction
- Gradual, smooth traction is applied to the affected arm until patient’s muscles relax or tire sufficiently to release the dislocated humeral head
- An assistant maintains counter traction to maintain patient in place
- Milch
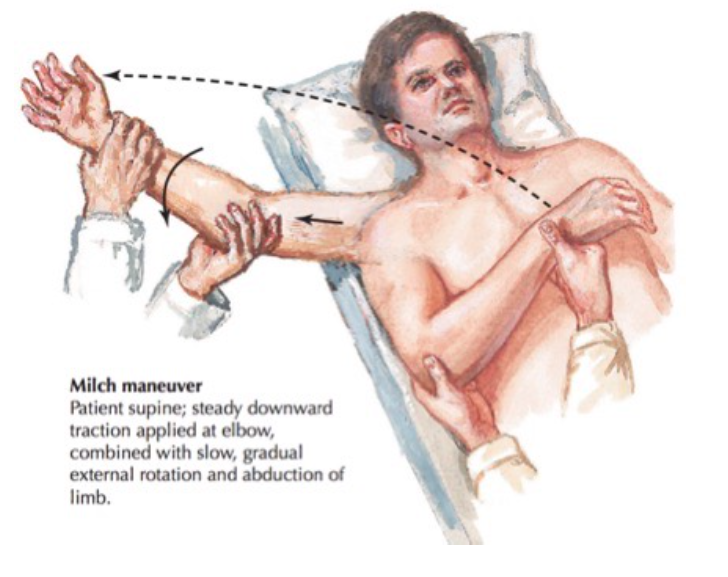
Milch Technique (Netter’s Concise Orthopedic Anatomy 2nd Edition)
- Posterior: requires 2 operators
- Traction-Countertraction recommended for all posterior dislocations
- Sitting patient upright and applying forward traction might be useful
- Inferior
- Arm traction superiorly with gradual shoulder adduction
- Sheet wrapped around upper torso to hold patient in place
- Traction-Countertraction
- Two-Step (Youm 2014)
- Arm traction superiorly while pushing humerus laterally
- This will either reduce the shoulder entirely or convert it to anterior dislocation, which can be reduced as above
Relative Contraindications to ED Reduction:
- Associated fracture of humeral neck
- Associated nerve injury/deficit
- Suspected major vascular injury
- Chronic Dislocation
- > 48 hours
- Success rate exceedingly low
- Refer to orthopedics for surgical evaluation if initial attempts fail
Follow Up
- Immobilize in sling for 3-4 weeks (older patients 1-2 weeks to avoid joint stiffening)
- Rehab should begin with passive range of motion exercises
- Anterior dislocations: no external rotation past neutral and no abduction past 90 degrees for the first 4-6 weeks
- Posterior dislocations: no internal rotation for first 4-6 weeks.
Take Home Points:
- Be vigilant for concomitant neurovascular injuries and always perform a full neurovascular assessment before and after reduction
- Carefully review radiographs for posterior dislocations as they may appear “normal” on first glance
- Be comfortable with multiple reduction techniques. No one approach will reduce all shoulder dislocations.
- Joint injections and systemic analgesia will facilitate reduction. Depending on patient response to initial attempts, procedural sedation may be necessary.
Read More:
LITFL: Posterior Shoulder Dislocation
LITFL: Cunningham’s Shoulder Relocation
EM Sandbox: The Cunningham Technique – Deep Dive Swaminathan
References
Youm T et al. Acute Management of Shoulder Dislocations. J Am Acad Orthop Surg. 2014 Dec;22(12):761-771.PMID: 25425611.
Rowe CR: Prognosis in dislocations of the shoulder. J Bone Joint Surg Am 1956; 38(5):957-977 PMID 13367074
Matsen FA et al. Principles for the evaluation and management of shoulder instability. Instr Course Lect 2007; 56:23-34. PMID: 17472289
Rouleau DM et al. Incident of associated injury in posterior shoulder dislocation: Systematic review of the literature. J Orthop Trauma 2012 ;26(4):246-251. PMID: 22183196
Robinson CM, Aderinto J. Posterior shoulder dislocations and fracture- dislocations. J Bone Joint Surg Am 2005; 87 (3):639-650. PMID: 15741636
Patel DN et al. Luxatio erecta: Case series with review of diagnostic and management principles. Am J Orthop 2011;40(11): 566-570. PMID: 22263209
Groh GI et al. Results of treatment of luxatio erecta (inferior shoulder dislocation). J Shoulder Elbow Surg 2010;19(3):423-426. PMID: 19836975
Provencher MT et al. The Hill-Sachs lesion: Diagnosis, classification, and management. J Am Acad Orthop Surg 2012;20(4):242-252. PMID: 22474094
Schwartz D. Emergency Radiology Case Studies. Upper Extremity: Patient 6. 271-279. McGraw-Hill Education / Medical; 1 edition (November 26, 2007)
Thompson J, Netter F, Machado C. Netter’s Concise Orthopaedic Anatomy. Second edition. Saunders Elsevier 2010.




