Definition: An infection of the cornea caused by the herpes simplex virus (HSV).
Epidemiology:
- Most frequent cause of corneal blindness in the United States
- Most common source of infectious blindness in the Western world. Approximately 2 million people worldwide have impaired vision from herpetic eye disease (Farooq 2012)
Pathophysiology:
- Primary infection: occurs most commonly in the mucocutaneous or ocular distribution of the trigeminal nerve, and can present as a non-specific upper respiratory infection
- Latency: the virus spreads from the infected epithelial cells to the cell body in the trigeminal ganglion where the virus persists indefinitely in a latent state
- Reactivation: interneuronal spread of HSV within the ganglion allows patients to develop subsequent ocular disease without ever having had primary ocular HSV infection
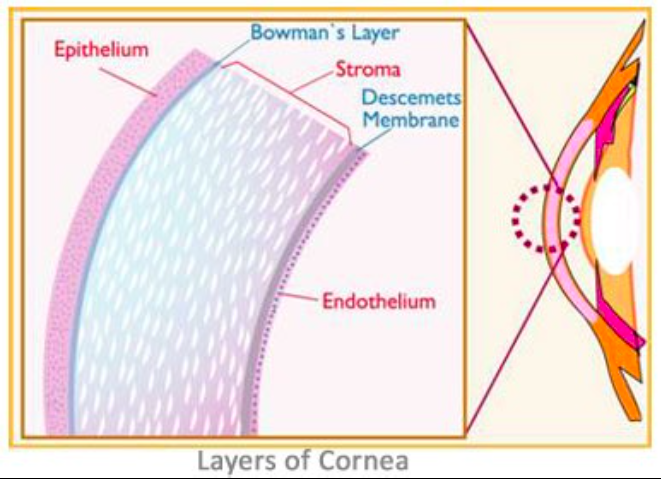
Corneal Layers – emaze.com
- HSV keratitis can be divided into 3 types: epithelial, stromal, and endothelial (White 2014)
- Epithelial: caused by actively replicating virus and occurs in the outermost layer of the cornea
- Stromal: caused by immune mechanisms and occurs in deeper layers
- Endothelial: caused by chronic inflammation and occurs in deeper layers
- Sequelae: Recurrent HSV keratitis can cause corneal scarring, ulceration, and perforation, ultimately leading toastigmatism and permanent vision loss.
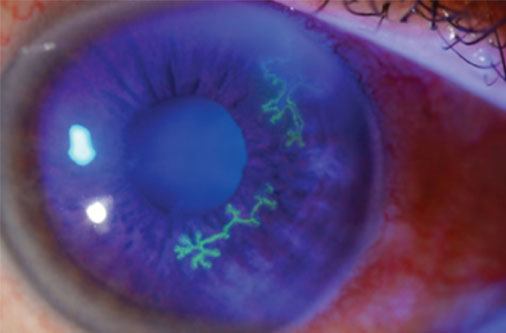
Dendritic Lesions (optometrist.com.au)
Symptoms:
- Eye pain
- Corneal injection
- Visual changes (blurry vision, decreased visual acuity)
- Tearing
- Discharge
- Photophobia
Physical exam:
- Visual acuity should be performed in all patients
- Fluorescein staining
- May reveal dendritic lesions (linear branching patterns with terminal bulbs)
- If the lesion enlarges, it can form a geographic ulcer
- Slit lamp exam
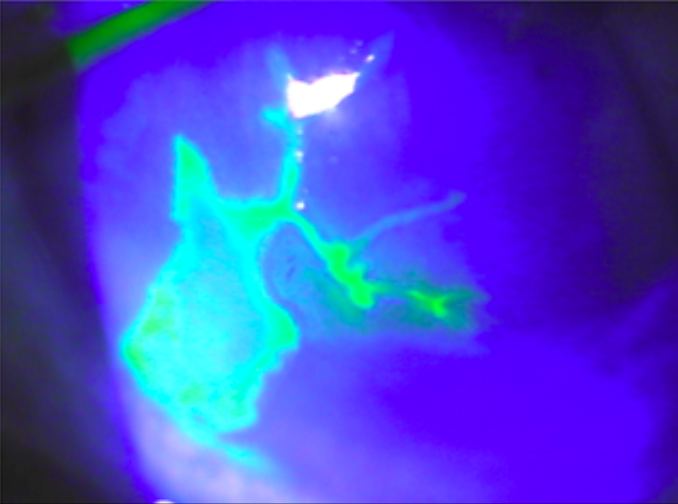
Geographic Ulcer – lasereyeconsultant.co.uk
- Used to identify disease in deeper (stromal + endothelial) layers
- Stromal disease shows up primarily as an inflammatory infiltrate with stromal edema, vascularization, and scarring
Diagnostics:
- The diagnosis of HSV keratitis is based on clinical eye exam.
