Definition: Clot formation within the major cerebral veins including the dural sinuses (superior sagittal sinus, straight sinus and transverse sinuses) as well as the cortical veins, vein of Galen and jugular veins.
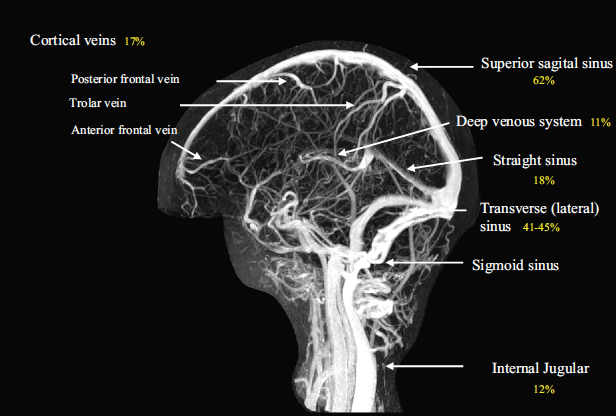
MRV of the Cerebral Venous System (Saposnik 2011)
Epidemiology
- More common in young (median age = 38) women (60-75% of cases)
- Rare disease: 0.5-1% of all strokes (Saposnik 2011)
- Mortality: 10-30% (Williams 2004)
- Risk Factors
- Virchow’s Triad: stasis of blood, changes to vessel walls and blood composition
- Acquired risk factors: infections (otitis, mastoiditis), surgery, pregnancy, trauma, cancer, exogenous hormone use
- Genetic risk factors: inherited thrombophilia
Pathophysiology
- Major veins drain cerebral blood into dural sinuses.
- Two different mechanisms for cerebral venous thrombosis (CVT) (Stam 2005)
- Thrombosis of cerebral veins leading to local effects from venous obstruction
- Thrombosis of major cerebral sinuses causing intracranial hypertension
- In majority of patients, both mechanisms occur simultaneously
Presentation
- CVT often presents with non-specific symptoms making it difficult to diagnose. On first presentation, patients often do not have any physical exam findings.
- History
- Severe headache – 90% (Stam 2005)
- Sensitive but highly non-specific
- 25% of patients will have headache alone (Saposnik 2011)
- Typically is a gradual onset of headache that progresses over days to weeks
- Rarely, can mimic subarachnoid hemorrhage (acute onset)
- Neurologic complaints: weakness, paresthesias, blurred or double vision
- Severe headache – 90% (Stam 2005)
- Clinical Manifestations
- Highly dependent on location of thrombosis and acuity of onset
- Manifestations resulting from increased intracranial pressure (ICP)
- Mental status changes, lethargy, decreased level of consciousness
- Papilledema
- Severe global mental status depression or alteration may signify impending brain herniation
- Manifestations resulting from focal brain injury
- Seizures (35-50%) (Stam 2005)
- Focal neurologic deficits (25-71%) – hemianopsia, contralateral weakness, aphasia etc
Differential Diagnosis
- Ischemic stroke
- Intracranial Hemorrhage (ICH)
- Encephalitis
