Definition: A tear in the innermost layer of the aorta (the intima) allowing for blood to dissect between layers of the aortic wall, which may lead to end-organ damage or death.
Epidemiology:
- 10,000 deaths in the US annually
- Incidence 16/100,000 for men, 9/100,000 for women (Milewicz 2011)
- Ratio of Aortic Dissection (AD) to Acute Coronary Syndrome is 1:600
- 22% of cases undiagnosed prior to death (Cline 2012)
Predisposing Factors:
- History of prior dissection
- Hemodynamic Stessors (HTN, cocaine use)
- Connective Tissue Disorders (Marfan Syndrome, Ehlers-Danlos Syndrome)
- Anatomic Abnormalities that cause abnormal flow (bicuspid aortic valve)
- Questionable predisposing factors: PCOS, Pregnancy, Family History
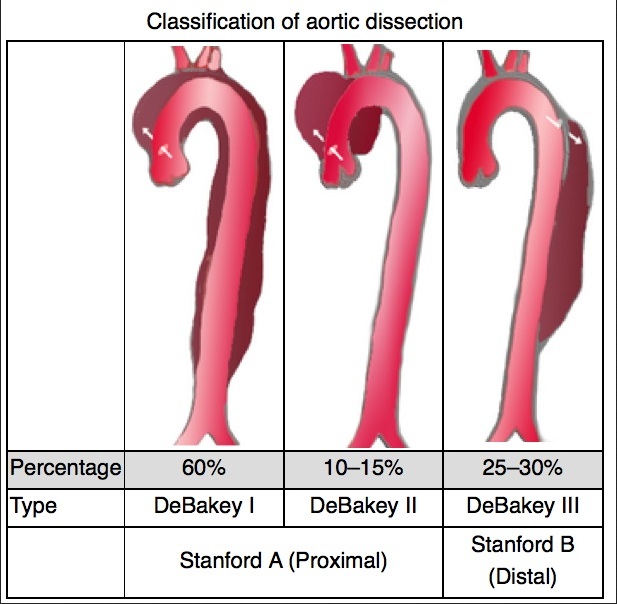
Classification:
- Stanford (More commonly used)
- Type A- Any involvement of the ascending aorta
- Type B- Descending aorta only (distal to the left subclavian artery)
- DeBakey
- Type 1: Involves ascending aorta, aortic arch, and descending aorta
- Type 2: Ascending aorta only
- Type 3: Descending aorta only
AD Variants
- Intramural thrombus- an infarction in the aortic media, most often due to an injury to the vaso vasorum, results in a thrombus within the aortic wall, which may extend or resolve spontaneously. Often a precursor to dissection
- Perforating ulcer- ulcer formation due to atherosclerosis which can lead to intramural thrombus, dissection or aortic perforation (Cline 2012)
History + Physical
- Classic presentation: sudden onset of tearing chest pain radiating to the back, however, dissection may occur anywhere along the aorta and thus the presentation may be broad and mimic other common disorders
- Variant presentations include:
- Patients with symptoms above and below the diaphragm
- Chest pain or back pain + vomiting
- Chest pain or back pain with neurologic findings (may be due to dissection into the carotid arteries)
- Cardiac tamponade
- Any patient that generally “looks bad”
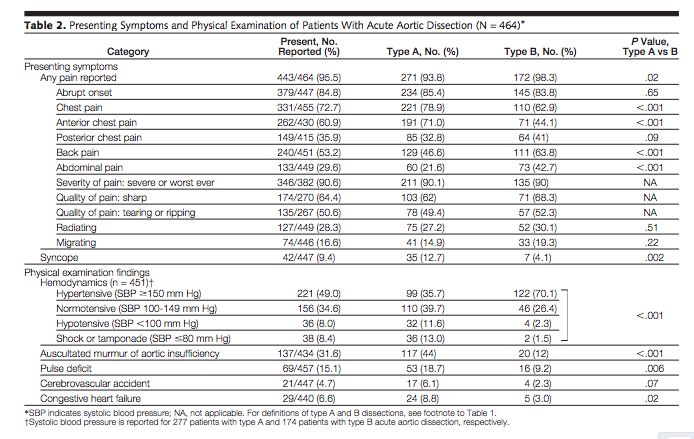
- Only 49% of AD patients have the classic tearing chest pain
- Presenting blood pressure
- Hypertension: 49%
- Normotension: 33%
- Hypotension: 18%
- 4% of AD patients are women. Women diagnosed with AD tend to be older and have higher mortality
- Classic Risk Factors (Hagan 2000)
- 9% of patient’s have Marfan syndrome, these patients are often young
- 72% had a history of HTN
- 9% had prior cardiac surgery
- Physical Examination (Hagan 2000)
- Pulse deficit: Present in only 15%
- Blood pressure differential19%
Diagnostic Testing
- EKG:
- Most changes are non-specific (41.4%) and hard to differentiate from ACS
- >30% of patients have no EKG changes (Hagan 2000)
- CXR: the classic finding is a widened mediastinum (present in 62%) and over 12% of AD patients have no abnormality on x-ray (Hagan 2000)
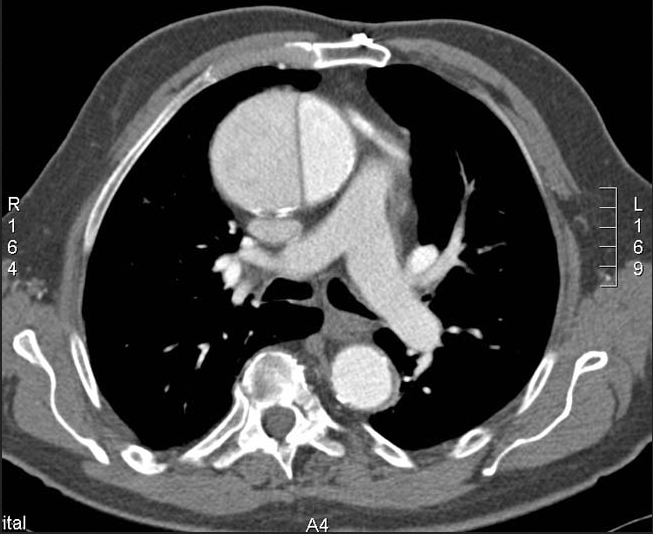
- CT: modality of choice with 100% sensitivity and 98% specificity
- Can identify a false lumen, location of dissection flap, extension into the great vessels, signs of aortic rupture and end-organ damage
- TEE and MRI have similar reliability
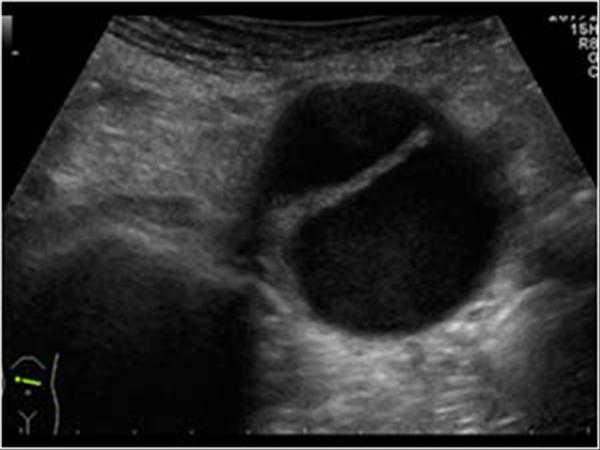
- TTE: may be helpful in identifying cardiac tamponade in an unstable patient
- Tamponade common cause of hypotensive presentation of AD
- ACEP Level B guideline: Do not rely on abnormal bedside TTE result to definitely establish diagnosis of thoracic aortic dissection
- ACEP Level C recommendation: Get a surgical consult or transfer to a higher level of care if TTE is suggestive of dissection (Diercks 2015)