- In the absence of dendritic lesions, decreased corneal sensation should increase concern for herpetic keratitsis (Weiner 2013)
- Viral culture
- Gold standard test
- Impractical in the ED: expensive, delayed
- Ophthalmology may perform additional testing, such as viral culture/PCR and Tzanck smear, to confirm the diagnosis but these are not routinely recommended (Welder 2012)
- Pitfalls: these tests are only positive when live virus is present, and cannot be used to diagnose stromal keratitis (White 2014)
Management:
- Most cases of HSV epithelial keratitis resolve spontaneously within 3 weeks. However, the American Academy of Ophthalmology recommends treatment of epithelial keratitis to prevent recurrence and progression to stromal or endothelial keratitis.
- Epithelial keratitis:
- Trifluridine 1% solution: 1 drop Q2hours for 7 days OR
- Ganciclovir 0.15% gel: five times per day
- Oral antiviral agents (not FDA approved, but equal efficacy in studies) (Wilhelmus 2010)
- Corneal debridement
- Stromal and endothelial keratitis:
- Urgent referral to ophthalmology
- Topical corticosteroid
- Oral antiviral agents for 10 weeks as prophylaxis reduces the rate of recurrent herpetic keratitis (Wilhelmus 1999)
Take Home Points:
- Fluorescein is an essential tool in the diagnosis of HSV keratitis
- Identifying the type of HSV keratitis is crucial, as it will guide treatment
- Update tetanus vaccination
- Consult ophthalmology if there is concern for HSV keratitis as these patients require close and frequent follow-up
References:
Farooq AV et al. Herpes simplex epithelial and stromal keratitis: an epidemiologic update. Surv Ophthalmol 2012; 57(5):448-462. PMID: 3652623
Wilhelmus KR et al. Antiviral treatment and other therapeutic interventions for herpes simplex virus epithelial keratitis. Cochrane Database Syst Rev 2010; (12): CD002898. PMID: 4739528
Weiner et al. Demystifying the ocular herpes simplex virus. American Academy of Ophthalmology. Link
McDonald et al. Management of epithelial herpetic keratitis: an evidence based algorithm. Link
Welder et al. Herpes simplex keratitis. University of Iowa Health Care. Link
Wilhelmus KR et al. Herpetic Eye Disease Study. A controlled trial of topical corticosteroids for herpes simplex stromal keratitis. Ophthamology 1999; 101(12):1883-1896. PMID: 7997324
Chan RV et al. Herpes simplex keratitis – Latin America. American Academy of Ophthalmology. Link
White et al. Herpes simplex keratitis: A treatment guideline – 2014. Link
Dear Christina Chien.
Thank you for the clear explanation and outline of Herpes Keratitis. I enjoyed reading your article.
I am also writing to you to ask for your kind permission to use the picture of an dendritic corneal ulcer for my Ophthalmic Nursing essay.
Your early response to this e mail would be very much appreciated as the essay submission is due in 3 weeks time.
Kind regards
Dorothea Clarke
The image was obtained from optometrist.com.au
You would have to ask them for permission.