- Subarachnoid Hemorrhage
- Mass Effect (tumor, abscess etc)
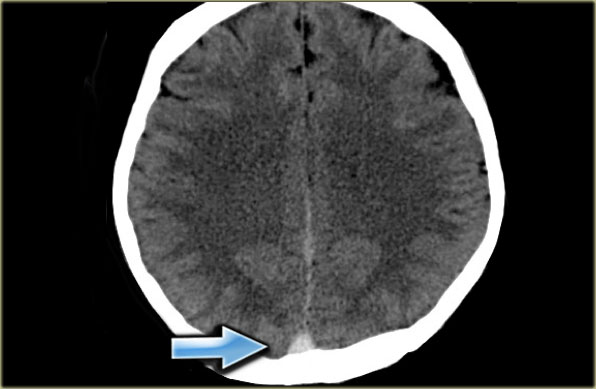
Hyperdensity of Dural Sinus on NCHCT (www.radiologyassistant.nl)
Diagnostics
- Cerebral Angiography
- Historically, diagnostic modality of choice
- Widely replaced by advanced, non-invasive imaging techniques
- Non-Contrast Head CT (NCHCT)
- Often utilized as initial imaging as it can be rapidly obtained and aids in ruling out other possible diagnoses (i.e. ICH)
- Possible findings
- Hyperdensity of a thrombosed sinus or deep vein
- Secondary Findings: brain edema, hemorrhagic conversion (up to 40% of patients (Stam 2005))
- Diagnostic Performance
- Gold standard test: MRI
- Sensitivity ~ 30% (Saposnik 2011)
- Specificity approaches 100% (Linn 2009)
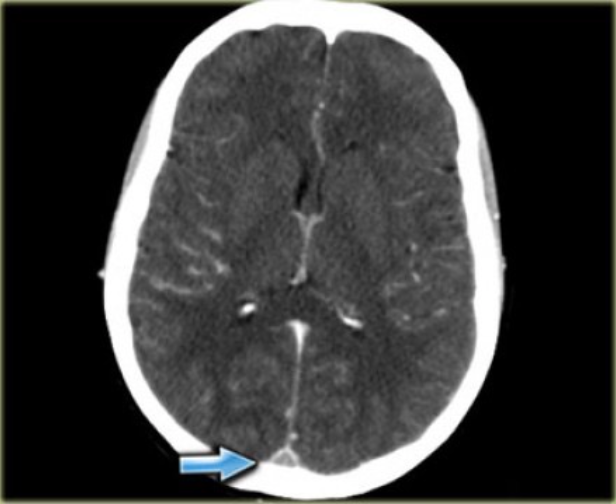
- CT Venogram
- Often added to NCHCT for evaluation
- Small studies have compared CT/CTV to cerebral angiography showing improved diagnostic performance in comparison to CT alone (Sensitivity 95%, Specificity 91%) (Wetzel 1999)
- Accuracy poor for cortical and deep venous thrombosis
- May be reasonable initial test in the absence of MRI availability
- Empty Delta Sign: Triangular area of enhancement with low-attenuating center
- Magnetic Resonance Imaging (MRI) with MR Venography
- Diagnostic modality of choice
- MRI may demonstrate hyperintense signal from thrombosed sinus
- MRV may demonstrate absence of flow to the suspected region
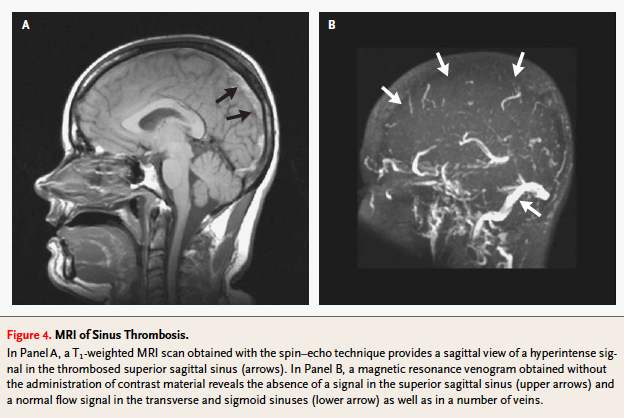
Cerebral Venous Thrombosis on MRI (Stam 2005)
Management
- Due to the rarity of this diagnosis, there is a paucity of controlled trials examining management strategies. The following recommendations are based on consensus statements
- Initial stabilization
- Aimed at preventing or reversing brain herniation
- Manage seizures
- Standard approach with benzodiazepines
- Prophylactic use of antiepileptic drugs may confer more harm than benefit (Saposnik 2011)
- Signs of herniation
- Mannitol 1 gm/kg IV or 3% Hypertonic Saline
- Hyperventilation (short-term only)
- All of the above are temporizing measures only
- Anticoagulation
- Should be considered in all patients without strict contraindications even in the presence of hemorrhagic conversion (Stam 2005, Saposnik 2011)