- D-dimer:
- May be helpful if checked within the first 24 hours however due to overlap with other diagnoses may lead to harm (exposure to radiation and cost of imaging) if applied to a large population
- May be negative in young patients and those with short dissection flaps
- Likely to be negative in patients with intramural thrombus as forming clot is not exposed to circulation
- ACEP Level C recommendation: In adult patients with suspected nontraumatic thoracic aortic dissection, do not rel on D-dimer alone to exclude the diagnosis of aortic dissection. (Diercks 2015)
Chest X-Rays in Aortic Dissection
Management
Surgical Management
- Mobilize consultants as early as possible (Cardiothoracic surgery, interventional radiology)
- Mortality increases by 1-2% for every hour from symptom onset to definitive treatment
- Consider pericardiocentesis if patient hypotensive
Medical Management
- Reverse anticoagulation
- Administer analgesia
- Adding fentanyl for pain control can decrease endogenous catecholamines that increase HR and inotropy
- Anti-impulse Therapy
- Goal: Decrease blood pressure and heart rate in order to decrease shear forces on the intima and thus prevent extension of the dissection flap
- No BP or HR goal has demonstrated a reduction in morbidity or mortality, however most sources recommend a systolic blood pressure goal of < 110 mmHg and a heart rate <60bpm
- Medications (Greenwood 2015)
- Beta blocker
- Mechanism of action: negative inotrope/chronotrope
- Esmolol ideal agent: rapid onset and easy to titrate
- Loading Dose: 500 mcg/kg bolus over 1 min (can repeat once)
- Infusion Dose: 50mcg/kg/min, titrate by 50mcg/kg/min q4min (max 300mcg/kg/min)
- Dihydropyridine calcium channel blocker (nicardipine or clevidipine)
- Mechanism of action pure arterial vasodilator (afterload reduction)
- Nicardipine Infusion Dose: 5mg/hr titrate by 2.5 mg/hr q 5min (max 15mg/hr)
- Beta blocker
Take Home Points
- Aortic dissection may occur in any location along the aorta and therefore the range of presentations is broad. Many AD patients do not fit the textbook presentation.
- CT, TEE and MRI are the most reliable methods to diagnose AD
- Once AD is diagnosed, rapid mobilization of consultant services is critical to increase the chance for survival
- Treatment in the ED is focused on lowering blood pressure and heart rate in hypertensive patients until surgical correction can be achieved
References
Cline, D et. al, Tintinalli’s Emergency Medicine Manual, 7e. McGraw-Hill (2012): 160-164.
Diercks DB, et al. Clinical policy: critical issues in the evaluation and management of adult patients with suspected acute nontraumatic thoracic aortic dissection. Ann Emerg Med. 2015 Jan;65(1):32-42.e12. PMID: 25529153.
Greenwood, JC, ed. PressorDex. Irving, TX: Emergency Medicine Residents’ Association; 2015.
Hagan PG, et. al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000 Feb 16;283(7):897-903. PMID: 10685714.
Milewicz DM. Stopping a killer: improving the diagnosis, treatment, and prevention of acute ascending aortic dissections. Circulation. 2011 Nov 1;124(18):1902-4. PMID: 22042924.
Rosman HS, et al. Quality of history taking in patients with aortic dissection. Chest. 1998 Sep;114(3):793-5. PMID: 9743168.
Swaminathan A, Jones MP. Hypertensive Crises. Decision Making in Emergency Critical Care 2015 1st Edition. 208-18.




Nice post – am going to use if for teaching next week – flip the classroom. Thanks!