- Initial anticoagulation (optimal dosing unknown)
- Unfractionated heparin (UFH)
- Bolus: 60-80 units/kg
- Infusion: 12-18 units/kg/hr
- Low molecular weight heparin (LMWH): 1 mg/kg SQ Q12 hours
- Unfractionated heparin (UFH)
- Patients often continued on a vitamin K antagonist for 6-12 months
- Other treatment modalities
- Systemic thrombolytics
- Cather-based interventions (thrombolytics and thrombectomy)
- Surgical: decompressive craniectomy (in markedly increased ICP), hematoma evacuation
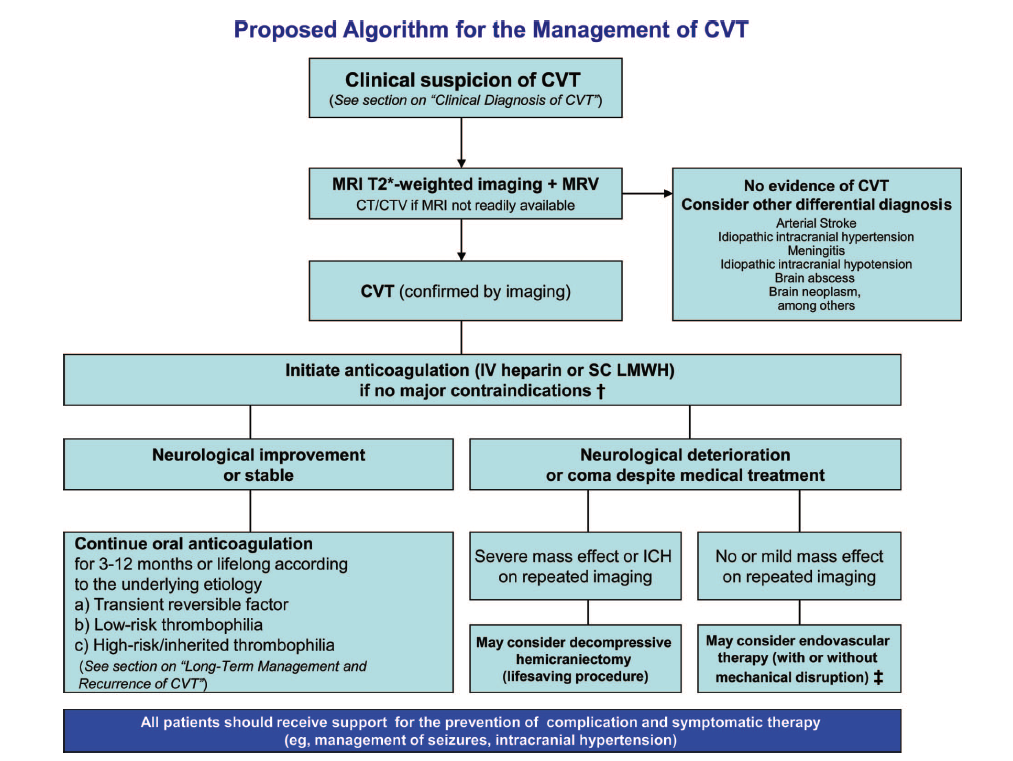
Cerebral Venous Thrombosis Diagnostic Algorithm (Saposnik 2011)
Take Home Points
- CVT is a rare disease that often presents with headache only or non-specific associated symptoms. Consider the diagnosis in patients with indolent, severe headaches, those with exogenous hormone use (or pregnancy) or established thrombophilic states.
- Patients with lethargy, coma, and status epilepticus should prompt consideration for treatment of brain herniation.
- NCHCT is a reasonable first-line test but cannot rule out the disease. MRI/MRV is the current gold standard with CT Venogram as a backup modality if MR is not available.
- Expert consensus recommends initial anticoagulation with heparin (UFH or LMWH) in most patients even in the presence of hemorrhagic conversion.
Read More
Stettler BA. Brain and Cranial Nerve Disorders, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2010, (Ch) 105: p 1409-1420.
References
Linn J et al: Noncontrast CT in deep cerebral venous thrombosis and sinus thrombosis: Comparison of its diagnostic value for both entities. Am J Neuroradiol 2009; 30:728-735. PMID: 19213820
Saposnik G et al. Diagnosis and management of cerebral venous thrombosis. A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011; 42: 1158-92. PMID: 21293023
Stam J. Thrombosis of the Cerebral Veins and Sinuses. NEJM 2005; 352 (17): 1791-1798. PMID: 15858188
Wetzel SG et al. Cerebral veins: comparative study of CT venography with intraarterial
digital subtraction angiography. Am J Neuroradiol. 1999;20: 249–255. PMID: 10094346
Williams DT et al. Cerebral venous thrombosis: hemorrhagic stroke requiring acute heparin anticoagulation. J Emerg Med 2004; 27(3): 295-7. PMID: 15388330
